Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Asthma Education and Its Effect on Patient Management
Amr S Albanna1,2*, Raed A Alghannam1, Moayyad Malas1, Essam A Alhejaili1 and Ali Alshamrani12Royal Victoria Hospital, McGill University, Montreal, Canada
Amr S Albanna, King Abdullah International Medical Research Center, King Abdulaziz Medical City, Jeddah, Saudi Arabia, Email: amralbanna@gmail.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021
Abstract
Objectives: To evaluate the level of asthma education and the effects of this education on avoidance of irritants and adherence to inhalers.
Methods: A cross-sectional study of adults with asthma in respiratory clinics of a tertiary hospital was conducted between September 2014 and September 2015. A standardized questionnaire was designed to measure the level of education received by asthmatics related to their disease, irritants, medications, and inhaler technique. Comparative analysis was performed using a chi-square test.
Results: 82 subjects were given the questionnaire and all were included. 70% received basic information about asthma, but only 44% were educated about major irritants (i.e. smoking, indoor irritants, outdoor irritants, colds, influenza, and exercise). Adherence to avoidance measures was significantly higher in patients who received education than in those without adequate education. However, education about inhalers, which was provided to the majority (88.8%) of the patients, was not associated with the quality of the respondents’ technique in using these devices. Patients were more likely to demonstrate correct use of a DISKUSβ® inhaler than a metered-dose inhaler or Turbohaler® (85%, 42%, and 52% of patients, respectively, p=0.003).
Conclusion: Almost half of the patients had not received sufficient education. Asthma education, which was provided mostly in the clinic by the treating physician, was associated with avoidance of irritants, but not with high-quality inhaler technique. To achieve the standard requirement for asthma management, a multidisciplinary educational program that ensures adequate understanding and proper use of inhalers is recommended
Keywords
Asthma, Education, Irritants, Inhaler, Adherence
Introduction
Asthma is the most common chronic pulmonary disease, affecting >300 million people globally [1]. Its prevalence has increased in recent decades, and in Saudi Arabia, according to the literature, asthma has been estimated to affect 23% of the total population [2]. It has also a considerable effect on public health, causing an estimated loss of 15 million Disability-Adjusted Life Years (DALYs) per year worldwide, which is similar to each of the statistics for liver cirrhosis, schizophrenia, and diabetes [3,4].
People with asthma develop symptoms after exposure to irritants such as allergens, as well as after exercise and during infections that affect the respiratory tract. The symptoms develop as a result of reversible airway hyper-responsiveness and hyper-secretion of mucus [3]. Asthma is a controllable disease that is managed using inhaled corticosteroids and β2-adrenergic receptor agonists administered through inhaler devices. The most commonly used types of inhalers are the Metered-Dose Inhaler (MDI) and Dry-Powder Inhalers (DPI) such as the Turbohaler® (AstraZeneca, London, UK), and the DISKUS® (GlaxoSmithKline, Brentford, UK). In one study, by Harnett, et al. it was noted that the most commonly used inhaler was the MDI in 61% of the patients. Turbohaler® was the second most common as it was used by 52% of the patients [5]. Harnett, et al. also assessed inhaler technique among patients with asthma and showed that 88% of patients using Turbohaler® were making at least one error in the administration. MDI, however, was associated with less percentage of incorrect use of 63%. Both were improved after providing education and follow-up after 3 months to become 38% for Turbohaler® and 17% for MDI users, respectively [5].
Asthma education relating to irritants, types of medication, and the proper use of inhaler devices is an integral component of treatment to control symptoms and reduce overall morbidity and mortality [6]. Results published in 2013 showed that >50% of patients with asthma in Saudi Arabia received no education relating to asthma or its management; this lack of education was associated with poor asthma control and more emergency department visits [7]. In India, a study was done to include 300 cases of COPD and asthma patients. This study showed that 100% of selftaught patients used their inhalers incorrectly. Among patients who received education on administration techniques, 94.3% of MDI users committed an error during the administration process in comparison to 70% in patients who used dry-powder inhalers [8]. Another study done in Turkey on elderly patients (age 60 years or older) showed that only 22 out of the 82 included patients demonstrated good administration technique [9]. Manriquez, et al. also performed a study on 128 adult patients with asthma to assess their technique in the administration of inhaler devices and found that 91% of adult asthma patients do not perform proper technique [10].
