Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 3
Anesthetic Management of Adult diaphragmatic Hernia for Laparoscopic Repair: A Case Report
Kalpana Kulkarni1*, Ila MS and Vishnu TejaKalpana Kulkarni, Department of Anaesthesiology, DY Patil Medical College Hospital, Kolhapur, Maharashtra, India, Tel: 9822065665, Email: drkrk29@gmail.com
Received: 10-Feb-2021 Accepted Date: Mar 24, 2021 ; Published: 31-Mar-2021
Abstract
Congenital Diaphragmatic Hernia (CDH) occurs in about 1 in 3000 births. It usually presents at birth because of the defects in the foramen of Bochdalek or Morgagni in the postero-lateral or anterior part of the diaphragm with an incidence of 1:3000. The late presentation in adulthood is rare and is reported in the literature. We present anesthetic management of a case of 75 years old male with subacute intestinal obstruction with respiratory distress diagnosed on X-ray Chest and CT chest-abdomen of having left-sided diaphragmatic hernia who admitted for laparoscopic surgical repair.
Keywords
Diaphragmatic hernia, General, epidural anesthesia
Introduction
Diaphragmatic hernias can be classified into congenital and acquired types. Congenital Diaphragmatic Hernia (CDH) includes Bochdalek hernia (70%) in the posterior-lateral and Morgagni hernia (25%-35%) in the anterior or central (2%-5%) part of the diaphragm, resulting in herniation of bowels and liver into the thorax [1]. CDH has an incidence of 1:3000 live births, usually presents immediately after birth with severe respiratory distress, which is life-threatening. 90% of cases are diagnosed antenatally or at birth. 5%-30% may present beyond the neonatal period [2]. There is a severe compromise in respiratory, cardiovascular functions with a strong association of malformations and poor development of the lungs leading to hypoplasia with insufficient gas exchange and pulmonary hypertension that has high morbidity and mortality. Acquired diaphragmatic hernias usually result from all types of blunt and penetrating trauma accounting for the majority. Adult late-onset Congenital Diaphragmatic Hernia (CDH) is uncommon but not rare with variable clinical manifestations like gastro-intestinal cardiopulmonary symptoms [3]. We report a 72-yearold male diagnosed with eventration of the diaphragm or left diaphragmatic hernia becoming symptomatic for the very first time and was scheduled for laparoscopic hernial repair under General Anesthesia (GA) and Epidural Anesthesia (EA).
Case Study
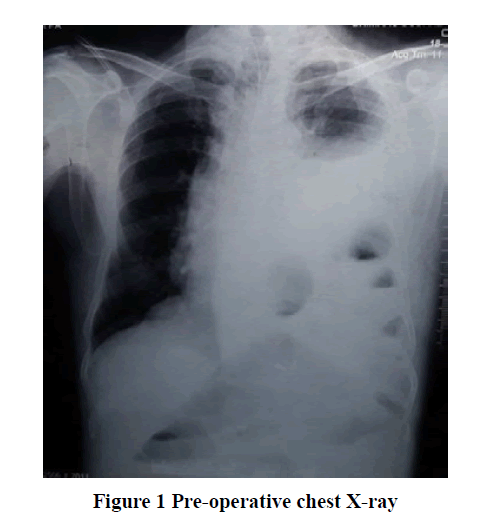
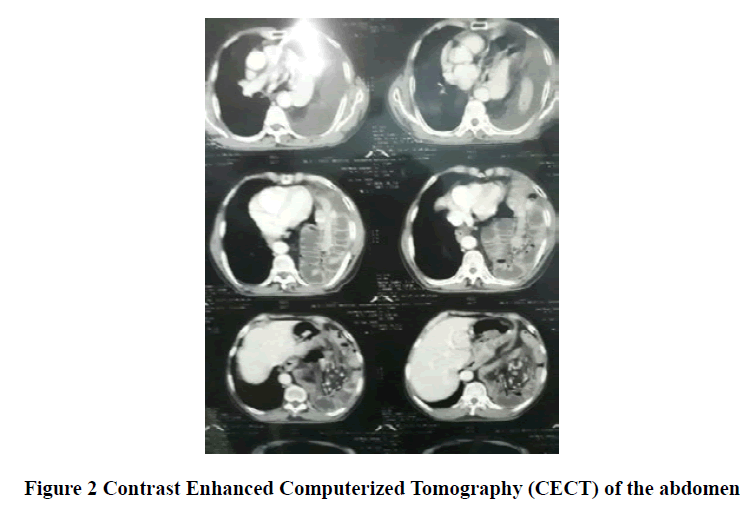
A 75-year male, 55 kg was presented with complaints of nausea and vomiting for 5 days and pain in the abdomen for 15 days. He also complained of difficulty in breathing and recurrent cough, expectoration, and fever suggestive of upper respiratory tract infections for the last 8 months. Other complaints included significant weight loss and a history of previous admissions in the hospital for the same and were treated with conservative medical management. He was a known case of hypertension for 10 years and was on tablet telmisartan 40 mg and amlodipine 10 mg OD with no other surgical history or any abdominal trauma. On general physical examination, the patient was thin and looked dehydrated with no pallor, icterus, cyanosis, clubbing, lymphadenopathy, and edema. The patient was conscious, coherent and vitals were within normal limits. On airway examination Mallampati grade III with 3 finger mouth opening was present. On systemic examination decreased breath sounds in the left