Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Brown-Sequard Syndrome Caused by a Large Disc Herniation in C3/4: A Case Report and Review of the Literature
Khalid Alsaleh*Khalid Alsaleh, Department of Orthopedics, College of Medicine, King Saud University, Kingdom of Saudi Arabia, Tel: 96114670000, Email: khalsaleh@ksu.edu.sa
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021
Abstract
Introduction: Brown-Sequard syndrome is uncommon in clinical practice and is very rarely caused by cervical disc herniation. We report a case of Brown-Sequard syndrome due to a disc herniation in C3-C4. Case report: A 39-yearold male presented to the emergency department with neck pain and progressive right hemiparesis. After been initially thought to have a cerebrovascular accident, a thorough assessment and investigation showed he had a left-sided large disc herniation at the level of C3-C4. An urgent C3-C4 anterior cervical discectomy and fusion were performed. He achieved full motor recovery within two weeks after surgery, but some sensory deficits persisted until the last follow-up visit. Conclusion: Due to its rarity, Brown-Sequard syndrome-without a preceding traumatic event- can be confused with other clinical syndromes. A delay in diagnosis and treatment may be detrimental to the outcome. A careful physical exam coupled with a high index of suspicion can provide good outcomes in most cases.
Keywords
Cervical spine, Disc herniation, Brown-Sequard syndrome
Introduction
Brown-Sequard Syndrome (BSS) is a clinical syndrome characterized by an acute loss of ipsilateral motor function with contralateral loss of temperature sensation and pain [1]. This clinical presentation is due to dysfunction of the cortico-spinal tract and the spinothalamic tract. Although the first description in 1849-was due to penetrating spinal cord injury, the clinician commonly encounters it in the setting of spinal trauma or-occasionally-in spinal neoplasia. More recently, BSS has been reported in cases of ischemic cord infarction, epidural hematoma, and intervertebral disc herniation [2-4]. Cases of high cervical disc herniation causing BSS are rare. The first report was by Stookey in 1928 [5]. In the past two decades, five more reports of a C3-C4 disc herniation causing BSS have been published [6-10]. In this report, we describe a case of a large C3-C4 disc herniation presenting as a case of BSS in a young man.
Case Report
A 39-year-old male pharmacist presented with acute onset of right upper and lower limb weakness of 2 hours duration. There was no prior history of trauma. The emergency room staff reviewed the patient, and their notes clearly state that “Physical examination revealed 4/5 power in both upper and lower limbs on the right side”. He was referred for an urgent Computerized Axial Tomography (CT) scan of the brain to rule out an acute Cerebrovascular Attack (CVA). As the CT was negative, the patient was reassured about the result and told he needed a neurologist’s review. On further, detailed physical examination by neurology: Cranial nerve examination was normal while power was diminished in the right arm and leg with absent temperature and pain sensation in the left arm, trunk, and leg. Sacral sensation and sphincter function were intact. Neck mobility was limited due to pain. At the same time, the motor assessment showed progression of the right upper and lower limb weakness (2/5).
