Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
Clinico-Radiological Profile of Pulmonary Tuberculosis with Diabetes Mellitus among Patients Attending to a Tertiary Care Teaching Hospital
Narayan Mood1*, Mouleeswara Kumar Tamma2, Surendra Babu Darivemula3 and Sri Krishna Kishore Advanapu12Department of General Medicine, Maharaja Institute of Medical Sciences, Vizianagaram, Andhra Pradesh, India
3Department of Community Medicine, ESIC Medical College & Hospital, Hyderabad, Telangana, India
Narayan Mood, Department of Pulmonary Medicine, ESIC Medical College & Hospital, Hyderabad, Telangana, India, Email: narayana5005@gmail.com
Received: 28-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Background: Diabetic patients are at higher risk of developing tuberculosis and the bi-directional association is a major concern for clinicians. The knowledge of the spectrum of disease in the Indian context is limited. Methods: A cross-sectional study was conducted on patients diagnosed with pulmonary tuberculosis and diabetes mellitus attending a tertiary care hospital in urban Telangana, India. Results: A total of 100 patients with tuberculosis were included in the study. The highest number of cases of tuberculosis with diabetes is prevalent in the 5th decade of their life. Nearly 80% of cases of tuberculosis are from urban areas and there is no significant difference in the association of diabetes with tuberculosis between urban and rural populations. More number of tuberculosis patients with diabetes (60%) are overweight compared to those without diabetes (20%). Lung infiltrations are the most common radiological presentation in both groups with a higher incidence in diabetic patients (82%) compared to non-diabetic tuberculous patients (62%). A higher number of acid-fast bacilli was observed on sputum microscopy in diabetic tuberculosis patients (3+ in 56%) while the majority of non-diabetic tuberculosis patients fall into the 1+ and 2+ categories. Patients with diabetes mellitus who consume a carbohydrate-rich diet, smoke, and consume alcohol had a higher association with tuberculosis. Conclusion: People with age more than 30 years were at higher risk for dual epidemic (DM-TB). Symptomatology was similar in both groups except that hemoptysis was observed more in patients with diabetes and TB. Family history of diabetes is an important clue for active DM screening in all TB patients and will help in the early detection of diabetes. Strategies are needed to ensure that optimal care is provided to patients with both diseases.
Keywords
Tuberculosis, Diabetes mellitus, Disease spectrum, Clinico-radiological presentation, Etiological patterns
Introduction
One of the major causes of mortality and morbidity globally is Tuberculosis (TB) an infectious disease. The risk of developing active TB is three-fold higher in those patients having Diabetes Mellitus (DM) in comparison to nondiabetic patients [1]. The bidirectional association between Tuberculosis (TB) and Diabetes Mellitus (DM) is currently one of the major concerns for clinicians, as DM affects the disease presentation and clinical outcome of TB and vice versa [2]. The main reason that may lead to the development of TB among diabetes patients is a weak immune system because of chronic disease, which places the population at higher risk from latent infection, it is noted that cellular immunity that is weakened, alveolar macrophages dysfunction, interferon-gamma low levels, micro-angiopathy of lungs, and deficiency of micronutrients play a significant role in the occurrence of tuberculosis in diabetic patients [3-5].
The spectrum of tuberculosis and DM is daunting. As result patients are usually subjected to inappropriate invasive and costly investigation for its evaluation. Therefore, knowledge of the spectrum of disease in the context of the Indian population will be valuable. As there are no studies available in our settings, clinical and radiological profile of tuberculosis and diabetes mellitus is in high need for proper evaluation and management of the patients, hence this study was taken up to know the clinical and radiological profile of pulmonary tuberculosis and diabetes mellitus, understand various modes of presentation, etiological pattern, clinical-radiological correlation of the study population.
Materials and Methods
Study Design
This is a cross-sectional study conducted on patients diagnosed with pulmonary tuberculosis and diabetes mellitus attending the department of pulmonary medicine in ESIC Medical College, Hyderabad during the period from May 2019 to November 2019.
