Case Report - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 6
Chronic Juvenile Recurrent Parotitis in an 8-Year-Old Patient: A Case Report
Akriti Shrestha1*, Sabi Rana1, Kolaj Kattel2, Astika Shrestha3 and Sagar Devkota42Department of Otorhinolaryngology and Head and Neck Surgery, Abdul Samad Memorial Hospital, Maldives
3Department of Internal Medicine, Grandy International Hospital, Kathmandu, Nepal
4Department of Anesthesiology and Critical Care, Kulhudhuffushi Regional Hospital, Kulhudhuffushi, Maldives
Akriti Shrestha, Department of Otorhinolaryngology and Head and Neck Surgery, Kulhudhuffushi Regional Hospital, Kulhudhuffushi, Maldives, Email: akriti.shrestha4.as@gmail.com
Received: 27-May-2023, Manuscript No. ijmrhs-23-100384; Editor assigned: 31-May-2023, Pre QC No. ijmrhs-23-100384(PQ); Reviewed: 13-Jun-2023, QC No. ijmrhs-22-100384(Q); Revised: 18-Jun-2023, Manuscript No. ijmrhs-23-100384(R); Published: 30-Jun-2023
Abstract
Background: Chronic Juvenile Recurrent Parotitis (CJRP), a nonsuppurative, nonobstructive, recurrent inflammation of the parotid gland, is a rare cause of parotid swelling in children presenting with multiple episodes of swelling over years, often accompanied by fever, with or without pain or discomfort. This work aimed to present a case report that highlights the signs and symptoms of this unusual condition and focuses on the value of ultrasonography to aid in the diagnosis. Methodology: A 8 years old female presented to the ENT outpatient department with complaints of multiple episodes of bilateral painful swelling below the ears for the past 1 year and had no significant past medical or surgical history. Discussion: On examination, the child was afebrile with bilateral parotid swelling, more on the right side, both sides being smooth, firm in consistency, and non-tender. All her blood investigations were within normal limits. Ultrasonography of the parotid glands revealed bilateral coarse, heterogeneous internal echogenicity and nodular hypoechoic areas suggesting sialectasis, scattered parenchymal calcifications, and fibrous septa (more on the left side). A diagnosis of bilateral chronic parotitis was made. The child was treated with an analgesic, antipyretic, antibiotic (co-amoxiclav), good oral hygiene, mouthwash, and adequate fluid intake during each episode. She has been asymptomatic for the last 15 months and is under regular follow-up. Conclusion: Even though rare, bilateral recurrent parotid swelling in children can be chronic juvenile recurrent parotitis and needs early diagnosis and prompt treatment.
Keywords
Bilateral Parotid Swelling (BPS), Chronic Juvenile Recurrent Parotitis (CJRP), Ultrasonography
Introduction
Chronic Juvenile Recurrent Parotitis (CJRP) is a nonsuppurative, nonobstructive, recurrent inflammation of the parotid gland in young children. CJRP is a rare cause of parotid enlargement, though bilateral inflammatory parotid swellings are common in children [1]. The etiopathology of CJRP is unclear, although underproduction of saliva, and congenital malformation of the parotid glands leading to retrograde infection, allergy, immunodeficiency, and autoimmune diseases, have been considered [2-5]. In most cases, the episodes begin between 3 years to 6 years of age and subside by the age of 10 years to 15 years. Although it tends to resolve spontaneously after puberty, all children must be screened for lymphoma, autoimmune diseases mainly Sjogren’s syndrome or sarcoidosis, and immunodeficiency including human immunodeficiency virus and tuberculosis. CJRP is a rare condition characterized by multiple episodes of swelling over years, often accompanied by fever, with or without pain or discomfort. It is usually unilateral but can occur bilaterally also. Here, we present a case of an 8-year-old girl with bilateral chronic juvenile recurrent parotitis. This case report has been reported taking into consideration the SCARE 2020 criteria [5].
Method
We reported this case following the updated consensus-based Surgical Case Report (SCARE) Guidelines [5].
Case Presentation
An 8-year-old girl presented to the ENT outpatient department with multiple episodes of bilateral painful swelling below the ears for the past 1 year. The swelling was more prominent on the right side as compared to the left and was usually associated with pain, fever, and malaise without any pus discharge. She had five such episodes in the last year with each episode lasting for 7 days to 14 days. Her last episode lasted for 10 days. The child did not encounter any symptoms like headache, vomiting, neck stiffness, lower abdominal pain, lower back pain, or burning micturition during any of the episodes. On examination, the child was afebrile with bilateral parotid swelling, more on the right side, with both sides being smooth, firm in consistency, and non-tender (Figure 1).
