Research Article - International Journal of Medical Research & Health Sciences ( 2024) Volume 13, Issue 3
Comparative Study on Complications of Early Entral Feeding and Nill Per Oral in Mild and Moderate Acute Pancreatitis
Sagar K, Dinesh L Jadhav, Vinay Prasad MH and Dhruva P Holla*Dhruva P Holla, Department of General Surgery, SS Institute of Medical Sciences and Research Center, Davangere, India, Email: dhruva.holla@gmail.com
Received: 19-Aug-2022, Manuscript No. IJMRHS-22-72427; Editor assigned: 22-Aug-2022, Pre QC No. IJMRHS-22-72427; Reviewed: 05-Sep-2022, QC No. IJMRHS-22-72427; Revised: 18-Jan-2023, Manuscript No. IJMRHS-22-72427; Published: 25-Jan-2023
Abstract
Introduction: Acute pancreatitis is a potentially lethal disease with wide variation in severity ranging from mild and self-limiting to a rapidly progressive illness leading to multiorgan failure. In accordance with this wide variation in clinical presentation, the treatment of acute pancreatitis requires a multidisciplinary approach. Mild acute pancreatitis causes disturbance in the homeostatic mechanism of the body is minimal; the treatment is aimed at supporting the native reparative processes of the body. One of the main supportive mechanisms is adequate and safe nutritional supplementation.
Objectives: To assess the occurrence of infective and non-infective complications in cases of acute pancreatitis on early enteral nutrition.
Materials and methods: This is a prospective study conducted on patients who were admitted to SSIMS and RC Davangere with symptoms suggestive of acute pancreatitis from July 2019 to July 2021. Patient with a clinical picture consistent with the diagnosis of acute pancreatitis, along with more than 3 fold elevation of serum amylase and elevated serum lipase were considered to have acute pancreatitis. After initial diagnosis and assessment, patients were duly informed regarding the study and consent was obtained. A 16 gauge nasogastric Ryle’s tube was inserted for all patients included in the study. The feeding patterns were initiated depending upon the severity of acute pancreatitis.
Results: The incidence of infective complications in our study was found to be 2% with none of the infections involving the pancreas itself. The incidence of non-infective complications in our study was found to be 30% with 13% involving the pancreas proper.
Conclusion: Use of early enteral feeding does not influence the incidence of infective and non-infective complications in mild and moderate acute pancreatitis. Early enteral feeding delivers nutrition, in a simpler and more cost effective. Nasogastric and oral feeding reduces the morbidity of the patient by accelerating return to normal activities.
Keywords
Acute pancreatitis, Enteral feeding, Infective complications, Non infective complications
Introduction
Acute pancreatitis has been recognized since antiquity [1,2] but the importance of pancreas and the severity of its inflammatory disorders were realized only in the middle of the 19th century [3].
Acute pancreatitis is a common disorder. The data available are mainly from US and UK. It has been noticed in most of the studies that there is an increase in the disease by a factor of 10 in the past three decades. The reason for the increase is speculated to be due to increase in alcohol abuse and an improved ability to diagnose the disease. But the disease has been a cause of significant morbidity and mortality [4,5]. Both sexes are equally affected.
Since the disturbance in the homeostatic mechanism of the body is minimal, the treatment is aimed at supporting the native reparative processes of the body. One of the main supportive mechanisms is adequate and safe nutritional supplementation. Acute pancreatitis is a hypermetabolic state marked by increased energy expenditure, proteolysis, gluconeogenesis, and insulin resistance. Nutritional supplementation in acute pancreatitis is complicated by these diverse pathophysiologic derangements associated with the disease.
Increasing evidence suggests that enteral feeding maintains the intestinal barrier function and prevents or reduces bacterial translocation from the gut. Furthermore, enteral nutrition eliminates some of the complications of parenteral nutrition such as catheter related sepsis, thrombosis, thrombophlebitis, catheter related embolism and pneumothorax.
Objectives: To assess the occurrence of infective and non-infective complications in cases of acute pancreatitis on early enteral nutrition.
Materials and Methods
Source of data: This prospective study was conducted on patients admitted to SS hospital with symptoms suggestive of acute pancreatitis from July 2019 to December 2009.
Type of study: Prospective study.
Sample size: 50 patients.