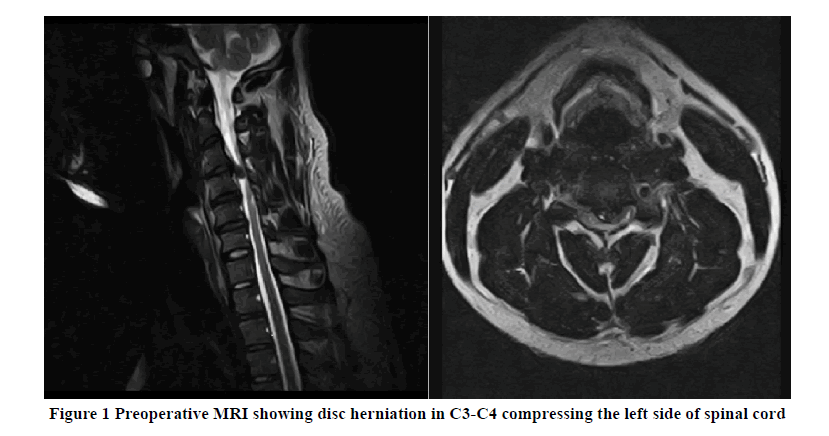
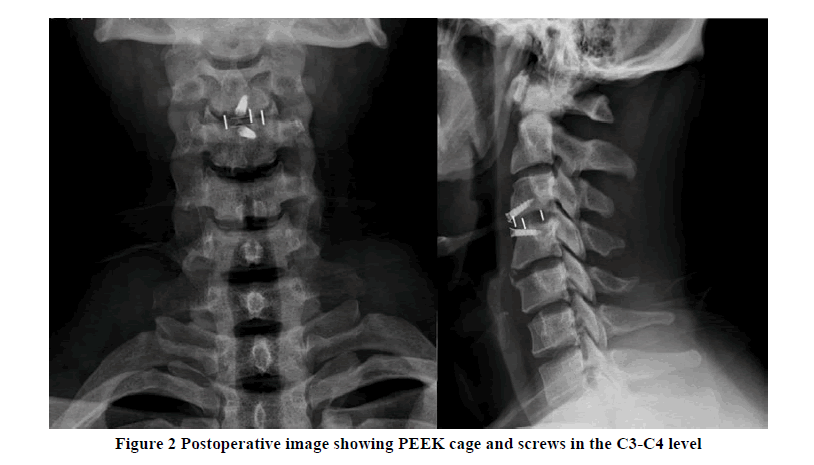
An urgent Magnetic Resonance Imaging (MRI) of the cervical spine was performed, which showed a large central disc herniation at C3/4 compressing the left side of the cord and deforming it (Figure 1). The patient was referred to the spine surgeon, and the decision was made for an emergent C3/4 discectomy. This was done utilizing the standard anterior Smith-Robinson approach [11]. Intra-operatively, the posterior longitudinal ligament was found to be torn, and a large disc fragment was found partly posterior to the vertebral body of C4. It was removed in its entirety in one piece. The endplates were prepared, and an appropriately sized Polyetheretherketone (PEEK) cage was inserted after filling it with allograft bone chips. The wound was then closed over a small closed-suction drain.
In the immediate post-operative period, the patient had 3/5 movement in both upper and lower limbs on the right sidewhich improved to 4/5 power 24 hours following surgery. He was then discharged home, capable of walking with a normal gait and not having any balance or proprioception issues. By two weeks postoperative, the patient recovered all motor power but showed no improvement with regards to temperature and pain sensation deficit in his left side. This remained the case until his latest follow-up two years after surgery, where his fusion was found to be fully mature radio-graphically (Figure 2).
Discussion
The prevalence of cervical disc herniation varies from 2.8% to 20% in asymptomatic individuals [12-15]. Symptom atic individuals diagnosed to have cervical disc herniation typically present with radiculopathy, myelopathy/spinal cord injury, or both. The majority of cases involve the lower cervical levels (C5-C6 and C6-C7). The incidence of disc herniations in the level of C3-C4 is only 16%, while BSS incidence due to a cervical disc herniation is only 2.6% in the series by Jomin [16]. The etiology of BSS was once thought to be primarily due to penetrating trauma [17,18]. More recent reports have shown that a large number of cases are due to blunt trauma to the cervical spine [19-21]. Regardless, cases of BSS due to disc herniation remain small and reported as case reports with a few series [4,6,22]. The instances of BSS due to a C3-C4 disc herniation are rare [5-10]. They are summarized in the table below (Table 1).
Table 1: Summary of all BSS cases -due to C3-C4 disc herniation-cases in the literature
| References | Age | Gender | Presentation | Procedure | Outcome |
|---|---|---|---|---|---|
| [5] | 44 | Male | Left hemiparesis | Laminectomy | Not reported |
| [6] | 34 | Male | Not reported | ACDF | Partial recovery |
| [7] | 52 | Female | Right hemiparesis | ACDF | Complete recovery |
| [8] | 46 | Male | Left hemiparesis | ACDF | Partial recovery |
| [9] | 28 | Male | Left hemiparesis | ACDF | Complete recovery |
| [10] | 63 | Male | Right hemiparesis | Laminoplasty | Complete recovery |
ACDF: Anterior Cervical Discectomy and Fusion
When looking at the more recent reports of cervical disc herniation causing BSS, the majority of these cases were -unsurprisingly- treated with anterior cervical discectomy and fusion [23-33]. The few reports of treatment by laminectomy were before the widespread utilization of the anterior approach [34,35]. Some form of neurologic recovery was encountered in all cases, but complete recovery happened in around 50% of all cases. Given the inconsistency of reporting on any delay in diagnosis or treatment, it is difficult to derive any judgments on the correlation of early surgery with better clinical outcomes.
