Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
Abdominal Obesity as a Risk Factor for Stroke in Abuja, Nigeria
GA Onwuegbuzie*, P Alabi and F AbdulaiGA Onwuegbuzie, Department of Medicine, University of Abuja Teaching Hospital, Abuja, Nigeria, Email: gerawele@yahoo.com
Received: 23-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
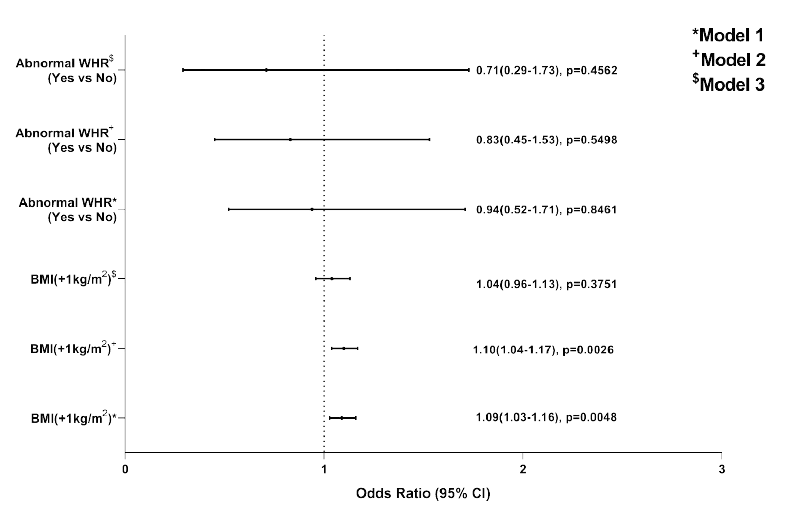
Obesity in Africa has remained a public health concern, which is been fueled by urbanization and its attendant lifestyle changes which include less energy demanding jobs, sedentary lifestyle, and adopting detrimental western eating habits. There are well-established risk factors for stroke; however, the association of obesity with that of stroke is less clear. This study was designed to determine whether abdominal obesity is independently associated with an increased risk of ischemic stroke. It is a case-control study of 113 patients in which a structured questionnaire was administered to consecutive patients admitted into the medical wards. The controls were matched for age and sex from a database with participants of the population-based cohort study. Statistical analysis of data was performed using SAS software (SAS Institute) 9.4. In the study 85% of the patients had hypertension, 50.5% had hypercholesterolemia and 33.6% had diabetes. The BMI was normal for most of the cases (23.3% vs. 76.7% p<0.0001) while the WHR was increased for most of the cases (70.9% vs. 29.1% p<0.0001). The statistical significance shows that WHR was more sensitive in assessing obesity than BMI. The logistic regression analysis, in model 1 unadjusted and model 2 adjusted for sex and age, BMI showed a positive association with risk of stroke (OR 1.10; 95% CI: 1.04-1.17; p: 0.002) this association lost its significance in model 3 after adjusting for diabetes, hypertension and hypercholesterolemia (OR 1.04; 95% CI: 0.96-1.13; p: 0.3751). The results of logistic regression analysis for WHR for model 1, model 2, and model 3 did not show any significance before and after adjustment. In conclusion, abdominal obesity may increase the risk of ischemic stroke through conventional vascular risk factors, but not as an independent risk factor.
Keywords
Obesity, Stroke, Risk factor
Introduction
Obesity has continued to play a significant role in the public health space. The prevalence of overweight or obesity in Africa has remained a public health concern, which is been fueled by urbanization and its attendant lifestyle changes which include less energy demanding jobs, sedentary lifestyle, and adopting detrimental western eating habits. Overweight is seen as a disorder of energy metabolism involving excess adipose tissue stored, which can be described as the imbalance between energy intake and expenditure such that energy is stored in fat cells [1].
Several classifications and definitions of obesity are available but the commonly adopted is the definition by the World Health Organization (WHO), which defines obesity as a Body Mass Index (BMI) of 30 kg/m2 or more [2]. A systematic review showed that the prevalence of overweight and obesity in Nigeria ranged from 20.3%-35.1%, and 8.1%-22.2%, respectively [3].