Sample size was calculated by using the formula,
Sample size estimation was done using open epi software 2.3.1. At 95% confidence level, 80% is power of the study. According to Petrov SM [6],
The portion of study subjects who tolerated oral fally following nasogastric tube: 50%=P1
The portion of study subjects who tolerated oral fally following nasogastric tube: 5.8%=P2
According to the formula, sample size estimated in each group is 20.
Assuming that there 20% loss of cases 20+4=24 approximately 25.
Hence sample size is 25 in NGT group and 25 in NBM group.
This study was conducted on patients who were admitted to SSIMS AND RC Davangere with symptoms suggestive of acute pancreatitis from July 2019 to July 2021. Patient with a clinical picture consistent with the diagnosis of acute pancreatitis, along with more than 3 fold elevation of serum amylase and elevated serum lipase were considered to have acute pancreatitis. After initial diagnosis and assessment, patients were duly informed regarding the study and consent was obtained. A 16 gauge nasogastric Ryle’s tube was inserted for all patients included in the study. The feeding patterns were initiated depending upon the severity of acute pancreatitis.
Results
The subjects were divided into two categories.
Group A: Patient who were allowed early feeding.
Group B: patients who kept nil per oral and allowed orally later on.
Table 1 shows the demographic and clinical data of the patients. Out of 50 patient’s majority (31) of the patients belonged to age less than 40 years. Out of the 50 patients studied, 40 were males and 10 were females. This may due to the intake of alcohol is more in men. It was seen that majority of the pancreatitis was caused due to alcohol intake.
| Group A | Group B | Total | |
|---|---|---|---|
| Age | |||
| <40 yrs. | 15 (60%) | 16 (64%) | 31 |
| 40-60 yrs. | 10 (40%) | 8 (32%) | 18 |
| >60 yrs. | 0 | 1 (4%) | 1 |
| Gender | |||
| Male | 20 (80%) | 20 (80%) | 40 |
| Female | 5 (20%) | 5 (20%) | 10 |
| Aetiology | |||
| Alcoholic | 19 (76%) | 15 (60%) | 34 |
| Gall Stones | 3 (12%) | 5 (20%) | 8 |
| Idiopathic | 3 (12%) | 5 (20%) | 8 |
| Chief complaints | |||
| Pain Abdomen | 25 (100%) | 25 (100%) | 50 |
| Nausea and Vomiting | 16 (64%) | 12 (48%) | 28 |
| Co-morbidities | |||
| Present | 6 (24%) | 4 (16%) | 10 |
| Absent | 19 (76%) | 21 (84%) | 40 |
| Vitals | |||
| Pulse rate (per min) | 81.20 ± 8.83 | 84.92 ± 7.04 | |
| Respiratory rate (per min) |
17.40 ± 2.68 | 16.40 ± 2.31 | |
| SPO2 | 96.12 ± 3.06 | 95.12 ± 2.58 | |
| Lab investigations | |||
| Serum amylase | 619.96 ± 229.62 U/L | 655.20 ± 230.14 U/L | |
| Serum lipase | 645.96 ± 158.94 U/L | 648.92 ± 143.71 U/L | |
| Imaging modalities | |||
| USG + CT | 9 | 8 | |
| USG | 16 | 17 | |
| Severity of acute pancreatitis | |||
| Mild | 12 (48%) | 10 (40%) | |
| Moderate | 13 (52%) | 15 (60%) | |
Table 1: Demographic details and clinical data of the patients.
The etiology for the pancreatitis was most commonly associated with alcohol in the majority of the patients (34). In 8 patients, the cause was due to gall stones and in 8 patients, the cause was idiopathic. This is in par with most of the studies that state that alcohol is most important risk factor for pancreatitis.
It was noticed that the most common chief complaint was in all the patients was pain abdomen. All the 25 patients had some form of pain abdomen. Some presented with pain and tenderness in the epigastric region and some in the umbilical region and some in the left lumbar region.
It was also observed that majority of the patients (28) presented with the chief complaints of nausea and vomiting associated with pain abdomen. Out of the 50 patients, 10 patients had co morbidities. These comorbities only worsened the prognosis of the patient and had complications.
It was seen that in mild and moderate cases of pancreatitis, the serum amylase and serum lipase ranged from 500-1000 U/l. Out of 50 patients, 17 patients underwent both USG and CT. 33 patients underwent only USG. The reason for not doing CT in all patients was the cost factor.