In this context, our objective was to evaluate the effect of asthma education relating to irritants and inhaler devices on the avoidance of these irritants and the adherence to proper inhaler techniques.
Materials and Methods
Population and Study Design
This questionnaire-based cross-sectional study was conducted from September 1st, 2014 to September 30th, 2015 at King Abdulaziz Medical City, a tertiary care center located in Jeddah, Saudi Arabia. After ethical approval had been received from the facility’s institutional review board, data collection took place in respiratory outpatient clinics by trained medical professionals who obtained consent from and performed the interviews.
The required sample size was calculated to be around 80 individuals, based on an anticipated improvement in the outcome measure (avoidance of asthma irritants) from less than 50% to over 80% with education, a power of 80%, and a two-sided α of 0.05. The study cohort comprised adult patients (aged ≥ 18 years) who attended the respiratory outpatient clinic for routine follow-up visits with a previous diagnosis of asthma, which was defined based on typical clinical features and either pulmonary-function test findings of airflow limitation with reversibility (change in the Forced Expiratory Volume in 1 s (FEV1) of 12% and 200 ml) or clinical response to asthma medications.
Patients with the following conditions were excluded from the study: known underlying lung disease other than asthma (for example, chronic obstructive pulmonary disease, bronchiectasis, or interstitial lung disease), decompensated heart failure, and poor overall performance status (inability to perform self-care activity).
Data Source and Measurements
All patients were given a standardized, interview-based questionnaire, which was designed to encompass all educational elements listed in the Global Initiative for Asthma guidelines. The questionnaire requested information on patient demographics, education provided by healthcare workers, measures taken to avoid asthma irritants, and the patient’s technique for using an inhaler device. However, healthcare workers who may have provided education to the patients were not informed about the interview process.
In the questionnaire, asthma education was classified into four categories: basic questions about the disease, asthma irritants, medications, and action plans. Appropriate responses in all four categories were required for a patient to be considered adequately educated about asthma. Basic information being the inflammatory nature of the disease, its episodic clinical characteristics, and airflow limitation. Education relating to irritants was classified into five subcategories: smoking; indoor irritants, including Bakhour (an incense that is burned to produce a scent which is commonly used by the Saudi population), pets, mold, dust mites, and cockroaches; outdoor irritants, including weather changes and pollution; colds and influenza; and exercise. Patients who had received education about all five sections were considered to be adequately educated about asthma irritants. The action plan category focused on the participants’ knowledge on when to modify the treatment regimen and when to visit the emergency department. Education about medications included the type of inhaler device based on its properties and the frequency and technique of its administration.
The inhaler-administration technique of each participant was then observed by the interviewer and graded based on the completion of the objective essential steps of usage for the given device. We used a validated checklist obtained through Oman Respiratory Society that labels participants as either having a good technique when all the essential steps are performed correctly or poor technique when at least one essential step is missed [11].
To determine the effect of education on the avoidance of irritants, the measures taken by patients to avoid tobacco smoke, indoor irritants (pets, mold, dust mites, Bakhour, and cockroaches), colds, influenza, and air pollution were assessed.
Statistical Analysis
Patient characteristics were described by proportions for dichotomous variables and means for continuous variables. A chi-square test was used for the comparative analysis. Two-tailed P values of <0.05 indicated a statistically significant difference in comparison. All analyses were performed using SPSS software version 22.
