Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 10
Comparison of the Dosimetric Parameters Obtained with Active Breathing Coordinator (ABC) vs. Free-Breathing (FB) in Radiotherapy for Left- Sided Breast Cancer and Effect of Body Mass Index
Rania Hashem1*, Zaheeda Mulla2, Afraa Abunar2, Ayah Mouais3, Nesreen Awad1, Abdulhameed M Khasim1, Raghdah Khadwardi4, Yosra Badahdah4, Mohammad Attar5, Zayd Jastaniah1 and Reem Ujaimi52Department of Oncology, King Faisal Specialist Hospital and Research Center (KFSHRC), Jeddah, Saudi Arabia
3Department of Medical Physics, King Abdul-Aziz University Hospital, Jeddah, Saudi Arabia
4Department of Medical School, King Abdul-Aziz University Hospital (KAUH), Jeddah, Saudi Arabia
5Department of Radiology, Faculty of Medicine, King Abdul-Aziz University, Jeddah, Saudi Arabia
Rania Hashem, Department of Radiation Oncology, King Abdul-Aziz University Hospital, Jeddah, Saudi Arabia, Email: raniahashem@gmail.com
Received: 28-Sep-2021 Accepted Date: Oct 22, 2021 ; Published: 29-Oct-2021
Abstract
Objective: Radio-toxicity hazard in breast cancer patients becomes a large-scale concern, proportional to the epidemiological figures and the growing population of breast cancer survivors. The present study compared the dosimetric efficacy of Deep Inspiration Breath Hold (DIBH) using Active Breathing Coordinator (ABC) with Free-Breathing (FB) in left-sided breast cancer patients and explored patient-related factors associated with ABC efficacy. Methods: We reviewed the treatment plans for 17 women with left-sided breast cancer, who were treated with external beam radiotherapy using the ABC system, between 2018-2020. CT-simulation images were compared between the two treatment plans including FB and ABC-DIBH. The compared dose-volume parameters included Left Lung V20 (%), Left Lung V5 (%), mean and maximum left lung doses, Heart V25 (%) and Heart V5 (%), and heart mean and maximum lung doses. The effect of body mass index was assessed. Results: The mean (SD) age of the participants was 45.29 (10.14) years, 6 (35.3%) were overweight and 6 (35.3%) were obese. ABC-DIBH was associated with significant relative decrease in all heart parameters including mean (40.9%, p=0.001) and maximum (14.4%, p=0.015) doses, and V25 (68.9%, p<0.001) and V5 (46.4%, p<0.001). However, no significant difference between the two techniques was observed in any of the lung parameters, including left lung mean (p=0.185) and maximum (p=0484) doses, or Left Lung V20 (p=0.122) or V5 (p=0.797). Left Lung V20 (R2=0.28, B=0.43, p=0.029) and Both Lung 20 (R2=0.28, B=0.21, p=0.028) were linearly correlated with BMI under ABC-DIBH, but not FB. Conclusion: The incorporation of DIBH with the ABC system improved heart sparing, which would reduce the radiation-induced cardiac morbidity and mortality; while, on other hand, it may increase lung radio-toxicity in obese patients.
Keywords
Breast cancer, Radiotherapy, Active breathing control, Breath-holding, Radiation technique, Dosimetry
Introduction
Breast cancer continues to be the leading female cancer in Saudi Arabia and worldwide, representing nearly one-third of newly diagnosed cancers in Saudi women [1-3]. External Beam Radiation Therapy (EBRT) has a major place in the management of breast cancer, aiming to improve both local tumour control and patient survival [4,5].
However, the use of EBRT in breast cancer is associated with an increased risk of radiotoxicity to critical organs and structures located near the RT field such as the lungs and the heart [6-9]. Additionally, the recent advances in other cancer control strategies including early detection and improved diagnosis, along with enhanced therapeutic effectiveness, notably the introduction of green therapy by curcumin and nanomaterial-based photo-thermal and photodynamic therapies, enabled a considerable increase of life expectancy notably among young, early diagnosed women [10-14]. This resulted in a growing population of breast cancer survivors, which makes the radio-toxicity issue become a larger-scale concern.
Long-term follow-up studies of patients who underwent left-sided breast RT showed a high incidence of cardiac radiotoxicity, which is associated with increased mortality and morbidity, notably the development of cardiac diseases; whereas such side-effects were less observed in right-sided breast RT [15-17]. A study by Darby, et al., among 2,168 irradiated patients, revealed that the relative risk for ischemic heart disease increased by 7.4% for every 1 Gray (Gy) increment in mean heart dose, the mean radiation dose received by the heart tissue [18]. Such observations highlight the sensitive balance in irradiated breast cancer patients, between achieving effective doses in the target volumes and reducing doses to the heart and critical organs to mitigate the risk of radiotoxicity and the associated morbidity.