Study Site and Data Collection
Data was collected using a structured questionnaire to elicit demographic and clinical variables including the history of diabetes mellitus in all patients who are diagnosed with pulmonary tuberculosis at ESIC Medical College, Hyderabad. Written and informed consent was taken before enrolling in the study. Institutional Ethics Committee approval was taken before the conduct of the study.
The assessment included the patient’s demographic profile, clinical features, chest X-ray features, sputum for Acid Fast Bacilli (AFB), HIV status and HbA1c, Fasting blood sugar, postprandial blood sugar levels, History of comorbidities, drug history, and any significant history was also noted.
All patients with history and clinical features suggestive of pulmonary tuberculosis subjected to chest x-ray and sputum for Acid Fast Bacilli (AFB) with Fluorescent staining by auramine rhodamine stain at the designated microscopy centre at our hospital. Culture and drug susceptibility tests were done for retreatment cases to rule out drug-resistant tuberculosis. Based on results sputum positive and sputum negative radiologically positive pulmonary tuberculosis cases were enrolled for the study and all such patients were screened by Enzyme-Linked Immune-Sorbent Assay (ELISA) test for HIV status.
From all the patients with pulmonary tuberculosis blood samples were collected to measure the random blood sugars, fasting, and post-lunch blood sugar HbA1c.
Inclusion Criteria
• The patients with pulmonary tuberculosis and diabetes mellitus with age 18 years and above as cases
• The patients with pulmonary tuberculosis without diabetes mellitus with age 18 years and above controls
• Patients willing to give written informed consent
Exclusion Criteria
• Pulmonary tuberculosis patients with age <18 years
• Patients with HIV
• Patients on steroids or any other form of immunosuppressive therapy
• Patients not willing for regular follow up
• All extrapulmonary tuberculosis patients
• History of known close contacts of drug-resistant pulmonary tuberculosis and already diagnosed drug-resistant pulmonary tuberculosis patients
Statistical Analysis
The software used is SPSS v21 for data analysis. The categorical variable data was represented as frequencies and percentages. The Chi-square test is used to test significance. A p-value less than 0.05 is considered statistically significant.
Observations and Results
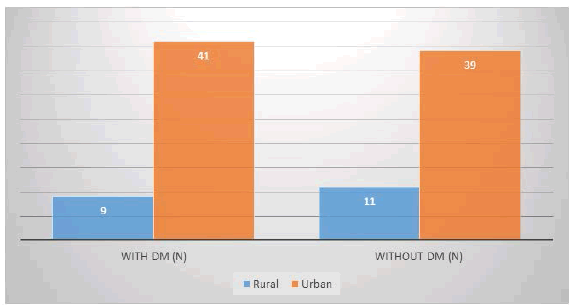
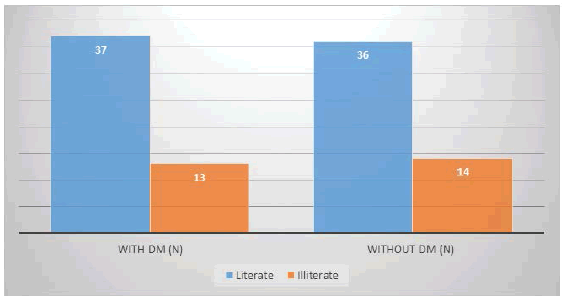
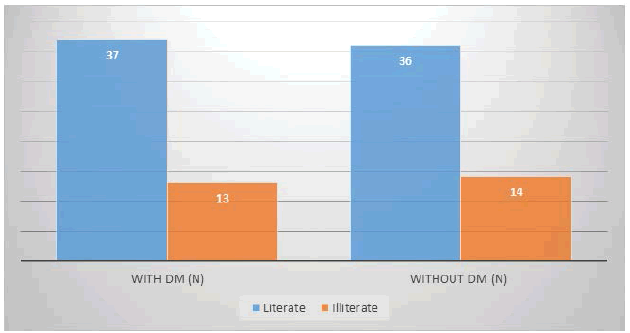
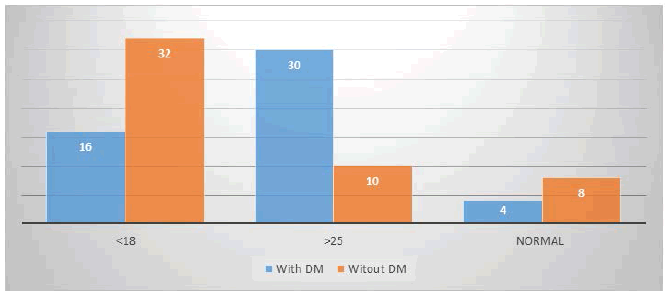
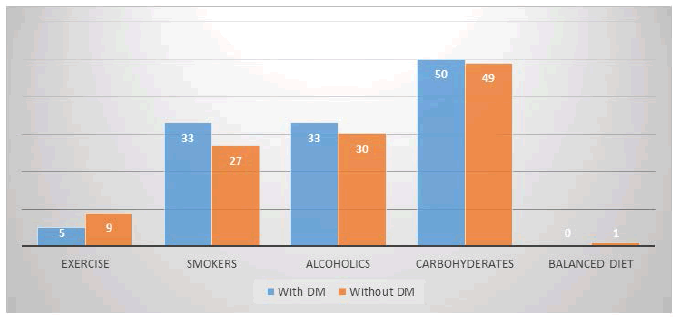
The age group of the patients in the current study varied from 18 years to 70 years. A total of 100 patients with tuberculosis were included in the study, of which 50 patients with diabetes were included in the study group and 50 patients without diabetes in the control group. It was observed that TB does occur in all age groups, but the highest number of cases of TB with DM were recorded in the 5th decade, and TB without DM was predominant in the 3rd decade of life (Table 1). This study group consisted of 40% males