Conclusion
Brown-Sequard syndrome is not commonly encountered in clinical practice. Having a high index of suspicion may aid management. Excellent outcomes can be expected if surgical treatment is provided early. Anterior cervical discectomy and fusion is the standard approach for such cases, as it offers direct decompression, minimal complications, and rapid recovery.
Declarations
Ethical Statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from the patient for being included in the study.
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Brown-Sequard, CE "On the transmission of sensory impressions through the spinal cord." CR Soc Biol, Vol. 1, 1849, pp. 192-94.
- Dolan, Ross, Graeme Houston, and Jonathan O'Riordan. "Brown-Séquard syndrome due to non-compressive disc prolapse and spinal cord infarction." QJM: An International Journal of Medicine, Vol. 102, No. 3, 2009, pp. 225-27.
- Kashyap, Samir, Gohar Majeed, and Shokry Lawandy. "A rare case of Brown-Sequard syndrome caused by traumatic cervical epidural hematoma." Surgical Neurology International, Vol. 9, 2018, p. 213.
- Abouhashem, Safwat, et al. "Management of Brown-Sequard syndrome in cervical disc diseases." Turkish Neurosurgery, Vol. 23, No. 4, 2013, pp. 470-75.
- Stookey, Byron. "Compression of the spinal cord due to ventral extradural cervical chondromas: Diagnosis and surgical treatment." Archives of Neurology & Psychiatry, Vol. 20, No. 2, 1928, pp. 275-91.
- Kohno, Michihiro, et al. "Postoperative prognosis of Brown-Séquard-type myelopathy in patients with cervical lesions." Surgical Neurology, Vol. 51, No. 3, 1999, pp. 241-46.
- Clatterbuck, Richard E., Allan J. Belzberg, and Thomas B. Ducker. "Intradural cervical disc herniation and Brown-Séquard's syndrome: Report of three cases and review of the literature." Journal of Neurosurgery: Spine, Vol. 92, No. 2, 2000, pp. 236-40.
- Sayer, Faisal T., et al. "Brown-Sequard syndrome produced by C3-C4 cervical disc herniation: A case report and review of the literature." Spine, Vol. 33, No. 9, 2008, pp. E279-82.
- Kim, Shin-Jae, et al. "Brown-Séquard syndrome caused by acute traumatic cervical disc herniation." Korean Journal of Neurotrauma, Vol. 15, No. 2, 2019, pp. 204-08.
- Yokoyama, Kunio, et al. "Cervical disc herniation manifesting as a Brown-Sequard syndrome." Journal of Neurosciences in Rural Practice, Vol. 3, No. 2, 2012, pp. 182-83.
- Robinson, R. "Anterolateral disc removal and interbody fusion for cervical disc syndrome." Bull Johns Hopkins Hosp, Vol. 96, 1955, pp. 223-24.
- Teresi, Louis M., et al. "Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging." Radiology, Vol. 164, No. 1, 1987, pp. 83-88.
- Lehto, I. J., et al. "Age-related MRI changes at 0.1 T in cervical discs in asymptomatic subjects." Neuroradiology, Vol. 36, No. 1, 1994, pp. 49-53.
- Boden, Scott D., et al. "Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation." The Journal of Bone and Joint Surgery. American, Vol. 72, No. 8, 1990, pp. 1178-84.
- Matsumoto, Morio, et al. "MRI of cervical intervertebral discs in asymptomatic subjects." The Journal of Bone and Joint Surgery. British, Vol. 80, No. 1, 1998, pp. 19-24.
- Jomin, M., et al. "Herniated cervical discs." Acta Neurochirurgica, Vol. 79, No. 2, 1986, pp. 107-13.