To this end, Deep Inspiration Breath-Hold (DIBH) techniques, have been proposed while irradiating left-sided breast cancers to keep the heart away from the breast radiation field, thereby sparing healthy tissues and reducing the mean heart dose. Early clinical experiences with DIBH indicated a significant decrease in irradiated myocardium volume, projecting a reduction of the radiation-induced cardiac morbidity and the associated mortality [19-23]. In our country, however, DIBH is not routinely used either due to lack of resources or the oncologist preference [24].
The present study compared the dosimetric efficacy of DIBH to Free-Breathing (FB) in left-sided breast cancer patients. Findings would provide further evidence on the effectiveness of DIBH in reducing the volume of the irradiated critical organs and to investigate eventual factors that may impact the interindividual feasibility and efficacy of applying this method in our practice and patient population. Ultimately, the study aimed at determining the patient profile that is associated with dosimetrist benefit from the use of DIBH RT.
Methodology
Design and Population
This was a retrospective dosimetric study that reviewed the treatment plans of all women with left-sided breast cancer, who were treated with external beam radiotherapy using the ABC system, between September 2018 and September 2020 at the Radiation Oncology Unit.
Routine Procedure for ABC at our Centre
At the consultation visit, each patient is given a brief overview of the ABC procedure with clarification of its potential benefits. Instructions are given to encourage patients to reach a constant breathing pattern. Patients are requested to practice breath-holding until they maintain a breath-hold for at least 20 seconds and reach a steady breathing pattern. At the time of CT simulation, patients are re-educated on the benefits of the Active Breathing Coordinator (ABC) and with instructions on the DIBH technique. Patients are tested 3 times to hold their breath for at least 20 seconds before proceeding with CT Simulation.
Of note, patients who have difficulty holding their breath for more than 10 seconds are not eligible for this technique. Eligibility criteria for ABC in our centre include all patients with an Eastern Cooperative Oncology Group (ECOG) performance status 0 or 1, no hearing impairments, no previous RT to the breast, and no comorbidities, such as cardiac or pulmonary comorbidities.
CT Simulation for ABC
Patients are simulated in the supine position on the breast board, with arms positioned above the head. Two CTsimulation procedures are performed. The first CT-simulation is performed in FB, and the other is acquired in DIBH, using the Elekta ABC device for monitoring respiratory breath-hold. CT images of 3 mm slice thickness for each patient are obtained and transferred to Monaco treatment planning system version 5.11.
Delineation of Target and Organs at Risks (OARs)
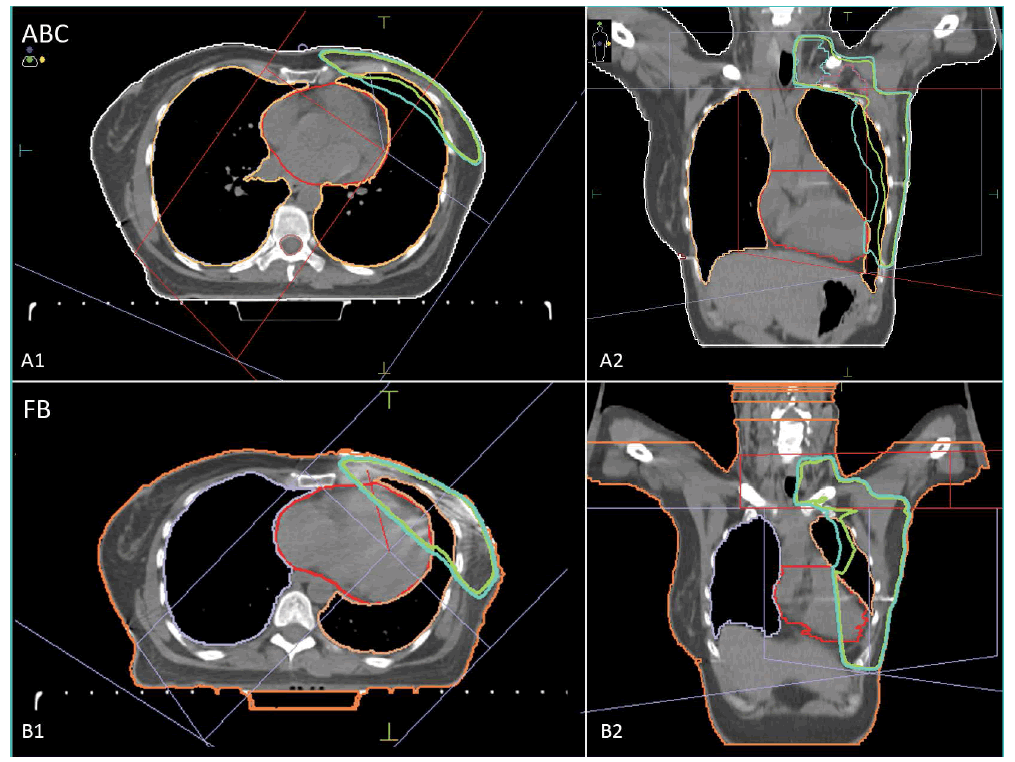
The delineation of the Clinical Target Volume (CTV) is based on the RTOG guidelines, which include the left chest wall and the supraclavicular and axillary level I-III nodes. Planning Target Volume (PTV) includes CTV with a 5 mm margin, in the superior-inferior, anterior-posterior, and left-right directions [25]. The volumes outside the body and inside the lung are excluded from the PTV. CTV, PTV, and the heart volume are delineated by a radiation oncologist, while the ipsilateral and contralateral lung and spinal cord are contoured by a dosimetrist. Treatment planning images for a patient in the axial and coronal plane with ABC and FB are shown in Figure 1, A1 and A2 and B1 and B2, respectively.