with DM and 38% of males without DM and 10% females with DM and 12% females without DM (Table 2). The mean age of males with DM is 40.82 ± 11.783 and without DM is 31.42 ± 9.420 and females with DM is 37.10 ± 8.920 and without DM is 28.23 ± 7.451 (Table 3). Out of a total of 50 patients with DM 41 hails from an urban area and 9 from a rural area and of those 50 patients without DM 39 hails from urban and 11 from a rural area. There was urban predominance over rural in both cases with an urban to the rural ratio of approximately 4:1 (Graph 1). Out of a total of 50 patients with DM 37 (74%) are literate and 13 (26%) are illiterate and of the 50 patients without DM 36 (72%) are literate and 14 (28%) are illiterate. This indicates that tuberculosis is predominant in literate than illiterate (Graph 2). Less number of PTB patients with DM patients 16 (32%) are underweight as compared to the PTB patients without DM 32 (64%). Overweight is more in cases of TB with DM 30 (60%) compared to controls 20% (Graph 3). The most common symptom in patients with or without DM is cough followed by expectoration and fever. Loss of appetite and loss of weight is almost equal in both groups and the least common symptom is hemoptysis (Graph 4). 32% of Diabetic patients have a family history and 22% of controls also have a family history of DM (Table 4). Most of the patients (44%) had diabetes mellitus for 6 to 10 years of range (Table 5). The majority of the patients with DM are on oral hypoglycemic agents (86%). The history of pulmonary tuberculosis in controls is 18% and in patients with diabetes mellitus is 22% (Table 6). The most common radiological presentation in both groups is infiltrations, but infiltration is more common in patients with DM (82%) when compared with non-Diabetic patients (62%). This is followed by cavitary lesions which are more in the diabetic group compared to the control group. The least common are lymphadenopathy in the diabetic and bronchiectasis in the control group (Table 7). Right upper zone involvement is more common in both cases (42) and controls (29) followed by left upper zone, i.e. tuberculous bacilli have more predilection to upper lobe, least predilection to lower lobe. Multiple involvements are more common in non-diabetic patients. Middle zone involvement is more common in diabetic patients than too on the right side (Table 8). Two sputum samples (sample A and sample B) were studied for Acid Fast Bacilli (AFB) and the severity of the disease based on sputum microscopy is more inpatient with diabetes mellitus compared to controls i.e. 56% of the diabetic patients are with 3+ compared to non-diabetic patients where 3+ cases are only 3% in sample A. Nondiabetic patients are mainly falling into 1+ and 2+ category (Table 9). Sample B also shows that the severity of the disease 3+ is more with diabetes mellitus than non-diabetes (Table 10). Smoker and alcoholics with diabetes have a higher chance of associating with tuberculosis than non-smoker and non-alcoholic and those with DM who consume a carbohydrate diet are at increased risk of tuberculosis than those who take a balanced diet (Graph 5).