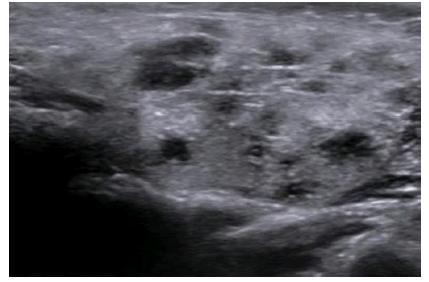
Pressure over the gland did not cause any purulent discharge from the parotid duct. There was no history of dental caries, weight loss, night sweats, hemoptysis, dryness of eyes, dryness of mouth, altered taste, increased salivation, joint pain or swelling, and skin rashes suggestive of autoimmune disorder during any episodes. There was no history of exposure to tuberculosis, no family history of recurrent parotid swelling, tuberculosis, or any autoimmune disorder. Her serum amylase level was on the higher side during all episodes except in the last episode. However, blood counts, erythrocyte sedimentation rate, c-reactive proteins, serum lipase, and serum immunoglobulin levels were within normal range. Screening for Human Immunodeficiency Virus (HIV) serology, rheumatoid factor, antibodies for anti-Ro and anti-La for Sjogren's syndrome, and AFB for tuberculosis were negative. Ultrasound of both parotid glands demonstrated coarse, heterogeneous internal echogenicity and nodular hypoechoic areas suggesting sialectasis, scattered parenchymal calcifications, and fibrous septa (Figure 2). Findings were more prominent on the left side.
A diagnosis of bilateral chronic parotitis was made. The child was treated with an analgesic, antipyretic, antibiotic (co-amoxiclav), good oral hygiene, mouthwash, and adequate fluid intake during each episode. During the last episode, in addition to the above treatment measures, massage of parotid glands, application of heat to the affected area, and encouraging sugar-free chewing gum and sour candy to stimulate the flow of saliva were given. She has remained symptom-free for 15 months and is under regular follow-up.
Discussion
Chronic juvenile recurrent parotitis is the second most common cause of parotitis in childhood, only after mumps [6, 7]. CJRP is often synonymously referred to in the literature as Infantile Chronic Recurrent Parotitis (ICRP) or Juvenile Recurrent Parotitis (JRP). The juvenile form of recurrent parotitis was first described by von Reuss [8,9]. The disease frequently affects males but higher distribution in females has been found when symptoms appear later [10]. The etiology of CJRP is reported as multifactorial. Genetic factors, familial causes with autosomal dominant inheritance, autoimmune causes like Sjogren’s disease, viral etiology like mumps, allergy, and IgG3 immunodeficiency have all been implicated as possible causes of CJRP [11]. But there is no definite evidence in support of any of these causes. However, the main cause postulated to explain the pathogenesis of CJRP is decreased salivary production causing inadequate salivary outflow which further facilitates infection. Pathological studies reveal several structural changes in the affected parotid gland, while there is still a debate about whether these are the primary abnormalities or the result of multiple episodes of parotitis
CJRP can be provisionally diagnosed by clinical symptoms and examination which may be aided by radiological investigations like ultrasonography and conventional sialography [11]. Clinical symptoms of JRP include recurrent parotid inflammation with swelling and pain associated with fever which usually lasts 2 days to 7 days. In 90% of the patients, the symptoms resolve spontaneously by puberty. In a few severe cases, there is progression leading to the destruction of the glandular parenchyma with a diminution of its functionality by 50% to 80% [12].
Ultrasonography features of CJRP include multiple hypoechoic lesions with gland enlargement and lymph nodal enlargement [1]. Studies have suggested that hypoechoic areas and anechoic areas in parotid are consistent with ductal ectasia and lymph node enlargement [13]. The ecstatic ducts are usually 1 mm to 2 mm in diameter and typically have a white appearance of the ductal layer without healthy blood vessel coverage when compared with a normal gland [14]. This aspect is believed to be characteristic of CJRP. Sialectasis was previously diagnosed by sialography, but ultrasound has superseded this technique [12]. Hence, clinical examination and sonography as a combination are sensitive tools for the diagnosis of CJRP.
