Brief Report - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 8
An Overview and Insights of Polycystic Ovarian Syndrome and Infertility
Lisy Prabu*Lisy Prabu, 4th Year MBBS - Tianjin Medical University, Tianjin, China, Email: lisyvima27@gmail.com
Received: 24-Jul-2023, Manuscript No. ijmrhs-23-107891; Editor assigned: 26-Jul-2023, Pre QC No. ijmrhs-23-107891(PQ); Reviewed: 13-Aug-2023, QC No. ijmrhs-23-107891(Q); Revised: 27-Aug-2023, Manuscript No. ijmrhs-23-107891(R); Published: 31-Aug-2023
Abstract
15% of couples struggle with infertility. A thorough medical history must be taken before conducting a physical, gynecological, and endocrine examination on a female patient with infertility. Several tests, including those assessing ovarian function and reserve, searching for uterine anomalies, and measuring tubal permeability, will be used to identify the causes of infertility. Polycystic Ovarian Syndrome (PCOS) is a prevalent gynecological-endocrine condition that affects 7% to 15% of women of reproductive age and is the main cause of infertility. The effectiveness of behavioral, medicinal, and surgical therapies to increase fertility in women with PCOS has been studied. It is crucial to make lifestyle changes (quit smoking, start exercising, and, if required, lose weight). In the absence of additional female or male factors contributing to infertility, clomiphene citrate remains the first line of medical therapy for women with PCOS. Metformin should not be used solely to treat infertility unless a metabolic disorder is present, along with novel medications like myoinositol. When medical therapy fails, surgical procedures designed to increase ovulation and pregnancy rates are an option. In the management of infertility, ovarian drilling through laparoscopy or transvaginal hydro-laparoscopy is becoming more common. For PCOS, In vitro maturation and conception still stand as the third line of defense.
Keywords
PCOS, Infertility, Laparoscopy
Introduction
Polycystic Ovarian Syndrome (PCOS), an endocrine and reproductive condition, affects 7% to 15% of women in their reproductive age. It was first described by Stein and Leventhal in 1935. The etiology of PCOS is complicated and still disputed, involving genetic, environmental, and behavioral factors. The three Rotterdam criteria, collectively describing PCOS, are oligo-anovulation, clinical or biological hyperandrogenism, and micro polycystic syndrome (characterized by ovarian volume >10 ml and/or the presence of more than 12 follicles in the ovary) [1].
Patients with various degrees of hyperandrogenism (hirsutism, seborrhea, acne), malfunction of the menstrual cycle, obesity, and infertility will visit a doctor if they have PCOS [2].
The delay in referral to a specialist, frequently for infertility, has been well-documented in the literature and is one explanation for a delayed diagnosis.
This article's goal is to provide a summary of the many solutions that might help PCOS patients become more fertile. A special focus will be placed on ovarian drilling, a surgical procedure that is less frequently utilized but has certain extra benefits.
Infertility
Evaluation in PCOS patients: After 12 months without conceiving, evaluation of infertility (or subfertility) is advised in couples who have frequent sex (2 or 3 times per week).
PCOS is the first cause of female infertility but the definite diagnosis should be given after exclusion of other etiologies of infertility such as other endocrine disorders (thyroid dysfunction, hyperprolactinemia, congenital adrenal hyperplasia, Cushing syndrome, premature ovarian insufficiency), anatomical dysfunctions (endometriosis, pelvic inflammatory diseases) or iatrogenic causes (surgery, chemotherapy, radiations) [3].
The patient’s personal medical and surgical as well as familial history, followed by a complete physical and gynecological examination is mandatory when exploring infertility. A thorough table with the infertility factors to search can be found in the supplemental data. Additional diagnostic tests including blood samples, ultrasonography and hysteroscopy among others are recommended [4].
Anti-Müllerian Hormone (AMH) is a useful test in the evaluation of infertility. It is produced by granulosa cells of early follicles and helps to evaluate the ovarian reserve. Because its production is gonadotrophin-independent, AMH levels remain consistent during the menstrual cycle. The antral follicle count, endometrial thickness, and uterine abnormality (polyps, myomas, and congenital deformity) are all assessed by Transvaginal Ultrasound (TVUS) [5].
Treatment
Non-pharmacologic measures remain the first line and the most effective in the treatment of infertility. We already know the positive effects of clomiphene citrate letrozole and gonadotropins in the treatment of infertility in PCOS. Myo-inositol and ovarian drilling are new lines of therapeutic and will be discussed in this review. This review includes articles until March 2021.
Non-pharmacological measures: Lifestyle changes are the first line of treatment for women with PCOS. In all cases, smoking should be ceased and physical exercise encouraged. Weight loss is recommended in overweight and obese women [6].
Additionally, the ovulation-inducing drugs' effects are improved by this weight reduction. Along with the established metabolic advantages, weight reduction in obese women with PCOS increases the rate of conception. When BMI is greater than 35 kg/m2 and lifestyle adjustments attempted for more than a year have failed, bariatric surgery may be considered [7].