| Age (years) | TB with DM n (%) | TB without DM n (%) | Total n (%) |
|---|---|---|---|
| 18-20 | 0 (0%) | 1 (2%) | 1 (1%) |
| 21-30 | 0 (0%) | 14 (28%) | 14 (14%) |
| 31-40 | 9 (18%) | 13 (26%) | 22 (22%) |
| 41-50 | 28 (56%) | 11 (22%) | 39 (39%) |
| 51-60 | 10 (20%) | 5 (10%) | 15 (15%) |
| 61-70 | 3 (6%) | 6 (12%) | 9 (9%) |
| Total | 50 (100%) | 50 (100%) | 100 (100%) |
| TB: Tuberculosis, DM: Diabetes Mellitus | |||
| Sex | No of cases (n) | Percentage (%) |
|---|---|---|
| Male with DM | 40 | 40% |
| Male without DM | 38 | 38% |
| Female with DM | 10 | 10% |
| Female without DM | 12 | 12% |
| Total | 100 | 100% |
| DM: Diabetes Mellitus | ||
| Sex | Mean | Standard deviation (±) |
|---|---|---|
| Male with DM | 40.82 | 11.783 |
| Male without DM | 31.42 | 9.42 |
| Female with DM | 37.1 | 8.92 |
| Female without DM | 28.23 | 7.451 |
| DM: Diabetes mellitus | ||
| Family history | With DM n (%) | Without DM n (%) |
|---|---|---|
| Present | 16 (32%) | 11 (22%) |
| Absent | 34 (68%) | 39 (78%) |
| TOTAL | 50 (100%) | 50 (100%) |
| DM: Diabetes mellitus | ||
| Duration (years) | No. of subjects (n) | Percentage% |
|---|---|---|
| 1-5 | 16 | 32% |
| 6-10 | 22 | 44% |
| 11-15 | 8 | 16% |
| >15 | 4 | 8% |
| Total | 50 | 100% |
| History of PTB | With DM n (%) | Without DM n (%) |
|---|---|---|
| Present | 11 (22%) | 9 (18%) |
| Absent | 39 (78%) | 41 (82%) |
| Total | 50 (100%) | 50 100%) |
| PTB: Pulmonary Tuberculosis, DM: Diabetes Mellitus | ||
| Presentation | With DM n (%) | Without DM n (%) |
|---|---|---|
| Cavitary lesions | 33 (66%) | 27 (54%) |
| Infiltrations | 41 (82%) | 31 (62%) |
| Consolidation | 11 (22%) | 10 (20%) |
| Pleural effusion | 2 (4%) | 7 (14%) |
| Lung abscess | 4 (8%) | 0 (0%) |
| Bronchiectasis | 2 (4%) | 1 (2%) |
| Pneumothorax | 1 (2%) | 2 (4%) |
| DM: Diabetes Mellitus | ||
| Zones | With DM (n) | Without DM (n) |
|---|---|---|
| Right upper zone | 42 | 29 |
| Left upper zone | 26 | 25 |
| Right middle zone | 22 | 15 |
| Left middle zone | 6 | 4 |
| Right lower zone | 0 | 0 |
| Left lower zone | 0 | 2 |
| Multiple | 15 | 22 |
| DM: Diabetes Mellitus | ||
| GRADE | With DM n (%) | Without DM n (%) |
|---|---|---|
| Scanty | 2 (4%) | 4 (8%) |
| 1+ | 3 (6%) | 17 (34%) |
| 2+ | 17 (34%) | 26 (52%) |
| 3+ | 28 (56%) | 3 (6%) |
| AFB: Acid Fast Bacilli, DM: Diabetes Mellitus | ||
| GRADE | With DM n (%) | Without DM n (%) |
|---|---|---|
| Scanty | 4 (8%) | 1 (2%) |
| 1+ | 17 (34%) | 11 (22%) |
| 2+ | 8 (16%) | 27 (54%) |
| 3+ | 21 (42%) | 11 (22%) |
| AFB: Acid Fast Bacilli, DM: Diabetes Mellitus | ||
Discussion
In the present study, the age group varied from 18 to 70 years of age and the highest number of TB with DM occurred in the 5th decade of life (56%) and TB without DM occurred in the 3rd decade of life (28%). TB with DM occurred in the 5th decade of life which is similar to the study conducted by Ullah H, et al. who reported 31% susceptibility between 41 to 50-year age group [6]. In another study conducted by Kouismi, et al. found that TB with diabetes mellitus prevailed more in the 6th decade of life [7].