Dose-Volume Parameters for this Study
A dosimetric comparison was made between the two treatment plans, ABC and FB, by using Dose-Volume Histograms (DVH). Measurements documented for the two treatment plans included:
• Left Lung V20 (%) and Left Lung V5 (%) corresponding to the percentage of left lung volume receiving 20Gy or more and percentage of left lung volume receiving 5Gy or more radiation, respectively;
• Mean and maximum lung doses;
• Heart V25 (%) and Heart V5 (%) corresponding to the percentage of heart volume receiving 25Gy or more and percentage of heart volume receiving 5Gy or more, respectively;
• Mean and maximum lung doses
Additionally, we measured the Cardiac Contact Distance (CCD) in both the axial (CCDax) and parasagittal (CCDps) planes in only FB CT. CCDax and CCDps measures were defined by Rochet N, et al. [26].
Statistical Methods
Data were coded, cleaned, and analyzed using the Statistical Package for Social Sciences version 21.0 for Windows (SPSS Inc., Chicago, IL, USA). Descriptive statistics were used to calculate means and Standard Deviations (SD) on continuous variables, and frequencies and percentages on categorical variables. The dosimetric efficacy of ABC was analyzed by comparing the outcome dosimetric parameters between ABC and FB simulations using paired t-test; results are presented as mean paired difference in the given parameter with the corresponding level of significance. Additionally, the correlation between FB and ABC measurements was analyzed by calculation of Pearson’s coefficient. Linear regression was used to analyze the association of body mass index with the relative change in critical dosimetry parameters including heart mean dose, left lung V20, and both lungs V20. A p-value of <0.05 was considered to reject the null hypothesis.
Results
Participants’ Characteristics
17 Cases were planned. The mean (SD) age of the participants was 45.29 (10.14) years, 6 (35.3%) were overweight and 6 (35.3%) were obese. All patients received hypofractionated RT, and the majority received a total dose of 40 Gy (12/17) in 15 fractions (14/17) (Table 1).
| Parameter | Mean | SD |
|---|---|---|
| Age (years) | 45.29 | 10.14 |
| Weight (Kg) | 71.53 | 20.31 |
| Height (cm) | 146.82 | 38.84 |
| BMI (kg/m2) | 29.10 | 7.55 |
| Cardiac Contact Distance (CCD, cm) | ||
| Axial plane | 4.49 | 1.59 |
| Parasagittal plane | 7.19 | 1.95 |
| Frequency | Percentage | |
| Weight category | ||
| Underweight | 1 | 5.9 |
| Normal | 4 | 23.5 |
| Overweight | 6 | 35.3 |
| Obese | 6 | 35.3 |
| Dose (Gy) | ||
| 40,05 | 12 | 70.6 |
| 42,40 | 1 | 5.9 |
| 45 | 3 | 17.6 |
| 50 | 1 | 5.9 |
| No. of fractions | ||
| 15 | 14 | 82.4 |
| 16 | 1 | 5.9 |
| 25 | 2 | 11.8 |
Dosimetric Efficacy of ABC
Although no significant difference was observed in the heart volume between the two treatment plans (p=0.433), ABC was associated with 1.8 Gy (40.9%) decrease in heart mean dose (p=0.001), 6.1 Gy (14.4%) decrease in heart maximum dose (p=0.015), and 4.2% (relative decrease=68.9%) and 6.5% (relative decrease=46.4%) decrease in Heart V25 (p<0.001) and V5 (p<0.001), respectively. On the other hand, no significant difference between the two techniques was observed in lung parameters including left lung mean (p=0.185) and maximum (p=0484) doses, or Left Lung V20 (p=0.122) or V5 (p=0.797) (Table 2).