According to a meta-analysis, monthly irregularities and hirsutism in obese PCOS patients following bariatric surgery were resolved in 96% of cases, and there was a substantial drop in testosterone levels. Bariatric surgery does not, as of now, appear to increase the conception rate in women with PCOS, according to substantial data. Additionally, vitamin deficiency, intestinal imprisonment in the Petersen space, and surgical consequences should not be disregarded [8].
Metformin: Off-label usage of metformin (an insulin sensitizer) has long been regarded as the first-line therapy for PCOS because of the crucial role that insulin resistance plays in PCOS. According to several studies, women with PCOS who take metformin (alone or in combination with Clomiphene) have longer ovulatory periods. Therefore, the current recommendations do not support the use of metformin for ovulation induction and restrict its usage to type 2 diabetes and insulin resistance in PCOS [9].
Treatment Already Confirmed
First line treatment:
• Clomiphene citrates: Women with PCOS experiencing infertility continue to get Clomiphene Citrate (CC) as their go-to ovulation induction medication. A negative feedback mechanism causes CC, an anti-estrogen treatment, to inhibit estrogen receptors in the brain and stimulate follicular growth. Therefore, the current recommendations do not support the use of metformin for ovulation induction and restrict its usage to type 2 diabetes and insulin resistance in PCOS.
• Letrozole: The class of aromatase inhibitors includes letrozole. Lower E2 levels are the effect of aromatase inhibitors. This significantly lowers the possibility t of developing numerous follicles. One of the key benefits of letrozole for CC is this. Another benefit is that letrozole has no negative effects on endometrial thickness or cervical mucus since it does not interfere with endometrial estrogen receptors. Letrozole is still advised as a second-line therapy for women with CC resistance or failure that does not have another infertility cause, though [10].
Second-line therapeutic options (gonadotropin therapy): A second-line therapeutic option is gonadotropin therapy associated with timed intercourse. For women with PCOS, all recommendations now agree to use a lowdose step-up regimen to prevent Ovarian Hyperstimulation Syndrome (OHSS) and multiple pregnancies. The high number of antral follicles in women with PCOS predisposes them to develop OHSS.
The third line of treatment (In vitro fertilization and In vitro maturation): When the second-line treatment options have failed, more complex therapies should be proposed, mainly In vitro Fertilization (IVF) and, more recently, In vitro Maturation (IVM). IVF protocols use the combined action of gonadotropins with gonadotropinreleasing hormone agonist and antagonist. Complications of this technique are multiple pregnancies and OHSS. After ovulation, multiple luteinized cysts are present within the ovaries leading to larger ovaries with higher vascular permeability resulting in a third space because of the shift of the fluids. Estrogens, progesterone and local cytokines are released as a vascular endothelial growth factor which encourages vascular hyperpermeability. The creation of a third space can lead to hypovolemia, renal insufficiency, and death. Women with PCOS are predisposed to develop OHSS because of the high number of antral follicles [11].
New Treatment
• Myoinositol
• Ovarian drilling
Technique: Laparoscopic ovarian cautery is performed with a traditional endoscope and two additional trocars. The whole length of the unipolar needle electrode is inserted into the ovary with a setting of 40 W for 4 sec to 5 sec. The laparoscopic technique is the recommended procedure for ovarian drilling. Transvaginal hydrolaparoscopy is performed with saline solution in the peritoneal cavity. The endoscope has an angle of 30ÃÂ?? and permits examination of the entire pelvic cavity. Salpingoscopy with fallopian tube and fimbriae inspection can also be performed by Transvaginal Laparoscopy (THL) Ovarian drilling carries the same hazards as any surgical operation, including the possibility of adhesion formation. Laparoscopy vs. THL as the procedure of choice may have an impact on safety. Giampaolino et al contrasted the advantages of THL with laparoscopy [12].
The outcomes demonstrated that THL is quicker, decreases adhesions, and is more patient-tolerated (reduced postoperative discomfort). The installation of saline solution, the shorter length, the use of bipolar diathermy, and the decrease in bleeding owing to less manipulation of the ovaries than during a laparoscopy may be the reasons behind these advantages. If this occurs, it is often treated with conservative measures and antibiotics. The integrity of the peritoneum will be confirmed by a second-look laparoscopy [13-15].
Mechanism of Action
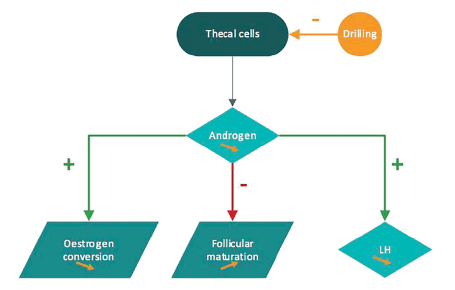
The mechanism of action of ovarian drilling is still poorly understood. It seems that ovarian drilling impairs local androgen synthesis and reduces intraovarian androgen level which decreases the inhibitory effect on follicular maturation. Lower levels of androgens diminish the peripheral conversion of androgen to estrogen and decrease the positive feedback on LH secretion. Recruitment of new follicles is permitted spontaneously or with exogenous FSH stimulation (Figure 1).