Stroke is the rapidly developing loss of brain functions due to a disturbance in the cerebral blood vessels. Despite information on the risk factors, stroke remains a neglected disease in Nigeria, as well as specific diagnosis and treatment in the hospitals [3]. There are well-established risk factors for stroke, such as increased blood pressure, increased blood cholesterol, cigarette smoking, carotid stenosis, diabetes mellitus, atrial fibrillation, and valvular heart disease. The association between obesity with many diseases such as type 2 diabetes mellitus, hypertension, dyslipidemia, gall bladder disease, respiratory disease, sleep apnea, and cancer has been well recognized [4-6]. Furthermore, even though the association of obesity with coronary heart disease and myocardial infarction is well recognized, that of stroke is less clear [7-10].
The World Health Organization (WHO) guidelines state that alternative measures that reflect abdominal obesity such as WC, WHR, and Waist-to-Height Ratio (WHtR) are superior to BMI [11]. Previous studies have demonstrated that abdominal obesity which is measured by Waist-to-Hip Ratio (WHR) is more strongly associated with cardiovascular risk than Body Mass Index (BMI) [10,12]. The WHO states that abdominal obesity is defined as a waist-hip ratio above 0.90 for males and above 0.85 for females [11].
The purpose of this study was to determine whether abdominal obesity is independently associated with an increased risk of ischemic stroke among the patients.
Methodology
Study Location and Data Collection
The study was carried out at the University of Abuja Teaching Hospital, a tertiary health center, from March 2017 to July 2020. This a case-control study in which patient structured questionnaires were administered to consecutive patients admitted into the medical wards who met the inclusion criteria for the diagnosis of ischemic stroke in the Neurology Unit, Department of Medicine, University of Abuja Teaching Hospital, Gwagawalada. A total of one hundred and thirteen cases were recruited. Detailed clinical records were incomplete for 10 patients, who were therefore excluded from the analysis. Each index patient was matched with controls without a history of cerebrovascular disease.
All patients who satisfied the WHO clinical criteria for ischemic stroke and had cranial computed tomography or MRI were included in the study
The anthropometric measures (BMI, waist circumference, waist-to-hip ratio) were documented for all study participants. Cases and controls had waist and hip circumference measurements were done in the supine position in those cases that we’re unable to stand. Waist Circumference (WC) was measured at the level of the umbilicus, and hip circumference was measured at the level of the bilateral greater trochanters. Height (in inches) and weight (in kilograms) were measured with a standard scale. About 12% of the patients were too sick for weight measurements and there were no previous medical records of weight for review.
According to international recommendations, BMI is defined as weight in kilograms divided by height in meters squared. In the BMI categories, we distinguished between normal weight (BMI 25.0 kg/m2 and below) and overweight (BMI 25.0 to 29.9 kg/m2), and obesity (BMI >30 kg/m2) [13].
WHR was measured as waist circumference divided by hip circumference. Obese women had WHR>0.85 and obese men WHR>0.95. Threshold categories for waist circumference in men were 94.0 cm (normal weight), 94.0 to 101.9 cm (overweight), and >102.0 cm (obesity). In women they were 80.0 cm, 80.0 to 87.9 cm and >88.0 cm, respectively [14].
Diabetes, hypertension, and hyperlipidemia information were obtained from the medical record of subjects. Diabetes was defined as fasting blood glucose >7mmol/L or on anti-diabetic agents, while hypertension was defined as systolic blood pressure >140 mmHg and/or diastolic blood pressure >90 mmHg, and hyperlipidemia was defined as total serum cholesterol level >5.18 mmol/L.
The controls were matched for age and sex from a database with participants of the population-based cohort study.
The questionnaire was structured to ask questions about: (1) demographic aspects (gender, age, educational level, and occupation) (2) risk factors of a stroke (3) anthropometric data.