| Parameter | Unit | FB | ABC | Mean paired difference | % change | p-value | ||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||||
| Heart volume | cm3 | 522.4 | 107.8 | 508.3 | 77.8 | 14.1 | -2.70% | 0.433 |
| Heart mean dose | Gy | 4.4 | 2.1 | 2.6 | 0.9 | 1.8 | -40.90% | 0.001* |
| Heart maximum dose | Gy | 42.4 | 4.8 | 36.4 | 11.0 | 6.1 | -14.40% | .015* |
| Heart V25 | % | 6.1 | 4.3 | 1.9 | 1.7 | 4.2 | -68.90% | <0.001* |
| Heart V5 | % | 14.0 | 6.5 | 7.5 | 3.9 | 6.5 | -46.40% | <0.001* |
| Left lung volume | cm3 | 935.2 | 253.4 | 1822.1 | 386.1 | -886.9 | 94.80% | <0.001* |
| Left lung mean dose | Gy | 11.4 | 3.7 | 10.5 | 2.4 | 0.8 | -7.00% | 0.185 |
| Left lung maximum dose | Gy | 43.4 | 4.2 | 44.1 | 5.1 | -0.7 | 1.60% | 0.484 |
| Left lung V20 | % | 25.9 | 10.2 | 23.3 | 6.2 | 2.6 | -10.00% | 0.122 |
| Left lung V5 | % | 41.7 | 11.7 | 41.3 | 9.1 | 0.5 | -1.20% | 0.797 |
| Both lungs V20 | % | 11.8 | 4.6 | 11.0 | 3.0 | 0.8 | -6.80% | 0.254 |
| Both lungs V5 | % | 18.9 | 5.5 | 19.3 | 4.3 | -0.4 | 2.10% | 0.603 |
| *: Statistically significant | ||||||||
Apart from Heart V25, all dosimetry parameters were positively intercorrelated between FB and ABC treatment plans, which was more notable in left lung volume (r=0.909) and left lung and both lungs V20 and V5 (r>0.750), in addition to heart volume (r=0.742) (Table 3).
| Parameter | r | p-value |
|---|---|---|
| Heart volume | 0.742 | 0.001* |
| Heart mean dose | 0.535 | 0.027* |
| Heart maximum dose | 0.564 | 0.018* |
| Heart V25 | 0.431 | 0.084 |
| Heart V5 | 0.575 | 0.016* |
| Left lung volume | 0.909 | <0.001* |
| Left lung mean dose | 0.749 | 0.001* |
| Left lung maximum dose | 0.601 | 0.011* |
| Left lung V20 | 0.779 | <0.001* |
| Left lung V5 | 0.767 | <0.001* |
| Both lungs V20 | 0.788 | <0.001* |
| Both lungs V5 | 0.772 | <0.001* |
| r: Pearson’s correlation coefficient, *: Statistically significant | ||
Effect of BMI on Dosimetry Parameters in Either Treatment Plan and the Relative Performance of ABC
Left Lung V20 (R2=0.28, B=0.43, p=0.029) and Both Lung 20 (R2=0.28, B=0.21, p=0.028) were linearly correlated with BMI using ABC but not FB. Otherwise, there was no association of BMI with the absolute or relative changes in heart mean dose, Left Lung V20 or both Lungs V20, between FB and ABC. Likewise, there was no correlation of BMI with heart mean dose using FB (Pearson’s correlation coefficient r=0.18, p=0.488) or ABC (r=0.368, p=0.146) separately (Table 4).