hemithorax and bowel sounds were present. Chest X-ray was advised and it showed multilinear gas-filled shadows with moderate pleural effusion in the lower lung fields with blunting of costophrenic angle Figure 1. Further CT scan of thorax and abdomen was done and it showed eventration of left diaphragmatic hernia of bowel loops causing a mediastinal shift towards right, moderate ascites, visualized lung fields showed moderate left pleural effusion with basal sub-segmental atelectatic changes Figure 2. ECG showed sinus tachycardia with 2D Echo findings of EF: 65% with mild diastolic dysfunction. All other routine investigations were within normal limits. The plan of the anesthetic technique of GA with EA and its risk was explained to the patient and relatives. Informed written valid high-risk consent and postoperative ventilator consent were taken. One unit of blood was cross-matched and reserved.
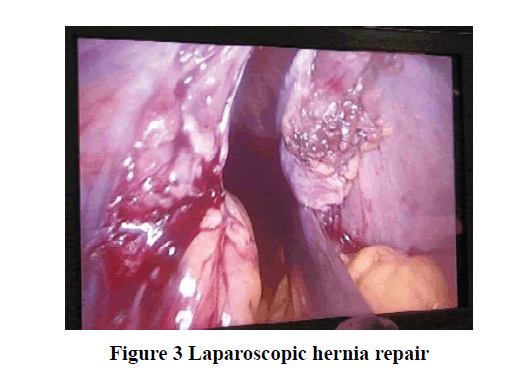
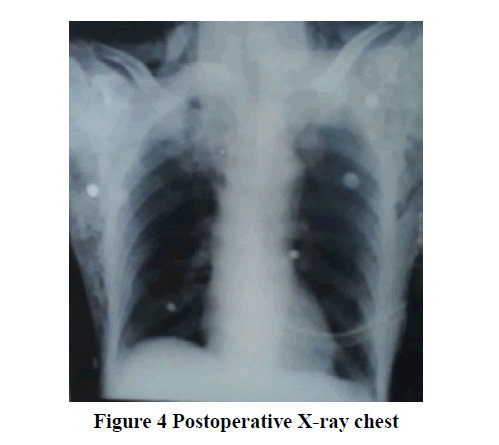
Preoperative optimization was done by nebulizing the patient with bronchodilators and mucolytic agents to improve pulmonary reserve, antibiotic coverage was given. In the operating room, multi-parameter monitors were attached. Premedication and antibiotics were given according to institutional protocol. A nasogastric tube was inserted, and the stomach was deflated. After adequate pre-oxygenation with 100% FiO2 for 5 min, rapid sequence induction with cricoid pressure was performed using fentanyl 80 μg, propofol 100 mg, and succinylcholine 75 mg. The trachea was intubated with right-sided 34-Fr. double-lumen bronchial tube. Anesthesia was maintained with, vecuronium, sevoflurane, and 50% O2 in the air and volume-controlled mode ventilation. The lung isolation technique was used in the initial stage of surgery and once the diaphragmatic defect was repaired both the lungs were ventilated. During one-lung ventilation, SpO2 maintained between 98%-100% by giving Positive End Expiratory Pressure (PEEP) of 5 mmHg using 100% oxygen. Under all aseptic precautions, the thoracic epidural catheter (T9-T10) was placed using 18G Tuohy’s needle by loss of resistance technique to air, 18G epidural catheter was introduced and fixed at 10 cm. Inj. lignocaine with adrenaline 2% 2cc test dose was given and catheter placement was confirmed and the first dose of 8 ml of 0.25% bupivacaine was injected after induction of anesthesia. Laparoscopic Bochdalek diaphragmatic hernia repair with a defect of (4 × 4) cm and the mesh was placed and the chest drain tube on the right side was inserted Figure 3. Intraoperative monitoring was done with ECG, SpO2, EtCO2, temperature, urine output, invasive blood pressure, and Central Venous Pressure (CVP) with a double lumen catheter in the right internal jugular vein. The duration of surgery was 3 hours and the patient was hemodynamically stable with all the vital parameters. Blood loss was around 250 ml and urine output of 300 ml CVP measured 14 cm. At the end of the surgery, the double-lumen tube was exchanged with a single lumen No. 8 portex tube under vision. The patient was shifted intubated to SICU and was mechanically ventilated for 24 hrs in view to assist the lung expansion. Epidural top-up was given for postoperative analgesia with 8 ml of 0.125% bupivacaine. The patient was extubated on postoperative day one and the epidural catheter was removed after 72 hrs. Postoperative chest X-ray, ABG was advised and they were normal. Post-operative X-ray chest on day 3 showed complete good lung expansion Figure 4.