In the present study tuberculosis with diabetes and without diabetes mellitus most commonly occurred in males 48% and 38% respectively compared to females which are 10% and 12% respectively which is similar to the study conducted by Kouismi, et al. where a male in both groups is 66% and 68% respectively and females 33% and 32% respectively [7]. Another study conducted by Mohapatra AK, et al. also found male predominance 85% compared to females [8].
In the present study mean age of males with DM is 40.82 ± 11.783 and without DM is 31.42 ± 9.420 and females with DM is 37.10 ± 8.920 and without DM is 28.23 ± 7.451. The mean age of a patient with DM is 38.96 ± 10.351 and without DM is 29.82 ± 13.145 whereas, in the study conducted by Kouismi H, et al. the mean age of a patient with diabetes is 54.1 ± 15.1and without DM is 41.34 ± 16.7 [7]. In another study conducted by Ogbera AO, the mean age of a patient with DM is 40.9 and without DM is 34.9 [9]. Our study is similar to both studies.
In the present study out of a total of 50 patients with DM 41 hails from an urban area and 09 hails from a rural area and another 50 patients without DM 39 hails from urban and 11 from a rural area. There is no significant difference in the occurrence of tuberculosis among the patient with DM and without DM in comparison with the residence. The present study is similar to the study conducted by Mohapatra AK, et al. where they also found no significant difference in the occurrence of tuberculosis in both the groups based on residence [8].
In the present study out of a total of 50 patients with DM 74% are literate and 26% are illiterate and another 50 patients without DM 72% are literate and 28% are illiterate. In a study conducted by Ogbera AO, 640 (16%) had received tertiary education; 2480 (62%) secondary education; 680 (17%) primary education; and 200 (5%) were illiterate which means 95% of patients with tuberculosis in both groups are literate and 5% of patients are illiterate which conclude that tuberculosis occurred more common in literate than illiterate which is similar to the present study [9].
In the present study, the percentage of underweight patients are more in TB without DM group (64%) compared to TB with DM group (32%). But the percentages of people who are overweight are more in TB with DM (60%) compared to TB without DM (20%). Ruslami R, et al. suggested that compared to non-DM patients, TB patients with DM usually have a higher body weight [10]. In a recent study from West Africa, Balde NM, et al., 23% of TB-DM patients were obese (BMI >30 kg/m2), compared with 3% of non-diabetic patients [11]. The present study results are similar to the study conducted by Ruslami R, et al. and Balde NM, et al. [10,11].