| Dosimetry Parameter | R2 | B | 95%CI | p-value | |
|---|---|---|---|---|---|
| Free-breathing | |||||
| Heart mean dose | 0.03 | 0.05 | -0.10 | 0.20 | 0.488 |
| Left lung V20 | 0.17 | 0.56 | -0.12 | 1.24 | 0.099 |
| Both lungs V20 | 0.16 | 0.25 | -0.06 | 0.56 | 0.107 |
| ABC | |||||
| Heart mean dose | 0.14 | 0.04 | -0.02 | 0.12 | 0.146 |
| Left lung V20 | 0.28 | 0.43 | 0.05 | 0.82 | 0.029* |
| Both lungs V20 | 0.28 | 0.21 | 0.03 | 0.39 | 0.028* |
| Absolute FB-to-ABC change (Gy) § | |||||
| Heart mean dose | 0.00 | -0.01 | -0.14 | 0.12 | 0.924 |
| Left lung V20 | 0.02 | -0.13 | -0.61 | 0.35 | 0.584 |
| Both lungs V20 | 0.01 | -0.04 | -0.25 | 0.17 | 0.701 |
| Percent FB-to-ABC change (%) ‡ | |||||
| Heart mean dose | 0.03 | 0.05 | -0.11 | 0.22 | 0.515 |
| Left lung V20 | 0.05 | -0.06 | -0.19 | 0.08 | 0.397 |
| Both lungs V20 | 0.02 | -0.04 | -0.18 | 0.10 | 0.563 |
| R2: Squared correlation coefficient; B: linear regression coefficient; CI: confidence interval; § Absolute change in the given parameter is calculated as ABC-FB; ‡ Percent change in the given parameter is calculated as 100*(ABC-FB)/FB | |||||
Discussion
Summary of Findings
The increasing prevalence of breast cancer along with the improved awareness, screening, and treatment have resulted in a growing number of cancer survivors with relatively young age, who are exposed to long-term cardiac radiotoxicity. Therefore, radiation oncologists are increasingly required to enhance accuracy in RT, by reducing radiation dose and volume to healthy organs, while delivering effective doses to target volumes. Consensus guidelines recommend that the volume of heart receiving radiation should be minimized as much as possible without compromising target coverage [27].
Considering these issues, this study was carried out to assess the effectiveness of implementing DIBH, using an ABC, in reducing dose and volume radiation received by the myocardium and lung tissues in patients with left-sided breast cancer. In comparison to FB, ABC induced a substantial relative decrease in heart mean (40.9%) and maximum (14.4%) doses as well as in Heart V25 (68.9%) and V5 (46.4%). The FB and ABC measurements were significantly correlated for all parameters. We have noticed that an elevated BMI may be associated with increased lung dose which may reduce the benefit of DIBH but this is to be explored and clinically correlated in future studies.
Dosimetric Efficacy of DIBH in Literature
Findings from the present study add to the growing evidence suggesting that the adoption of breathing maneuvers and RT techniques for left-sided breast cancer patients improve treatment precision, organ sparing, and dosimetric results [28-36]. Two Turkish studies used a comparable design to the present study and showed similar findings regarding the effectiveness of DIBH in reducing cardiac dose and volume. The first one, by Dincoglan, et al., compared DIBH with FB in 27 post-mastectomy patients with locally advanced left-sided breast cancer and showed a mean relative decrease in heart V30 (72.9%), V5 (51.8%), and mean dose (40.9%) [28]. The second study, by Sager, et al., was conducted among 25 patients with early-stage breast cancer after breast-conserving surgery and showed a mean relative decrease in heart V30 (76.3%), V5 (61.0%), and mean dose (51.8%) [29]. However, contrary to our findings, both previous studies showed a significant effect of DIBH in reducing lung volume and dose including ipsilateral lung V20 (16.6% and 27.0%), and mean dose on ipsilateral (19% and 22.9%) and both (21.1% and 24.0%) lungs, respectively. Furthermore, the two studies assessed the relative decrease in mean doses received by other critical organs including the Left Anterior Descending artery (LAD, 69.3% and 53.1%) and the spinal cord (20.3% and 54.0%) [28,29]. Another study from Canada, by Lin, et al., used the same design to measure the relative decrease in heart and LAD dosevolume parameters using both locoregional irradiation for 15 patients with breast-conserving surgery, and whole breast RT for 17 postmastectomy patients. Authors reported a 94% decrease in heart V25, 65% decrease in heart V5, and 44% decrease in mean heart dose, along with a 65% decrease in LAD mean dose [30]. In Qatar, Al-Hammadi, et al. assessed the dosimetric efficacy of voluntary DIBH among a selection of 54 patients operated for left-sided breast cancer, who showed heart V25 ≥ 5% at FB. The authors reported a significant reduction in mean heart V25 (62.4%), heart V10 (65.3%), and heart mean dose (47.5%); in addition to a significant decrease in mean LAD dose (35.7%). However, similar to our finding, no significant change in left lung V20 and mean dose was observed [35].