Inclusion Criteria
All patients were admitted into the medical ward with a confirmed diagnosis of Ischemic stroke. All patients who had a full clinical assessment for stroke were screened clinically by WHO criteria and verified radiologically by cranial computer tomography scan from March 2017 to July 2020 were included in the study.
Exclusion Criteria
Patients who had space-occupying lesions with neurological deficits or metastatic brain disease and those with Human Immunodeficiency Virus with neurological deficits were excluded from this study. Also excluded from the study were those who were unconscious, had a hemorrhagic stroke, and those people who have other causes of increased abdominal girth like ascites due to any cause, females with pregnancy, or an intra-abdominal mass.
Data Analysis
Statistical analysis of data collected was performed using SAS software (SAS Institute) 9.4. Data collected were analyzed by frequency, mean, standard deviation, and chi-square test. For all statistical tests, the threshold of significance is fixed at 5%. p-value>0.05 indicates none significant results. p-value<0.05 indicates significant results.
Multiple logistic regression models for matched case-control data were used to calculate the Odds Ratio (OR) and 95% Confidence Interval (CI) for BMI and WHR and ischemic stroke. Adjusted ORs were calculated after adjusting for potential confounding factors (clinical history of hypertension, diabetes, and hypercholesterolemia) and age and sex were evaluated.
Results
A total of 113 patients with ischemic stroke were evaluated. Of these cases 53.1% were females and 46.9% were males. Table 1 shows the demographic characteristic and distribution of the study population (cases and control) stratified by sex.
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Number (%) | Control 59 (49.6) |
Cases 60 (50.4) |
p-value | Control 52 (49.5) |
Cases 53 (50.5) |
p-value |
| Age group | ||||||
| ≤ 30years | 4 (6.6) | 3 (5.0) | 0.901 | 2 (3.9) | 1 (1.9) | 0.4196 |
| 31-60 years | 26 (44.1) | 28 (46.7) | 0.7759 | 23 (44.2) | 18 (34.0) | 0.2809 |
| >60 years | 29 (49.2) | 29 (48.3) | 0.9288 | 27 (51.9) | 34 (64.2) | 0.2042 |
| Lifestyle | ||||||
| Cigarette smoking | 0 (0.0) | 3 (5.1) | 0.0819 | 2 (3.9) | 10 (18.9) | 0.0171 |
| Alcohol intake | 16 (27.6) | 8 (13.3) | 0.0545 | 23 (45.1) | 26 (49.1) | 0.686 |
| Marital Status | ||||||
| Single | 5 (8.5) | 5 (8.3) | 0.9778 | 4 (7.7) | 4 (7.7) | 0.9999 |
| Married | 42 (71.2) | 44 (73.3) | 0.7937 | 46 (88.5) | 44 (84.6) | 0.5656 |
| Separated/divorced | 1 (1.7) | 1 (1.7) | 0.9904 | 1 (1.9) | 3 (5.8) | 0.9904 |
| Widowed | 11 (18.6) | 10 (16.7) | 0.7772 | 1 (1.9) | 1 (1.9) | 0.9999 |
| Educational Status | ||||||
| Uneducated | 1 (1.7) | 4 (6.7) | 0.1765 | 4 (7.7) | 0 (0.0) | 0.0395 |
| Informal | 19 (32.2) | 2 (3.3) | <0.0001 | 7 (13.5) | 1 (1.9) | 0.0254 |
| Primary | 8 (13.6) | 9 (15.0) | 0.8223 | 8 (15.4) | 0 (0.0) | 0.003 |
| Secondary | 14 (23.7) | 19 (31.7) | 0.3335 | 11 (21.2) | 18 (34.0) | 0.1422 |
| Tertiary | 17 (28.8) | 23 (38.3) | 0.2717 | 21 (40.4) | 34 (64.2) | 0.0148 |
| Occupational Status | ||||||
| Civil servant | 7 (11.9) | 14 (23.3) | 0.1008 | 11 (22.5) | 26 (49.1) | 0.0052 |
| Private servant | 4 (6.8) | 7 (11.7) | 0.3574 | 10 (20.4) | 6 (11.3) | 0.2074 |
| Self-employed | 37 (62.7) | 15 (25.0) | <0.0001 | 26 (53.1) | 16 (30.2) | 0.019 |
| Student | 2 (3.4) | 1 (1.7) | 0.5488 | 0 (0.0) | 1 (1.9) | 0.3339 |
| Unemployed | 9 (15.3) | 23 (38.3) | 0.0045 | 2 (4.1) | 4 (7.6) | 0.4574 |
Table 2 shows the cardiovascular risk factors for stroke in cases. In the study 85% of the patient had hypertension, 50.5% had hypercholesterolemia and 33.6 % had diabetes. 22% had a family history of a relative that has had a stroke.