Comparison of Symptoms
In the present study, the most common symptom in patients with or without DM is cough followed by expectoration and fever. Loss of appetite and loss of weight is almost equal in both groups and the least common symptom is hemoptysis. Cough is the major symptom in all the studies followed by expectoration, fever, and hemoptysis. The present study is similar to the study by Kouismi H, et al. and Mohapatra AK, et al. [7,8].
In the present 32% of patients with DM has a positive family history of diabetes mellitus and 22% without DM has positive family history whereas in a study conducted by Ogbera AO 26.3% of patients with DM has a positive family history and 5.5% of patients without DM has a positive family history [9]. In the present study family history of diabetes mellitus is more in TB-DM (32%) group compared to TB without DM (22%). Similar results were seen in Vasudevan K, et al. and Ogbera AO studies showing significant association of family history of DM seen in TB-DM group [9,12]. So, family history of DM in pulmonary TB patients may be considered as a risk factor and screen for DM in all such patients for early and better management of TB-DM.
From the present study, it is evident that most of the patients (44%) had diabetes mellitus for 6 to 10 years of range with an average period of 8 years duration. Kouismi H, et al. reported an average period of 7 years of DM in 90% of patients which is similar to the present study [7].
In the present study, 14% of patients are on insulin and 86% of patients are on OHA (Oral Hypoglycemic Agents). In the study conducted by Mohapatra AK, et al. 27.5% of patients are on insulin therapy and 75.2% of the patients are on OHA which is similar to the present study [8].
In the present study, a history of pulmonary tuberculosis in patients with DM was reported in 22% and 18% of those without DM, whereas the study by Kouismi H, et al., history of Tuberculosis inpatient with DM was 10% and without DM was 32% [7]. This is contrary to the present study where the history of pulmonary tuberculosis is more in patients with DM. The exact reason for this is not known but could be because of the small study group and shorter duration of the study.
In the present study, the most common presentation in both groups is infiltrations, but infiltration is more common in patients with DM (82%) when compared with non-diabetic patients (62%). This is followed by cavitary lesions which are more in the diabetic group compared to the control group. The least common are pneumothorax in diabetic and bronchiectasis in the control group. The present study is similar to the study conducted by Mohapatra, et al. where the most common radiological presentation was infiltrations followed by cavitation and consolidation in both groups but is more in patients with DM compared to non-diabetic patients [8].
In the present study right upper zone involvement is more common in both cases (42) and controls (29) followed by left upper zone, i.e. tuberculous bacilli have more predilection to upper lobe, least predilection to lower lobe. Multiple involvements are more common in non-diabetic patients. Middle zone involvement is more common in diabetic patients, on the right side. The present study is similar to the study conducted by Kouismi, et al. where an upper zone has the most predilection for pulmonary tuberculosis in both groups [7].
In the present study, the severity of the disease based on sputum microscopy is more inpatient with diabetes mellitus compared to controls i.e. 56% of the diabetic patients showed sputum positivity of 3+ compared to non-diabetic where 3+ cases are only 3%. Nondiabetic patients are mainly falling into the 1+ and 2+ categories. In a study conducted by Venkateswara BR, et al. 27% of patients with DM are with 1+ (mild), 50% are with 2+ (moderate) disease, 2% are with 3+ (advanced) disease [13]. No conclusion could be drawn from the above studies as there is no control group in the study conducted by Venkateswara BR, et al. [13].