Clinical Benefits of DIBH
It is worth noting that the clinical benefits of DIBH on cardiac morbidity and mortality have not been evidenced to date, given the prolonged latency of cardiac radiotoxicity. Hence, the only evidence comprises surrogate outcomes including the previously exposed dosimetric parameters or derived predictive models of cardiac morbidity and mortality. Simonetto, et al. modeled the expected Years of Life Lost (YLL) associated with the estimated risk of radiation-induced Ischemic Heart Disease (IHD) under DIBH versus FB. The model showed a 0.04 reduction in mean YLL under DIBH, and this was more remarkable in patients with high baseline risk, low tumor grade, or high mean heart dose under FB [22]. Chatterjee, et al. estimated the DIBH-associated reduction in YLL and the related resource utilization, after estimating the risk reduction of radiation-induced IHD and the associated mortality, by reference to YLL due to IHD in the reference population. The model predicted a mean 0.95 reduction of YLL for every 100 patients treated with DIBH, which represents approximately 13 hours of life saved per 1 hour of work required to implement DIBH [23]. The two previous models provide mathematical estimates of the survival and cost-effectiveness benefits of DIBH by reference to FB. However, further prospective cohorts are warranted to confirm such benefits and balance the indication of DIBH with regards to the patient-specific factors that may impact this benefit. Regarding morbidity, some authors probed into the effect of DIBH in reducing radiation-induced myocardial perfusion defects, which would constitute a more tangible indicator for cardiac radiotoxicity. Unfortunately, a randomized controlled trial by Zellars, et al. failed to demonstrate any difference in the incidence of myocardial perfusion defects between the two treatment plans [37].
Patient Selection for ABC-DIBH and Effect of BMI
Findings from the present study showed that left and both lung V20 increased proportionally with BMI in ABC-DIBH but not in FB, which suggests that the implementation of an ABC may increase lung radiotoxicity in obese patients. In literature, several patient-specific factors have been explored to predict the benefit of DIBH, but to our knowledge no mention of the effect of BMI. Among these factors is the maximum heart distance, which was demonstrated to be positively correlated with the mean heart dose [33]. Other authors found that both axial and parasagittal CCDs were strongly correlated with the heart dose, with greater distances associated with higher doses [38-40]. In the present study, the FB axial, but not the parasagittal, CCD was positively correlated with the mean heart dose in ABC (R2=0.322, B=0.26, p=0.018); however, considering our limited resources, it may not be useful as a screening method to select which patient should be for ABC. Other anatomical factors that may impact the heart doses are the pendulous breast and posterior tumour location; it may be of interest to assess the correlation of either factor with the effectiveness of DIBH in reducing heart doses [33]. Interestingly, Lin, et al. demonstrated that patients who had mastectomy exhibited more benefit from DIBH in terms of heart volume and dose reduction [30].
Other patient-specific factors that may hypothetically limit the indication or cost-effectiveness of DIBH include claustrophobia and reduced lung function. Yet, many research efforts are needed to determine the relevant patientspecific factors that would enable accurate selection of patients with the best-expected benefit, thus optimizing the effectiveness and cost-effectiveness of using DIBH. These criteria are to be considered in combination with the patient’s compliance and tolerance to the DIBH technique, and further interventions and or innovations may be required to improve the treatment convenience for the target patients or to enhance the effectiveness in those with low efficacy profiles. Other factors that need to be considered are inherent to the limitations of the technique itself, including increased CT simulation time (estimated 45-55 minutes), and a 25-minute increase in daily treatment time per patient, on average, which may increase the clinical workload. Besides, the ABC device is onerous, and its implementation requires specialized training for physicians and radiation therapists to optimize the use of the DIBH in routine clinical practice.
Limitations
The present cohort is limited by the small sample size and the retrospective nature of the study.
Conclusion
The incorporation of DIBH with the ABC system improved critical organ sparing, notably concerning the heart dose and volume, with subsequent reduction in radiation-induced cardiac morbidity and mortality. The present study failed to demonstrate any significant beneficial effect of ABC-DIBH on lung-sparing, and further findings suggest an increased lung irradiated volume proportional to patient’s BMI, which indicates the necessity to consider BMI in patient selection for DIBH. Further long-term prospective studies are warranted to confirm the clinical benefits of DIBH and to determine the significant predictors for DIBH effectiveness and cost-effectiveness.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Data Availability
Research data are stored in an institutional repository and will be shared upon request to the corresponding author.
Acknowledgments
The authors thank Dr Mohamed Amine Haireche (amine.haireche@gmail.com) for his kind help in assisting with the statistical analysis and Lookman Adeleke Abdullah for his help in some dosimetry calculations...
References
- Torre, Lindsey A., et al. "Global cancer in women: Burden and trends." Cancer Epidemiology and Prevention Biomarkers, Vol. 26, No. 4, 2017, pp. 444-57.
- Ahmed, Anwar E., et al. "Trends and projections of breast cancer in Saudi Arabia: A national incidence rates by gender, age, nationality, and years (1999-2014)." Arabia, Vol. 12, No. 4, 2019, pp. 9326-31.