Categorization of patients based on the severity, 22 patients were found to have mild pancreatitis with a Ransons score of 0 to 1.28 patients were found to have a score 2 to 3 moderate pancreatitis (Table 2). Mild pancreatitis patients tolerated early enteral feeding better than moderate pancreatitis patients.
| Starting of oral feeds (in no of days) | Group A | Group B | P value |
|---|---|---|---|
| 1.44 ± 0.51 | 5.04 ± 0.68 | 0.001 | |
| Severity of acute pancreatitis based on the oral feeds | |||
| Mild pancreatitis | 1.00 ± 0.00 | 4.90 ± 0.57 | 0.001 |
| Moderate pancreatitis | 1.85 ± 0.37 | 5.13 ± 0.74 | 0.001 |
| Average | 1.425 | 5.015 | 0.001 |
| Initiation of normal diet | 5.16 ± 1.11 | 7.08 ± 0.57 | 0.001 |
| Severity of acute pancreatitis based on the normal diet | |||
| Mild pancreatitis | 6.25 ± 1.5 | 6.80 ± 0.42 | 0.001 |
| Moderate pancreatitis | 5.15 ± 0.98 | 7.27 ± 0.59 | 0.001 |
| Average days | 5.7 days | 7.035 days | 0.001 |
Table 2: Association of Acute pancreatitis with respect to enteral feeds.
This table shows, based on the starting of the oral feeds in group A, the feeds were either started on the first day and in group B the feeds were started on mean day 5. Since the p was is less than 0.05, this was found to be statistically significant. Severity of acute pancreatitis based on the oral feeds in the group A, the feeds were started earlier when compared to group B. Since the p was is less than 0.05, this was found to be statistically significant.
By day 5 most of the early feeding group was on normal diet and by day 7, most of the late feeding group was on normal diet. Since the p value is less than 0.05 this is highly significant. Group A tolerated normal feeds much earlier than group B patients. Group A patient could reach the target nutrition earlier than group B Table 3. It is seen that in group A, where patients were taking early feeds, normal diet was started earlier than in those who took delayed feed.
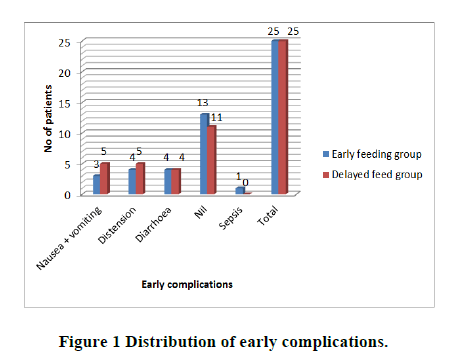
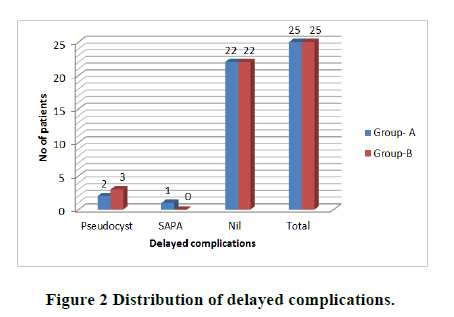
Table 3 shows, most of the patients in the early enteral feeding group had no complications and the most common complication being diarrhoea and ileus, 4 patients, followed by nausea and vomiting. Patients in the delayed group had ileus and nausea and vomiting as the most common complication followed by diarrhoea. One patient in the early enteral group, after feeding went into sepsis and mods and pain became severe. It was seen that 5 patients developed a pseudo cyst after the resolution of acute pancreatitis. 1 patient developed a splenic artery pseudo aneurysm and 44 patients were without any complications (Figures 1 and 2).
| Early complications | ||||
| Early feeding group | Delayed feed group | Total | ||
| Nausea+vomiting | 3 | 5 | 7 | |
| Distension | 4 | 5 | 9 | |
| Diarrhea | 4 | 4 | 8 | |
| Nil | 13 | 11 | 24 | |
| Sepsis | 1 | 0 | 1 | |
| Total | 25 | 25 | 50 | |
| Delayed complications | ||||
| Complications | Group-A | Group-B | Total | |
| Pseudocyst | 2 | 3 | 5 | |
| SAPA | 1 | 0 | 1 | |
| Nil | 22 | 22 | 44 | |
| Total | 25 | 25 | 50 | |
Table 3: Complications of feeds.