Conclusion
PCOS is a frequent syndrome and the most frequent cause of infertility. PCOS is defined as a syndrome with at least two of three of the Rotterdam criteria. A complete evaluation of the infertility is needed to exclude other causes of infertility. PCOS treatment is still controversial but three lines of therapies were discussed. The first line of treatment remains lifestyle modifications and bariatric surgery-associated or not with metformin and myoinositol. Clomiphene citrate and letrozole are considered also as the first line of treatment. Gonadotrophin therapy and ovarian drilling are the second line of treatment. Nevertheless, the place of transvaginal hydrolaparoscopic ovarian drilling is still not well clarified. Further studies are necessary to encourage this technique. If the patient is still resistant to those therapies, a third line of treatment is proposed as In vitro fertilization and In vitro maturation.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Practice Committee of the American Society for Reproductive Medicine. "Definitions of infertility and recurrent pregnancy loss: a committee opinion." Fertility and sterility, Vol. 99, No. 1, 2013, p. 63.
Google Scholar Crossref - Pasquali, Renato, et al. "Clinical and hormonal characteristics of obese amenorrheic hyperandrogenic women before and after weight loss." The Journal of Clinical Endocrinology & Metabolism, Vol. 68, No. 1, 1989, pp. 173-9.
Google Scholar Crossref - Thessaloniki ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. "Consensus on infertility treatment related to polycystic ovary syndrome." Human reproduction, Vol. 23, No. 3, 2008, pp. 462-77.
Google Scholar Crossref - Gibson-Helm, Melanie E., et al. "Women’s experiences of polycystic ovary syndrome diagnosis." Family practice, Vol. 31, No. 5, 2014, pp. 545-9.
Google Scholar Crossref - Melo, Anderson Sanches, Rui Alberto Ferriani, and Paula Andrea Navarro. "Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice." Clinics, Vol. 70, 2015, pp. 765-9.
Google Scholar Crossref - Sahmay, Sezai, et al. "Serum AMH levels and insulin resistance in women with PCOS." European Journal of Obstetrics & Gynecology and Reproductive Biology, Vol. 224, 2018, pp. 159-64.
Google Scholar Crossref - Artini, Paolo Giovanni, et al. "PCOS and pregnancy: a review of available therapies to improve the outcome of pregnancy in women with polycystic ovary syndrome." Expert review of endocrinology & metabolism, Vol. 13, No. 2, 2018, pp. 87-98.
Google Scholar Crossref - Kiddy, Deborah S., et al. "Improvement in endocrine and ovarian function during dietary treatment of obese women with polycystic ovary syndrome." Clinical endocrinology, Vol. 36, No. 1, 1992, pp. 105-11.
Google Scholar Crossref - Balen, Adam H., et al. "Should obese women with polycystic ovary syndrome receive treatment for infertility?." Bmj, Vol. 332, No. 7539, 2006, pp. 434-5.
Google Scholar Crossref - Crosignani, Pier Giorgio, et al. "Overweight and obese anovulatory patients with polycystic ovaries: parallel improvements in anthropometric indices, ovarian physiology and fertility rate induced by diet." Human reproduction, Vol. 18, No. 9, 2003, pp. 1928-32.
Google Scholar Crossref - Malik, Shaveta M., and Michael L. Traub. "Defining the role of bariatric surgery in polycystic ovarian syndrome patients." World Journal of Diabetes, Vol. 3, No. 4, 2012, p. 71.
Google Scholar Crossref - Escobar-Morreale, Hector F., et al. "Prevalence of ‘obesity-associated gonadal dysfunction’in severely obese men and women and its resolution after bariatric surgery: a systematic review and meta-analysis." Human Reproduction Update, Vol. 23, No. 4, 2017, pp. 390-408.
Google Scholar Crossref - Mahawar, Kamal, Chetan Parmar, and Yitka Graham. "One anastomosis gastric bypass: key technical features, and prevention and management of procedure-specific complications." Minerva Chirugia, Vol. 74, No. 2, 2018, pp. 126-36.
Google Scholar Crossref - Arterburn, David E., et al. "Benefits and risks of bariatric surgery in adults: a review." Jama, Vol. 324, No. 9, 2020, pp. 879-87.
Google Scholar Crossref - Morley, Lara C., et al. "Insulinâ?sensitising drugs (metformin, rosiglitazone, pioglitazone, Dâ?chiroâ?inositol) for women with polycystic ovary syndrome, oligo amenorrhoea and subfertility." Cochrane Database of Systematic Reviews, Vol. 11, 2017.
Google Scholar Crossref