- Kingdom of Saudi Arabia, Saudi Health Council, Saudi Cancer Registry. "Cancer Incidence Report Saudi Arabia, 2014." 2017. https://www.nhic.gov.sa/eServices/Documents/2014.pdf
- Early Breast Cancer Trialists' Collaborative Group. "Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials." The Lancet, Vol. 366, No. 9503, 2005, pp. 2087-106.
- Ragaz, Joseph, et al. "Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial." Journal of the National Cancer Institute, Vol. 97, No. 2, 2005, pp. 116-26.
- Piroth, Marc D., et al. "Heart toxicity from breast cancer radiotherapy." Radiation Therapy and Oncology, Vol. 195, No. 1, 2019, pp. 1-12.
- Yeboa, Debra Nana, and Suzanne Buckley Evans. "Contemporary breast radiotherapy and cardiac toxicity." Seminars in Radiation Oncology, Vol. 26, No. 1, 2016, pp. 71-78.
- Schmitz, Kathryn H., et al. "Prospective surveillance and management of cardiac toxicity and health in breast cancer survivors." Cancer, Vol. 118, No. S8, 2012, pp. 2270-76.
- Agrawal, Sushma. "Late effects of cancer treatment in breast cancer survivors." South Asian Journal of Cancer, Vol. 3, No. 02, 2014, pp. 112-15.
- Hatamie, Shadie, et al. "Curcumin-reduced graphene oxide sheets and their effects on human breast cancer cells." Materials Science and Engineering: C, Vol. 55, 2015, pp. 482-89.
- Assali, Akram, et al. "Multifunctional core-shell nanoplatforms (gold@ graphene oxide) with mediated NIR thermal therapy to promote miRNA delivery." Nanomedicine: Nanotechnology, Biology and Medicine, Vol. 14, No. 6, 2018, pp. 1891-903.
- Myers, Evan R., et al. "Benefits and harms of breast cancer screening: A systematic review." JAMA, Vol. 314, No. 15, 2015, pp. 1615-34.
- Capocaccia, Riccardo, G. Gatta, and L. Dal Maso. "Life expectancy of colon, breast, and testicular cancer patients: An analysis of US-SEER population-based data." Annals of Oncology, Vol. 26, No. 6, 2015, pp. 1263-68.
- Cao, Bochen, et al. "Benchmarking life expectancy and cancer mortality: Global comparison with cardiovascular disease 1981-2010." BMJ, Vol. 357, 2017.
- Nielsen, Hanne M., et al. "Study of failure pattern among high-risk breast cancer patients with or without postmastectomy radiotherapy in addition to adjuvant systemic therapy: Long-term results from the Danish Breast Cancer Cooperative Group DBCG 82 b and c randomized studies." Journal of Clinical Oncology, Vol. 24, No. 15, 2006, pp. 2268-75.
- Darby, Sarah C., et al. "Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: Prospective cohort study of about 300 000 women in US SEER cancer registries." The Lancet Oncology, Vol. 6, No. 8, 2005, pp. 557-65.
- Nilsson, Greger, et al. "Distribution of coronary artery stenosis after radiation for breast cancer." Journal of Clinical Oncology, Vol. 30, No. 4, 2012, pp. 380-86.
- Darby, Sarah C., et al. "Risk of ischemic heart disease in women after radiotherapy for breast cancer." New England Journal of Medicine, Vol. 368, No. 11, 2013, pp. 987-98.
- Sixel, Katharina E., Marianne C. Aznar, and Yee C. Ung. "Deep inspiration breath hold to reduce irradiated heart volume in breast cancer patients." International Journal of Radiation Oncology* Biology* Physics, Vol. 49, No. 1, 2001, pp. 199-204.
- Krauss, Daniel J., et al. "MRI-based volumetric assessment of cardiac anatomy and dose reduction via active breathing control during irradiation for left-sided breast cancer." International Journal of Radiation Oncology* Biology* Physics, Vol. 61, No. 4, 2005, pp. 1243-50.
- Remouchamps, Vincent M., et al. "Initial clinical experience with moderate deep-inspiration breath hold using an active breathing control device in the treatment of patients with left-sided breast cancer using external beam radiation therapy." International Journal of Radiation Oncology* Biology* Physics, Vol. 56, No. 3, 2003, pp. 704-15.
- Simonetto, Cristoforo, et al. "Does deep inspiration breath-hold prolong life? Individual risk estimates of ischaemic heart disease after breast cancer radiotherapy." Radiotherapy and Oncology, Vol. 131, 2019, pp. 202-07.
- Chatterjee, Sanjoy, et al. "Resource requirements and reduction in cardiac mortality from Deep Inspiration Breath Hold (DIBH) radiation therapy for left sided breast cancer patients: A prospective service development analysis." Practical Radiation Oncology, Vol. 8, No. 6, 2018, pp. 382-87.