| All | Men | Women | |
|---|---|---|---|
| Number (%) | 113 | 53 (46.9) | 60 (53.1) |
| Heart disease | 21 (19.1) | 9 (17.7) | 12 (20.3) |
| Hypertension | 96 (85.0) | 48 (90.6) | 48 (80.0) |
| Hypercholesterolemia | 54 (50.5) | 25 (50.0) | 29 (50.9) |
| Diabetes | 38 (33.6) | 15 (28.3) | 23 (38.3) |
| Family history of stroke | 24 (22.0) | 12 (24.5) | 12 (20.0) |
Table 3 revealed the anthropometric characteristics of cases and control stratified by gender.
| Number (%) | Control | Cases | p-value |
|---|---|---|---|
| Mean ± SD | |||
| Waist Cir | 87.7 ± 11.9 | 94.8 ± 17.4 | 0.0005 |
| Hip Cir | 96.8 ± 12.4 | 102.6 ± 12.9 | 0.0011 |
| BMI | 25.3 ± 6.3 | 26.8 ± 4.8 | 0.0665 |
| WHR | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.5735 |
| Median (IQR) | |||
| Waist Cir | 87.0 (17.0) | 93.5 (17.0) | 0.0001 |
| Hip Cir | 95.0 (18.0) | 101.0 (15.0) | 0.0002 |
| BMI | 24.0 (7.0) | 26.0 (5.9) | 0.0051 |
| WHR | 0.9 (0.1) | 0.9 (0.1) | 0.4105 |
The mean waist circumference for control and cases (87.7 ± 11.9 vs. 94.8±17.4; p=0.0005), while the hip circumference (96.8 ± 12.4 vs. 102.6 ± 12.9; p=0.0011). However, the Waist-to-Hip Ratio (WHR) did not show any statistical significance among control and cases (0.9 ± 0.1 vs. 0.9 ± 0.1; p=0.5735), as well as BMI (25.3 ± 6.3 vs. 26.8 ± 4.8; p=0.0665).
The result of the median waist circumference for control and cases (87.0 vs. 93.5; p=0.0001), The hip circumference (98.0 vs. 101.1; p=0.0002). However, the Waist-to-Hip Ratio (WHR) did not show any statistical significance among control and cases (p=0.4105), while the BMI (24.0 vs. 26.0; p=0.0051).
Table 4 shows the prevalence of obesity among cases with stroke. The BMI showed that most of the cases were normal (23.3% vs. 76.7%; p<0.0001) while the WHR showed that most of the cases were not normal (70.9% vs. 29.1%; p<0.0001). The statistical significance shows that WHR was more sensitive in assessing obesity than BMI.
| Number (%) | p-value | ||
|---|---|---|---|
| BMI (n=90) | BMI ≥ 30kg/m2 | 21 (23.3) | <0.0001 |
| BMI<30kg/m2 | 69 (76.7) | ||
| WHR (n=103) | Abnormal WHR | 73 (70.9) | <0.0001 |
| Normal WHR | 30 (29.1) | ||
Figure 1 shows the results of logistic regression analysis, in model 1 unadjusted and then model 2 adjusted for sex and age, BMI showed a positive association with risk of stroke (OR 1.10; 95% CI: 1.04-1.17; p: 0.002) this association lost its significance in model 3 after adjusting for diabetes, hypertension and hypercholesterolemia (OR 1.04; 95% CI: 0.96-1.13; p: 0.3751).