Results
A total of 82 patients were provided with the questionnaire, completed it, and were included in the study. Demographic characteristics are shown in Table 1.
| Characteristic | Value | 95% CI |
|---|---|---|
| Age (mean) | 44.7 years | 41.1-48.4 years |
| Gender (male) | 37.00% | 27.0%-48.0% |
| Occupation | ||
| Employed | 26.30% | 17.0%-37.3% |
| Student | 10.00% | 4.4%-18.8% |
| Housewife | 41.30% | 30.4%-2.8% |
| Unemployed | 13.80% | 7.1%-23.3% |
| Other | 8.80% | 3.6%-17.2% |
| Housing | ||
| Apartment | 52.40% | 41.1%-63.6% |
| Villa or house | 29.30% | 19.7%-40.4% |
| Other | 18.30% | 10.6%-28.4% |
| Education | ||
| Elementary | 17.10% | 9.7%-27.0% |
| Intermediate | 6.10% | 2.0%-13.7% |
| Secondary | 24.40% | 15.6%-35.1% |
| College | 32.90% | 22.9%-44.2% |
| Illiterate | 19.50% | 11.6%-29.7% |
| The income per month (Saudi Riyals) and it's equivalent in (United State Dollar) | ||
| <5,000 SR ≈ 1333 USD | 35.90% | 25.3%-47.6% |
| 5,000-9,999 SR ≈ 1333-2666 USD | 35.90% | 25.3%-47.6% |
| 10,000-14,999 SR ≈ 2666-3999 USD | 9.00% | 3.7%-17.6% |
| 15,000-19,999 SR ≈ 3999-5332 USD | 12.80% | 6.3%-22.3% |
| ≥ 20,000 SR ≈5332 USD | 6.40% | 2.1%-14.3% |
| Comorbidity | 58.50% | 47.0%-69.0% |
| Smoking history | 8.60% | 4.0%-17.0% |
Table 1: Demographic characteristics of the participants (n=82).
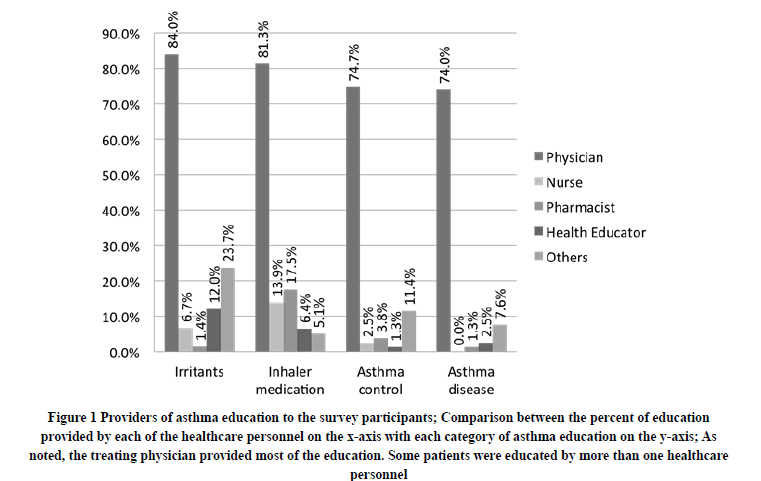
Participants reported that education about all aspects of asthma was typically given by physicians during clinic visits (Figure 1). Nevertheless, 48% of the subjects did not satisfy the criteria for an adequate overall education relating to asthma. Meaning they did not have sufficient knowledge of the four categories.