Discussion
In the present study had found the incidence of infective complications in our study was found to be 2% with none of the infections involving the pancreas itself. The incidence of non-infective complications in our study was found to be 30% with 13% involving the pancreas proper.
Patients had developed a few complications due to the feeds. Most common was nausea and vomiting followed by distension and diarrhoea. Unlike Eckerwall [7], our patients didn’t have any features of pulmonary insufficiency, pleural effusion, atelectasis, acute fluid collection, pancreatic necrosis mods and death. Olah [8] also had similar complication, SIRS, MODS, pancreatic abscess, pneumonia and death. Abuassai [9] had ARDS, pancreatic necrosis, hyperglycaemia. Manjunath [10] had similar complications, such as nausea, vomiting being the maximum followed by ileus and diarrhoea. Petrov had urinary infection, pneumonia and venous catheter. However, one patient did worsen after taking early enteral feeds and went into sepsis.
Long terms complications, Majority of the cases did not have any complications. 5 cases did develop a pseudocyst and one patient had a splenic artery pseudo aneurysm. There was no significant variation in the complications of pancreatitis in patients who were early fed to those who were fed late. Similar complications were also seen in Petrov, Abuassai, Olah, Maheshwari [11]. No patient in our study had SIRS or MODS or death, which was seen in the above mentioned studies.
Limitations of the present study were sample size was small. Reasons scoring system is now outdated and Atlanta system is now preferred. We couldn’t do a CT scan for all the patients of the study.
Conclusion
Severe cases were excluded from the trial. The patient’s couldn’t be followed up after they had developed complications of the study. The study does not have a control group and does not employ double blinding and randomization.
References
- Fitz RH. Acute pancreatitis: A consideration of pancreatic haemorrhage, hemorrhagic, suppurative and gangrenous pancreatitis and of disseminated fat necrosis. The Boston Medical and Surgical Journal, Vol. 120, No. 8, 1889, pp. 181-187, [Google Scholar]
- Opie EL. The etiology of acute hemorrhagic pancreatitis. Bull Johns Hopkins Hosp, Vol. 12, 1901, pp. 182-185. [Google Scholar]
- Thomson SR, et al. Epidemiology and outcome of acute pancreatitis. The British Journal of Surgery, Vol. 74, No. 5, 1987, pp. 398-401. [Crossref] [Google Scholar] [PubMed]
- Baron TH and Morgan DE. Acute necrotizing pancreatitis. The New England Journal of Medicine, Vol. 340, No. 18, 1999, pp. 1412-1417. [Crossref] [Google Scholar] [PubMed]
- Steinberg W and Tenner S. Acute pancreatitis. The New England Journal of Medicine, Vol. 330, No. 17, 1994, pp. 1198-1210. [Crossref]
- Petrov MS, M Isabel TD Correia and John AW. Nasogastric tube feeding in predicted severe acute pancreatitis: A systematic review of the literature to determine safety and tolerance. Journal of the Pancreas, 2008; Vol. 9, No. 4, 2008, pp. 440-448. [Google Scholar] [PubMed]
- Eckerwall GE, et al. Immediate oral feeding in patients with mild acute pancreatitis is safe and may accelerate recovery-a randomized clinical study. Clinical Nutrition, Vol. 26, No. 6, 2007, pp. 758-763. [Crossref] [Google Scholar] [PubMed]
- Oláh A and Romics L Jr. Enteral nutrition in acute pancreatitis: a review of the current evidence. World Journal of Gastroenterology, Vol. 20, No. 43, 2014, pp. 16123-16131. [Crossref] [Google Scholar] [PubMed]
- Abbasi AH and Abid S. Acute pancreatitis; a comparative study to assess the clinical outcome of acute pancreatitis in relation with major etiologies. The Professional Medical Journal, Vol. 26, No. 4, 2019, pp. 658-662. [Crossref] [Google Scholar]
- Manjunath BD and Abhishek G. Early versus delayed enteral feeding in acute pancreatitis. International Surgery Journal, Vol. 5, No. 3, 2018, pp. 942-945. [Crossref] [Google Scholar]
- Maheshwari R and Subramanian RM. Severe acute pancreatitis and necrotizing pancreatitis. Critical Care Clinics, Vol. 32, No. 2, 2016, pp. 279-290. [Crossref] [Google Scholar] [PubMed]