The results of logistic regression analysis for WHR for model 1, model 2, and model 3 did not show any significance before and after adjustment.
Discussion
This study assessed the relationship between obesity as a risk factor for stroke among cases and controls. Previous works done have demonstrated that there is an increased atherosclerotic and cardiovascular risk in the association of abdominal obesity [15,16]. Furthermore, an increased prevalence of cardiovascular risk factors has been seen with the increase in abdominal obesity by other researchers [17-21]. In other studies, obese people have been found to have an increased risk of developing ischemic stroke with a person with a 100 cm waist size or more having a risk of 10% [22].
Our study shows a slight preponderance of females among the study population, with total females among the patients as 53.1% while the males were 46.9%. The prevalence of stroke was more in the age group greater than 60 years. The educational characteristics show 50.5 % of the patient had tertiary education and 32.8 % had secondary education. Although the educational level and age have been reported to be associated with knowledge of stroke risk factors [23-25]. It is important to note that about 80% of the cases had at least secondary education, which was a predictor of stroke knowledge.
High blood pressure was the most frequently identified risk factor in our study as in other studies [26,27]. Our study found hypercholesterolemia and diabetes mellitus in 54% and 38% respectively. This finding in our study agrees in part with previous works done in our center which showed a prevalence of hypercholesterolemia to be 45% and diabetes to be 33% [28].
Our study, therefore, sought to review the prevalence of obesity among stroke patients. Those with abnormal WHR constituted 70.9% (p<0.0001). Abnormal BMI was found in twenty-three percent of the patients. This is in support of previous work done which had a lower predictive value of different markers of adiposity Where BMI and WHR were compared as a risk factor among patients with stroke [29]. Furthermore because of a loss of lean body mass with age, weight or BMI can decrease with age [29,30]. What this means is that WHR may be a more useful method to assess abdominal fat, however in clinical practice WHR is a more difficult measure to standardize when compared to measurement of BMI. Waist circumference which is an indicator of abdominal obesity when used alone instead of WHR is not a good predictor of stroke as demonstrated in previous works [9,29].
Abdominal obesity may increase the risk of ischemic stroke through conventional vascular risk factors, but our study did not demonstrate an effect independent of other cofounders. The odds ratio of waist to hip ratio and BMI were 0.94 and 1.09 respectively. After the adjustment for age and sex the p-value was still significant for BMI (0.0026) however after adjustment for diabetes, hypertension, and hypercholesterinemia the significance was lost. Our result does not support previous studies which were associated with the risk of ischaemic stroke with a p-value of 0.01(OR 1.57; CI=1.28-1.94) [31]. However, in the case of the waist to hip ratio after adjustment for age and sex as well as diabetes, hypertension, and hypercholesterinemia the significance was lost. In some cohort studies, WHR was no longer an independent risk factor for stroke after adjustment for hypertension and blood lipid levels or diabetes [32,33]. In other studies, there was a significant relationship between abdominal obesity and BMI ischemic stroke, with the probability of abdominal obesity for ischemic stroke (1.75), and BMI (0.794) [34]. Despite the loss insignificance after adjustment of more risk factors, available evidence suggests that those markers remain important as shown in other studies [35].
In our study, we did not consider the pre-morbid patient WHR or BMI which may in part be an explanation for this finding in addition to the different study designs applied and populations studied. It is also important to note that abdominal obesity may indirectly contribute to the incidence of ischemic stroke by influencing other well-recognized risk factors. Furthermore, abdominal obesity may increase the risk of ischemic stroke through other mechanisms like insulin resistance or metabolic syndrome. It is worth noting that our study could not demonstrate an effect independent of these mechanisms and other conventional vascular risk factors.
Available evidence suggests that abdominal obesity is related not only to endothelial dysfunction which may be an early marker of atherosclerosis, but also disturbances associated with blood flow and atherogenesis, which includes hyper-viscosity of blood, hyper-fibrinogenemia reduction in erythrocyte aggregability and deformability, and platelet activation [36-38].