Figure 1. Providers of asthma education to the survey participants; Comparison between the percent of education provided by each of the healthcare personnel on the x-axis with each category of asthma education on the y-axis; As noted, the treating physician provided most of the education. Some patients were educated by more than one healthcare personnel
Seventy percent of participants had received education in one or more of the subcategories of basic information about asthma, and 72% had received education on how to assess asthma control, when to adjust their medication dose and when to go to the emergency department (Table 2). Concerning asthma irritants, over 80% of participants had received education in at least one subcategory. However, only 43.9% were educated in all five subcategories. Notably, participants who were educated about irritants reported significantly higher levels of measures to avoid these irritants than participants who were not educated in this category (Table 3).
| Percentage (%) | 95% CI | |
|---|---|---|
| Basic information about asthma | ||
| Airway inflammation | 58.5 | 47.7-69.4 |
| Airway narrowing | 65 | 54.3-75.7 |
| Variable (episodic) in nature | 62.2 | 51.5-72.9 |
| Education in one or more subcategories | 70.4 | 60.2-80.5 |
| Education about irritants | ||
| Smoking | 70.4 | 60.2-80.5 |
| Indoor irritants | 84.2 | 76.1-92.2 |
| Pets | 61 | 50.2-71.8 |
| Dust mites | 42 | 31.0-53.0 |
| Mold | 38.8 | 27.8-49.7 |
| Cockroaches | 39.2 | 28.2-50.3 |
| Bakhour | 80.3 | 71.4-89.1 |
| Outdoor irritants | 76.8 | 67.5-86.2 |
| Pollution | 63 | 52.2-73.7 |
| Weather changes | 54.9 | 43.9-65.9 |
| Colds and influenza | 64.6 | 54.1-75.2 |
| Exercise | 51.3 | 40.1-62.4 |
| Education in all subcategories | 43.9 | |
| Education about inhaler medications | ||
| Types (controllers vs. relievers) | 67.1 | 56.5-77.7 |
| Device technique | 81.5 | 72.8-90.1 |
| Time and frequency of administration | 84 | 75.8-92.1 |
| Education in one or more subcategories | 88.8 | 81.7-95.8 |
| Education about asthma control | ||
| Assessment of asthma control | 57 | 45.8-68.1 |
| Dose adjustment (action plan) | 60.5 | 49.6-71.4 |
| Need for emergency-room visit | 58 | 47.0-69.0 |
| Education in one or more subcategories | 72 | 62.0-81.9 |
Table 2: Type of health education provided to patients with asthma.
| Irritant avoided | Total (%) | Educated (%) | Not educated (%) | p-valuea |
|---|---|---|---|---|
| Smoking | 75.9 | 91 | 42 | <0.001 |
| Indoor irritants | ||||
| Pets | 61.4 | 80.5 | 31 | <0.001 |
| Cockroaches | 51.7 | 96.2 | 22.7 | <0.001 |
| Mold | 51.8 | 95.7 | 25 | <0.001 |
| Bakhour | 77.8 | 81 | 53.3 | 0.028 |
| Dust mites | 47.3 | 81.5 | 25 | <0.001 |
| Colds and influenza | 56.9 | 82.9 | 26.9 | <0.001 |
| Pollution | 69.1 | 83.3 | 38.5 | <0.001 |
a p-value for Chi-square test performed to compare avoidance of irritants between educated and not educated groups
Table 3: The proportion of patients who used measures to avoid asthma irritants, stratified by whether or not education about these irritants were provided.
Although education about the technique of using inhaler devices was provided to 82% of our population, it did not influence patients’ adherence to proper administration technique, which was 39% among educated patients and 30% among non-educated patients (p=0.57). However, a comparison of the different types of inhalers showed significant differences in patient adherence. Proper use of the DISKUS® device was observed in a significantly higher proportion of patients than for other devices (85%, compared with 52% for the Turbohaler® and 42% for the MDI, p=0.003) (Table 4).
| Number of patients using the device | Percentage of patients using the device correctly | 95% CI (%) | |
|---|---|---|---|
| MDI metered-dose inhaler | 57 | 42.1 | 29.1-55.9 |
| Turbohaler® | 31 | 51.6 | 34.3-68.7 |
| DISKUS® | 13 | 84.6 | 57.8-97.3 |
| All prescribed devices | 70 | 37.1 | 25.9-49.5 |
Notes: The treatment regimen of some patients included a combination of more than one device (for example, MDI as a reliever medication and DISKUS® as a controller medication).