Discussion
Diaphragmatic hernia beyond the neonatal period varies from 5% to 30% [2]. In newborns and infants, diaphragmatic hernias result in life-threatening symptoms such as respiratory distress, therefore it should be corrected surgically [2,3]. Failure or incomplete fusion of the posterior compartment of the diaphragm leads to Bochdalek hernia which is commonest among the other hernias like Morgagni hernia and esophageal hiatus. Bochdalek hernia is associated with chromosomal disorders (10%-25%) and other congenital defects (25%-57%) [4]. Late-onset of CDH is more difficult to diagnose as they present with vague symptoms of cardiorespiratory and others which can mislead the diagnosis. And one should always have a differential diagnosis of diaphragmatic hernia in the list of such scenarios. On systemic evaluation, one can pick up the findings, and still, Chest X-ray and Contrast Enhanced Computerized Tomography (CECT) of the chest and abdomen remain the gold standard in diagnosing these cases [5]. Anesthetic management of such adult type of CDH are very challenging to anesthesiologists in every stage that could be in proper planning of anesthetic technique, considering them as full stomach and providing required aspiration prophylaxis, all the necessary modalities for hemodynamic monitoring and always anticipating a difficult airway and keeping a difficult airway cart ready is a must. Early diagnosis and proper management of symptomatic CDH is appropriate, otherwise, patients may present with acute bowel obstruction or cardiorespiratory distress, pulmonary hypertension, and may land up in complications and emergency surgery. Amongst different surgical approaches, laparoscopic repair is considered safe and effective. But there are more chances of pneumothorax and very high airway pressures during the procedure [6]. As in our case, all the necessary precautions were taken and the case was managed well with a good patient outcome.
Conclusion
Although CDH in adults is a rare presentation it is challenging for the anesthesiologist which requires special care especially when it comes to emergency surgery. In our case which presented as semi-emergency, we could manage successfully with proper planning of GA with one-lung ventilation using double-lumen tube +EA for laparoscopic hernia repair.
Laparoscopic repair of CDH hernia has also been described and is considered to be a safe and effective procedure, but it provides different challenges for anesthesiologists as there are more chances of pneumothorax and very high airway pressures during the procedure. Basic principles of anesthetic management remain the same, and to avoid pneumothorax, intra-abdominal pressure should be kept low, and one must avoid nitrous oxide. If there is a decrease in SpO2 during the procedure, ask for lowering the intra-abdominal pressure or stop surgery and ventilate the lung with 100% oxygen and PEEP post-procedure chest radiograph should be advised to look for pneumothorax.
Declarations
Acknowledgments
We thank the Department of surgery for their cooperation and for sharing the patients’ details for publication.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
None.
References
- Kotecha, Sailesh, et al. "Congenital diaphragmatic hernia." European Respiratory Journal, Vol. 39, 2012, pp. 820-29.
- Sridhar, A. V., and S. Nichani. "Late presenting congenital diaphragmatic hernia." Emergency Medicine Journal, Vol. 21, No. 2, 2004, pp. 261-62.
- Bianchi, Enrica, et al. "Congenital asymptomatic diaphragmatic hernias in adults: A case series." Journal of Medical Case Reports, Vol. 7, No. 1, 2013, pp. 1-8.
- Nama, Rajnish K., et al. "Anesthetic management of Morgagni hernia repair in an elderly woman." Anesthesia, Essays and Researches, Vol. 9, No. 3, 2015, pp. 413-16.
- Malekzadegan, Alireza, and Alireza Sargazi. "Congenital diaphragmatic hernia with delayed presentation." Case Reports in Surgery, Vol. 2016, 2016.
- Takeyama, Kazuhide, et al. "Anesthetic management for repair of adult Bochdalek hernia by laparoscopic surgery." Journal of Anesthesia, Vol. 19, No. 1, 2005, pp. 78-80.