Conclusion
We acknowledge the limitations in our study being a single-centered hospital-based study but still highlight the importance of WHR as a determinant of obesity in stroke as a risk factor. Despite these limitations, the argument still favours adding WHR as a measurement to vascular risk assessments.
In conclusion, this study highlights the need to increase public awareness about stroke risk factors including obesity. Even though abdominal obesity was not found as an independent risk factor for stroke, it contributes to the risk of stroke through the conventional risk factors.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Heymsfield, Steven B., and Thomas A. Wadden. "Mechanisms, pathophysiology, and management of obesity." New England Journal of Medicine, Vol. 376, No. 3, 2017, pp. 254-66.
- Status, Physical. "WHO Technical Report Series 854." World Health Organization, 1995.
- Chukwuonye, Innocent Ijezie, et al. "Prevalence of overweight and obesity in adult Nigerians-A systematic review." Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy, Vol. 6, 2013, pp. 43-47.
- Burton, B. T., et al. "Health implications of obesity: An NIH Consensus Development Conference." International Journal of Obesity, Vol. 9, No. 3, 1985, pp. 155-70.
- Must, Aviva, et al. "The disease burden associated with overweight and obesity." JAMA, Vol. 282, No. 16, 1999, pp. 1523-29.
- National Heart, et al. "The practical guide: identification, evaluation, and treatment of overweight and obesity in adults." The Institute, 2000.
- Hubert, Helen B., et al. "Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study." Circulation, Vol. 67, No. 5, 1983, pp. 968-77.
- Fraser, Gary E., et al. "Effects of traditional coronary risk factors on rates of incident coronary events in a low-risk population. The Adventist Health Study." Circulation, Vol. 86, No. 2, 1992, pp. 406-13.
- Prineas, Ronald J., Aaron R. Folsom, and Susan A. Kaye. "Central adiposity and increased risk of coronary artery disease mortality in older women." Annals of Epidemiology, Vol. 3, No. 1, 1993, pp. 35-41.
- Rimm, Eric B., et al. "Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men." American Journal of Epidemiology, Vol. 141, No. 12, 1995, pp. 1117-27.
- World Health Organization. "Waist circumference and waist-hip ratio: Report of a WHO expert consultation, Geneva, 8-11 December 2008." 2011.
- Yusuf, Salim, et al. "Obesity and the risk of myocardial infarction in 27 000 participants from 52 countries: A case-control study." The Lancet, Vol. 366, No. 9497, 2005, pp. 1640-49.
- Consultation, W. H. O. "Obesity: Preventing and managing the global epidemic." World Health Organization technical report series, 2000, pp. 1-253.
- Lean, M. E. J., T. S. Han, and C. E. Morrison. "Waist circumference as a measure for indicating need for weight management." BMJ, Vol. 311, No. 6998, 1995, pp. 158-61.
- Northern Manhattan Stroke Study Collaborators, et al. "Stroke incidence among white, black, and Hispanic residents of an urban community: The Northern Manhattan Stroke Study." American Journal of Epidemiology, Vol. 147, No. 3, 1998, pp. 259-68.
- Sacco, Ralph L., et al. "The protective effect of moderate alcohol consumption on ischemic stroke." JAMA, Vol. 281, No. 1, 1999, pp. 53-60.
- Folsom, Aaron R., et al. "Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women." Stroke, Vol. 21, No. 5, 1990, pp. 701-06.
- Blair, Dorothy, et al. "Evidence for an increased risk for hypertension with centrally located body fat and the effect of race and sex on this risk." American Journal of Epidemiology, Vol. 119, No. 4, 1984, pp. 526-40.
- Folsom, Aaron R., et al. "Relation of body fatness and its distribution to cardiovascular risk factors in young blacks and whites: The role of insulin." American Journal of Epidemiology, Vol. 130, No. 5, 1989, pp. 911-24.