- Ujaimi, Reem K. "Patterns of breast cancer radiotherapy practices among Saudi radiation oncologists." Saudi Medical Journal, Vol. 42, No. 5, 2021, pp. 562-70.
- Small Jr, William, et al. "NRG oncology/RTOG consensus guidelines for delineation of clinical target volume for intensity modulated pelvic radiation therapy in postoperative treatment of endometrial and cervical cancer: An update." International Journal of Radiation Oncology* Biology* Physics, Vol. 109, No. 2, 2021, pp. 413-24.
- Rochet, Nathalie, et al. "Deep inspiration breath-hold technique in left-sided breast cancer radiation therapy: Evaluating cardiac contact distance as a predictor of cardiac exposure for patient selection." Practical Radiation Oncology, Vol. 5, No. 3, 2015, pp. e127-34.
- Gagliardi, Giovanna, et al. "Radiation dose-volume effects in the heart." International Journal of Radiation Oncology* Biology* Physics, Vol. 76, No. 3, 2010, pp. S77-85.
- Dincoglan, Ferrat, et al. "Dosimetric evaluation of critical organs at risk in mastectomized left-sided breast cancer radiotherapy using breath-hold technique." Tumori Journal, Vol. 99, No. 1, 2013, pp. 76-82.
- Sager, Omer, et al. "The role of Active Breathing Control-moderate Deep Inspiration Breath-Hold (ABC-mDIBH) usage in non-mastectomized left-sided breast cancer radiotherapy: A dosimetric evaluation." International Journal of Hematology and Oncology, Vol. 30, No. 4, 2012, pp. 147-55.
- Lin, Angela, et al. "The benefit of deep inspiration breath hold: evaluating cardiac radiation exposure in patients after mastectomy and after breast-conserving surgery." Breast Cancer, Vol. 24, No. 1, 2017, pp. 86-91.
- Nissen, Henrik D., and Ane L. Appelt. "Improved heart, lung and target dose with deep inspiration breath hold in a large clinical series of breast cancer patients." Radiotherapy and Oncology, Vol. 106, No. 1, 2013, pp. 28-32.
- Smyth, Lloyd M., et al. "The cardiac dose‐sparing benefits of deep inspiration breath‐hold in left breast irradiation: A systematic review." Journal of Medical Radiation Sciences, Vol. 62, No. 1, 2015, pp. 66-73.
- Bergom, Carmen, et al. "Deep inspiration breath hold: Techniques and advantages for cardiac sparing during breast cancer irradiation." Frontiers in Oncology, Vol. 8, 2018, p. 87.
- Hayden, Amy J., Melissa Rains, and Kenneth Tiver. "Deep inspiration breath hold technique reduces heart dose from radiotherapy for left‐sided breast cancer." Journal of Medical Imaging and Radiation Oncology, Vol. 56, No. 4, 2012, pp. 464-72.
- Al-Hammadi, Noora, et al. "Voluntary deep inspiration breath-hold reduces the heart dose without compromising the target volume coverage during radiotherapy for left-sided breast cancer." Radiology and Oncology, Vol. 52, No. 1, 2018, p. 112.
- Kim, HaYeon, et al. "Assessment of deep inspiration breath hold technique setup reproducibility using mega voltage imaging for left breast cancer radiation therapy-integrated network study." Medical Dosimetry, Vol. 45, No. 1, 2020, pp. 28-33.
- Zellars, Richard, et al. "SPECT analysis of cardiac perfusion changes after whole-breast/chest wall radiation therapy with or without active breathing coordinator: Results of a randomized phase 3 trial." International Journal of Radiation Oncology* Biology* Physics, Vol. 88, No. 4, 2014, pp. 778-85.
- Lee, Grace, et al. "Anatomic features of interest in women at risk of cardiac exposure from whole breast radiotherapy." Radiotherapy and Oncology, Vol. 115, No. 3, 2015, pp. 355-60.
- Rochet, Nathalie, et al. "Deep inspiration breath-hold technique in left-sided breast cancer radiation therapy: Evaluating cardiac contact distance as a predictor of cardiac exposure for patient selection." Practical Radiation Oncology, Vol. 5, No. 3, 2015, pp. e127-34.
- Ferdinand, Soujanya, et al. "Dosimetric analysis of Deep Inspiratory Breath-hold technique (DIBH) in left-sided breast cancer radiotherapy and evaluation of pre-treatment predictors of cardiac doses for guiding patient selection for DIBH." Technical Innovations & Patient Support in Radiation Oncology, Vol. 17, 2021, pp. 25-31.