Table 4: Proper device technique among patients with asthma
Discussion
In our cross-sectional study of 82 patients with asthma in Jeddah, Saudi Arabia, 52% of respondents had received some education in each of four categories relating to the disease. Approximately 30% of the respondents provided responses indicating that they had not received any education about the nature of asthma as an episodic disease that involves airway inflammation and narrowing. Although most of the respondents knew one or more subcategories relating to asthma irritants, only 44% had received education on all five subcategories. Bakhour was the irritant that had most commonly been mentioned to patients, followed by tobacco smoking. Education about irritants had a significant effect on efforts to avoid them (p=values in Table 3). Although we could not determine the extent to which these avoidance measures reduced exposure to the irritants, and whether any reduction in exposure was reflected in disease activity, these results indicate the potential value of education to bring about change in patients’ behavior. Further research may be directed to measure the effect of education about irritants and their impact on disease activity.
Unlike the other categories, education about asthma medications was provided to most included patients. However, this information did not significantly affect patients’ technique when using their inhaler devices (39% among educated versus 30% among non-educated patients, p-value: 0.57). Most education was provided by a physician during a clinic visit when time constraints do not generally enable proper demonstration and observation of a patient’s technique. Health educators, who are personnel devoted to delivering certain educational material to the patients, on the other hand, had a small role in educating patients. One study done in Europe found that education provided by a physician was the worst among other health care providers [12]. Strikingly, across different inhaler devices, the technique used with the DISKUS® device was correct in a significantly higher proportion of patients than the technique with Turbohaler® or MDI devices. This finding is consistent with a previously conducted study in Italy which showed that DISKUS® was used more correctly than Turbohaler® [13]. The explanation of this difference, however, is not clear and may be related to the simplicity of using DISKUS®, compared to other devices, rather than the amount of education.
A previously conducted study in Saudi Arabia showed that almost half of patients who visited the emergency department were not educated about asthma as a disease, and approximately 41% did not receive any education about inhaler-device techniques [7]. This low level of education about inhaler devices could reflect the selection of a high-risk population of patients who visited the emergency department. By contrast, in our study, the population was selected from outpatient clinics, to include a wide variety of patients with different levels of asthma control. Another multicenter study, which included 349 patients in Spain, showed that education about asthma disease, medications, and inhaler devices technique significantly improved patients’ symptoms and quality of life [14]. This finding highlights the importance of education for disease control.
One of the limitations of the present study is that our sample was limited to a single healthcare center and may not be representative of the wider population of asthma at a national level. Since the study was conducted in a well-equipped tertiary center, its results may overestimate the actual level of education provided in all different health care sectors. In addition, the effect of education on asthma control was not assessed. We intend to assess asthma control with follow-up visits of the same patients in a future study. Also, the questionnaire used was not validated. However, the questions were designed to ask participants whether education was provided to them or not, and it was not to test their knowledge.
The pandemic of COVID-19 has a great impact on managing patients with chronic illness, especially asthma. Chronic asthmatic patients are more prone to seasonal variability and frequent excerptions, thus putting them among those who require more hospital visits as well as frequent adjustment of their treatments. Keep in mind that there was a huge constrain to access the healthcare system in this crucial time, for example, curfew restriction and outpatient clinic with its closed door. Not only those, but people who suffer from asthma were also under the pressure to visit the emergency departing fearing contracting COVID-19.
Just to mention a few of the challenges. The use of aerosolized generating nebulized treatment in the emergency department, the use of steroid in its both formulations inhaled or oral and close follow up of these patients physically in the clinic [15]. These challenges open a new window to discover means to be overcome. Technology has evolved during the last decade leading to the development of telemedicine. With the use of video and phone calls, the virtual clinic was running and patient management was not cumbersome indeed it was easier to use and utilize time more efficiently [16].
Conclusion
Lastly, these correlations of COVID pandemic and its impact on asthma patient management were not among the indented variable in our current study and further paper to elaborate on it would be a necessity.