- Gillum, Richard F. "The association of body fat distribution with hypertension, hypertensive heart disease, coronary heart disease, diabetes and cardiovascular risk factors in men and women aged 18-79 years." Journal of Chronic Diseases, Vol. 40, No. 5, 1987, pp. 421-28.
- Daniels, Stephen R., et al. "Association of body fat distribution and cardiovascular risk factors in children and adolescents." Circulation, Vol. 99, No. 4, 1999, pp. 541-45.
- Zhong, Chong Ke, et al. "Measures of abdominal adiposity and risk of stroke: A dose-response meta-analysis of prospective studies." Biomedical and Environmental Sciences, Vol. 29, No. 1, 2016, pp. 12-23.
- Zeng, Ying, et al. "Knowledge of stroke warning signs and risk factors among patients with previous stroke or TIA in China." Journal of Clinical Nursing, Vol. 21, No. 19pt 20, 2012, pp. 2886-95.
- Sundseth, Antje, et al. "Factors related to knowledge of stroke symptoms and risk factors in a Norwegian stroke population." Journal of Stroke and Cerebrovascular Diseases, Vol. 23, No. 7, 2014, pp. 1849-55.
- Shravani, K., et al. "Risk factor assessment of stroke and its awareness among stroke survivors: A prospective study." Advanced Biomedical Research, Vol. 4, 2015.
- Pancioli, Arthur M., et al. "Public perception of stroke warning signs and knowledge of potential risk factors." JAMA, Vol. 279, No. 16, 1998, pp. 1288-92.
- Kim, Jong S., and Sung S. Yoon. "Perspectives of stroke in persons living in Seoul, South Korea: A survey of 1000 subjects." Stroke, Vol. 28, No. 6, 1997, pp. 1165-69.
- Onwuegbuzie, Gerald A, and RengRifkatu S. "Serum lipid profile of patients with ischaemic stroke in a Tertiary Centre in Nigeria." IOSR Journal of Dental and Medical Sciences (IOSR-JDMS), Vol. 15, No. 11, 2016, pp. 60-64.
- Walker, Susan P., et al. "Body size and fat distribution as predictors of stroke among US men." American Journal of Epidemiology, Vol. 144, No. 12, 1996, pp. 1143-50.
- Flegal, Katherine M., et al. "Overweight and obesity in the United States: Prevalence and trends, 1960-1994." International Journal of Obesity, Vol. 22, No. 1, 1998, pp. 39-47.
- Mitchell, Andrew B., et al. "Obesity increases risk of ischemic stroke in young adults." Stroke, Vol. 46, No. 6, 2015, pp. 1690-92.
- Lapidus, Leif, et al. "Distribution of adipose tissue and risk of cardiovascular disease and death: A 12 year follow up of participants in the population study of women in Gothenburg, Sweden." British Medical Journal, Vol. 289, No. 6454, 1984, pp. 1257-61.
- Larsson, B. K. L. L. P. G., et al. "Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913." British Medical Journal, Vol. 288, No. 6428, 1984, pp. 1401-04.
- Laily, S. R., et al. "Abdominal obesity as a risk factor of ischemic stroke incidence in Lamongan distric, Indonesia." Malaysian Journal of Medicine and Health Sciences, Vol. 16, No. 6, 2020, pp. 88-93.
- Suk, Seung-Han, et al. "Abdominal obesity and risk of ischemic stroke: The Northern Manhattan Stroke Study." Stroke, Vol. 34, No. 7, 2003, pp. 1586-92.
- Arcaro, G., et al. "Body fat distribution predicts the degree of endothelial dysfunction in uncomplicated obesity." International Journal of Obesity, Vol. 23, No. 9, 1999, pp. 936-42.
- Solerte, S. B., et al. "Hyperviscosity and microproteinuria in central obesity: Relevance to cardiovascular risk." International Journal of Obesity, Vol. 21, No. 6, 1997, pp. 417-23.
- Davì, Giovanni, et al. "Platelet activation in obese women: Role of inflammation and oxidant stress." JAMA, Vol. 288, No. 16, 2002, pp. 2008-14.