In the present study smoker and alcoholics with diabetes have a higher incidence of tuberculosis i.e. 66% (both smoking and alcohol) than non-smoker and non-alcoholic (54% and 60% respectively) and those with DM and consume carbohydrate diet are at increased risk of tuberculosis than those who take balanced diet. In a study conducted by Kouismi, et al. 33% of patients with tuberculosis and DM had a smoking history, and 48% of patients with tuberculosis without DM has a smoking history [7]. He also found that Diabetes was significantly associated with older age, family history of diabetes; consumption of alcohol, smoking, and sputum positivity, risk of tuberculosis is more with an above risk factor. This study is similar to the present study
Limitations of the Study
• The study sample is small and conducted over a limited period
• This was not a multi-centric study and all of the data came from our cohort which was recruited at our hospital
• No long term follow up
• In the present study, MDR pulmonary tuberculosis was not included
• Some behavioural data for instance smoking are self-reported which are subjected to social desirability biases
Conclusion
A high prevalence of diabetes mellitus was seen among pulmonary tuberculosis. Males are more affected than females. People with age more than 30 years were at high risk for dual epidemic (DM-TB). Being overweight is an important risk factor in the development of diabetes among tuberculosis patients. Symptomatology was almost the same in both groups except that hemoptysis was observed more in diabetes with TB. Family history of diabetes mellitus is an important clue for active DM screening in all TB patients. Screening patients with Tuberculosis for fasting blood sugar estimation will help in the early detection of diabetes. Strategies are needed to ensure that optimal care is provided to patients with both diseases.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Funding Source
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Smith, Issar. "Mycobacterium tuberculosis pathogenesis and molecular determinants of virulence." Clinical Microbiology Reviews, Vol. 16, No. 3, 2003, pp. 463-96.
- Dooley, Kelly E., and Richard E. Chaisson. "Tuberculosis and diabetes mellitus: Convergence of two epidemics." The Lancet Infectious Diseases, Vol. 9, No. 12, 2009, pp. 737-46.
- Peleg, Anton Y., et al. "Common infections in diabetes: pathogenesis, management, and relationship to glycaemic control." Diabetes/Metabolism Research and Reviews, Vol. 23, No. 1, 2007, pp. 3-13.
- Stegenga, Michiel E., et al. "Hyperglycemia enhances coagulation and reduces neutrophil degranulation, whereas hyperinsulinemia inhibits fibrinolysis during human endotoxemia." Blood, The Journal of the American Society of Hematology, Vol. 112, No. 1, 2008, pp. 82-89.
- Webb, E. A., et al. "High prevalence of Mycobacterium tuberculosis infection and disease in children and adolescents with type 1 diabetes mellitus." The International Journal of Tuberculosis and Lung Disease, Vol. 13, No. 7, 2009, pp. 868-74.
- Ullah, Hamid, et al. "Frequency of pulmonary tuberculosis in patients presenting with diabetes." Pakistan Journal of Chest Medicine, Vol. 15, No. 4, 2015, pp..
- Kouismi, Hatim, et al. "Pulmonary tuberculosis and diabetes mellitus profile." Integrative Journal of Medical Sciences, Vol. 2, No. 1, 2015, pp. 11-15.
- Mohapatra, Amrut Kumar, Pratima Singh, and Saswat Subhankar. "Study of clinical and radiological profile of pulmonary tuberculosis among patients having diabetes mellitus." International Journal of Advances in Medicine, Vol. 4, No. 5, 2017, pp. 1378-82.
- Ogbera, Anthonia Okeoghene, et al. "Clinical profile of diabetes mellitus in tuberculosis." BMJ Open Diabetes Research and Care, Vol. 3, No. 1, 2015, p. e000112.
- Ruslami, Rovina, et al. "Implications of the global increase of diabetes for tuberculosis control and patient care." Tropical Medicine & International Health, Vol. 15, No. 11, 2010, pp. 1289-99.
- Balde, N. M., et al. "Associated tuberculosis and diabetes in Conakry, Guinea: Prevalence and clinical characteristics." The International Journal of Tuberculosis and Lung Disease, Vol. 10, No. 9, 2006, pp. 1036-40.
- Raghuraman, Soundararajan, et al. "Prevalence of diabetes mellitus among tuberculosis patients in urban Puducherry." North American Journal of Medical Sciences, Vol. 6, No. 1, 2014, p. 30.
- Babu, R. Venkateswara, et al. "A comparative study of diabetes mellitus in pulmonary tuberculosis patients." World Journal of Medical Sciences, Vol. 9, No. 2, 2013, pp. 93-96.