- Peacock, W. J., R. D. Shrosbree, and A. G. Key. "A review of 450 stabwounds of the spinal cord." South African Medical Journal, Vol. 51, No. 26, 1977, pp. 961-64.
- Roth, E. J., et al. "Traumatic cervical Brown-Sequard and Brown-Sequard-plus syndromes: The spectrum of presentations and outcomes." Spinal Cord, Vol. 29, No. 9, 1991, pp. 582-89.
- Oller, D. W., and S. Boone. "Blunt cervical spine Brown-Séquard injury. A report of three cases." The American Surgeon, Vol. 57, No. 6, 1991, pp. 361-65.
- Edwards, A., and R. Andrews. "A case of Brown-Sequard syndrome with associated Horner's syndrome after blunt injury to the cervical spine." Emergency Medicine Journal, Vol. 18, No. 6, 2001, pp. 512-13.
- Miranda, Pablo, et al. "Brown-Sequard syndrome after blunt cervical spine trauma: Clinical and radiological correlations." European Spine Journal, Vol. 16, No. 8, 2007, pp. 1165-70.
- Choi, Kyeong Bo, et al. "Cervical disc herniation as a cause of brown-séquard syndrome." Journal of Korean Neurosurgical Society, Vol. 46, No. 5, 2009, p. 505.
- Schneider, Steven J., Robert G. Grossman, and R. Nicholas Bryan. "Magnetic resonance imaging of transdural herniation of a cervical disk." Surgical Neurology, Vol. 30, No. 3, 1988, pp. 216-19.
- Finelli, Pasquale F., Norman Leopald, and Seth Tarras. "Brown-Sequard syndrome and herniated cervical disc." Spine, Vol. 17, No. 5, 1992, pp. 598-99.
- Rumana, Christopher S., and David S. Baskin. "Brown-Sequard syndrome produced by cervical disc herniation: Case report and literature review." Surgical Neurology, Vol. 45, No. 4, 1996, pp. 359-61.
- Antich, P. A., et al. "High cervical disc herniation and Brown-Sequard syndrome: A case report and review of the literature." The Journal of Bone and Joint Surgery. British, Vol. 81, No. 3, 1999, pp. 462-63.
- Börm, Wolfgang, and Torsten Bohnstedt. "Intradural cervical disc herniation: Case report and review of the literature." Journal of Neurosurgery: Spine, Vol. 92, No. 2, 2000, pp. 221-24.
- Iwamura, Yuichi, et al. "Cervical intradural disc herniation." Spine, Vol. 26, No. 6, 2001, pp. 698-702.
- Mastronardi, Luciano, and Andrea Ruggeri. "Cervical disc herniation producing Brown-Sequard syndrome: Case report." Spine, Vol. 29, No. 2, 2004, pp. E28-E31.
- Wang, Chih-Hsiu, Chun-Chung Chen, and Der-Yang Cho. "Brown-Sequard syndrome caused by cervical disc herniation." Mid-Taiwan Journal of Medicine, Vol. 11, No. 1, 2006, pp. 62-66.
- Sathirapanya, Pornchai, et al. "Brown-Séquard syndrome from cervical disc herniation: A case report and review of literature." Neurology Asia, Vol. 12, No. 1, 2007, pp. 65-67.
- Rustagi, Tarush, et al. "Cervical disc herniation causing Brown-Séquard's syndrome: A case report and literature review." Case Reports in Orthopedics, Vol. 2011, 2012.
- Yeung, Jacky T., John I. Johnson, and Aftab S. Karim. "Cervical disc herniation presenting with neck pain and contralateral symptoms: A case report." Journal of Medical Case Reports, Vol. 6, No. 1, 2012, pp. 1-4.
- Roda, José M., et al. "Intradural herniated cervical disc: Case report." Journal of Neurosurgery, Vol. 57, No. 2, 1982, pp. 278-80.
- Eisenberg, Robert A., Alfonso M. Bremer, and H. Martin Northup. "Intradural herniated cervical disk: A case report and review of the literature." American Journal of Neuroradiology, Vol. 7, No. 3, 1986, pp. 492-94.