CJRP is a self-limiting condition with unknown incidence, occurring at any age during childhood. In most cases, symptoms disappear in puberty without the need for invasive treatment. Because of this, doctors are conservative in their approach to treatment. Analgesics, attention to good oral hygiene, massage of the parotid gland, warmth, and use of chewing gum and sialogogic agents are helpful. Antibiotic treatment during attack is often proposed to prevent additional damage to the glandular parenchyma while low-dose prophylactic antibiotics have been recommended when an immunoglobulin-A deficiency is observed [15]. It is only in severe cases that invasive treatments are considered. Nahlieli et al performed duct probing with lavage, dilation, and hydrocortisone injection via sialendoscopy with a resolution of symptoms and a very low recurrence rate on follow-up [14]. More aggressive treatment is justified only for those patients with persistent problems and includes parotid duct ligation, parotidectomy, or tympanic neurectomy but all have unsatisfactory results [11].
Conclusion
Although CJRP is a rare disease, early identification, regular follow-up, and early management are required for patients with bilateral parotid swelling and we should be aware of this disease and treatment options. Some signs and symptoms may guide the diagnosis but ultrasonography finds its place to confirm it.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Source of Funding
None.
Ethical Approval
Not applicable (A case report does not require ethical approval at our institute).
Consent
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author Contributions
Shrestha A, Rana S, and Kattel K conceptualized the study. Shrestha A and Rana S were in charge of the case and they reviewed and edited the manuscript. Kattel K, Shrestha A, and Devkota S reviewed and edited the original manuscript.
Research Registration
Not applicable.
Provenance and Peer Review
Not commissioned, externally peer-reviewed.
References
- Gadodia, A., et al. "Bilateral parotid swelling: a radiological review." Dentomaxillofacial Radiology, Vol. 40, No. 7, 2011, pp. 403-14.
Google Scholar Crossref - Cimaz, Rolando, et al. "Primary Sjogren syndrome in the paediatric age: a multicentre survey." European journal of paediatrics, Vol. 162, 2003, pp. 661-65.
Google Scholar Crossref - Alp, H., et al. "Recurrent parotitis as a first manifestation in a child with primary Sjogren's syndrome." West Indian Medical Journal, Vol. 60, No. 6, 2011, pp. 685-87.
Google Scholar - Kevin, B., et al. "Recurrent parotitis as a presentation of primary pediatric Sjogren syndrome." Pediatrics, Vol. 129, No. 1, 2012, pp. 179-82.
Google Scholar Crossref - Agha, Riaz A., et al. "The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines." International Journal of Surgery, Vol. 84, 2020, pp. 226-30.
Google Scholar Crossref - Ericson, Sune, Birgitta Zetterlund, and Jan Ohman. "Recurrent parotitis and sialectasis in childhood: clinical, radiologic, immunologic, bacteriologic, and histologic study." Annals of Otology, Rhinology & Laryngology, Vol. 100, No. 7, 1991, pp. 527-35.
Google Scholar Crossref - Chitre, V. V., and Premchandra, D. J. "Recurrent parotitis." Archives of disease in childhood, Vol. 77, No. 4, 1997, pp. 359-63.
Google Scholar Crossref - Bhattarai, M., and P. T. Wakode. "Recurrent parotitis in children." Journal of Indian Association of Pediatric Surgeons, Vol. 11, No. 4, 2006, p. 246.
Google Scholar Crossref - Von Reuss, A. "Uber chronische Erkrankungen der Parotis im Kindesalter." Jahrb. f. Kinderheilk, Vol. 70, 1909, pp. 161-78.
Google Scholar - Katz, Philippe, Dana M. Hartl, and Agnès Guerre. "Treatment of juvenile recurrent parotitis." Otolaryngologic Clinics of North America, Vol. 42, No. 6, 2009, pp. 1087-91.
Google Scholar Crossref - Iro, Heinrich, and Johannes Zenk. "Salivary gland diseases in children." GMS current topics in otorhinolaryngology, head and neck surgery, Vol. 13, 2014.
Google Scholar Crossref - Leerdam, C. M., et al. "Recurrent parotitis of childhood." Journal of paediatrics and child health, Vol. 41, No. 12, 2005, pp. 631-34.
Google Scholar Crossref - Nozaki, H., et al. "Ultrasonographic features of recurrent parotitis in childhood." Pediatric radiology, Vol. 24, 1994, pp. 98-100.
Google Scholar Crossref - Oded, N., et al. "Juvenile recurrent parotitis: a new method of diagnosis and treatment." Pediatrics, Vol. 114, No. 1, 2004, pp. 9-12.
Google Scholar Crossref - Tamas, F., et al. "Selective IgA deficiency in children with recurrent parotitis of childhood." The Pediatric infectious disease journal, Vol. 24, No. 5, 2005, pp. 461-62.
Google Scholar Crossref