In conclusion, although education is an integral component of asthma management, it was not provided sufficiently to a large proportion of patients managed in our tertiary care center to a degree that we can call them educated. Even when education was provided, it was mostly given by the treating physician during busy clinic visits, which may reflect the insufficient education provided to the patient. The incomplete provision of education is reflected in the fact that almost half of the patients did not take any measures to avoid indoor asthma irritants, and only 37% used their inhaler devices correctly. To provide effective education, a well-planned, comprehensive multidisciplinary education program should be conducted with the participation of trained health educators, pharmacists and not to forget the role of social media, all of which need to be furtherly studied in the future.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Colledge, Nicki R. "Davidson's principles and practice of medicine." 2010.
- Al Frayh, A. R., et al. "Epidemiology of asthma and allergic rhinitis in two coastal regions of Saudi Arabia."Allergy and Immunology,Vol. 21, No. 10, 1989, pp. 389-93.
- Longo, Dan L., et al."Harrison's principles of internal medicine 18E Vol 2 EB." McGraw Hill Professional, 2012.
- Masoli, Matthew, et al. "The global burden of asthma: Executive summary of the GINA Dissemination Committee report."Allergy,Vol. 59, No. 5, 2004, pp. 469-78.
- Harnett, C. M., et al. "A study to assess inhaler technique and its potential impact on asthma control in patients attending an asthma clinic."Journal of Asthma,Vol. 51, No. 4, 2014, pp. 440-45.
- GIf, Asthma. "GINA global strategy for asthma management and prevention." 2012.
- Hamdan, AL-Jahdali, et al. "Improper inhaler technique is associated with poor asthma control and frequent emergency department visits."Allergy, Asthma and Clinical Immunology,Vol. 9, No. 1, 2013, pp. 1-7.
- Arora, Piyush, et al. "Evaluating the technique of using inhalation device in COPD and bronchial asthma patients."Respiratory Medicine,Vol. 108, No. 7, 2014, pp. 992-98.
- Ozturk, A. B., et al. "Association between asthma self-management knowledge and asthma control in the elderly."Annals of Allergy, Asthma and Immunology,Vol. 114, No. 6, 2015, pp. 480-84.
- Manríquez, Pablo, et al. "Study of inhaler technique in asthma patients: Differences between pediatric and adult patients."Brazilian Journal of Pulmonology,Vol. 41, No. 5, 2015, pp. 405-09.
- Oman Respiratory Society and Oman Famco Society. "Guidelines for management of asthma." 2009. https://www.moh.gov.om/documents/272928/1314763/Guidelines+for+management+of+Asthma+Second+edition+2009+%281%29.pdf/c5e8ff0c-d937-4c57-bc2b-d225c26be727
- Lavorini, Federico, and Omar S. Usmani. "Correct inhalation technique is critical in achieving good asthma control."Primary Care Respiratory Journal,Vol. 22, No. 4, 2013, pp. 385-86.
- Voshaar, Thomas, et al. "Comparing usability of NEXThaler® with other inhaled corticosteroid/long-acting β2-agonist fixed combination dry powder inhalers in asthma patients."Journal of Aerosol Medicine and Pulmonary Drug Delivery,Vol. 27, No. 5, 2014, pp. 363-70.
- Giner, J., et al."Multicenter and prospective study of" education and teaching "of the inhalation procedure in respiratory patients (EDEN Study)."Archives of Bronconeumology,Vol. 38, No. 7, 2002, pp. 300-05.
- Chai, C. S., and C. K. Liam. "Common concerns in managing bronchial asthma during the COVID-19 pandemic."International Journal of Tuberculosis and Lung Disease,Vol. 24, No. 7, 2020, pp. 750-52.
- Beaney, Thomas, et al. "Assessment and management of adults with asthma during the covid-19 pandemic."BMJ,Vol. 369, 2020.