Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 7
Complications of Circumcision in Three Hospitals in Douala: Epidemiological, Clinical and Therapeutic Profile
Nwaha Makon Axel Stephane*, Epoupa Ngalle Guy Frantz, Moby Mpah Edouard Herve, Nwatchap Jean Jacques, Tazemda Kuitsouc Gildas Boris and Mouafo Tambo Faustin2Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Cameroon
3Higher Institute of Health Sciences. Université des Montagnes (UdM), Bangangté, Cameroon
Nwaha Makon Axel Stephane, Faculty of Medicine and Biomedical Sciences of the University of Yaounde I, Cameroon, Email: nwahamakon@gmail.com
Received: 26-Jun-2022, Manuscript No. ijmrhs-22-67744; Editor assigned: 29-Jun-2022, Pre QC No. ijmrhs-22-67744(PQ); Reviewed: 30-Jun-2022, QC No. ijmrhs-22-67744(Q); Revised: 15-Jul-2022, Manuscript No. ijmrhs-22-67744(R); Published: 25-Jul-2022
Abstract
Background: Description of the epidemiological, clinical, and therapeutic aspects of the complications of circumcision in three hospitals in the city of Douala. Methods: The work talks about the descriptive cross-sectional study for 4 months (from January to April 2021) with retrospective recruitment over 10 years (January 1st, 2011 to December 31st, 2020) in the surgery Departments of the Douala General Hospital, Douala Catholic Hospital Notre Dame de l’Amour and the Urology Department of Laquintinie Hospital of Douala. During this study period, all records of complications of circumcision that met the inclusion criteria have been included in this study. A pre-designed questionnaire has been used for data collection too. Confirmation of each case of complication was made by at least two urological surgeons. Results: A total of 131 patients have been admitted for complications of circumcision. Out of the 131 patients, the annual frequency of Circumcision complications has reached the level of 13.1 cases/year. Moreover, 29 patients were secondarily excluded from statistics analyzes because of incomplete files. Among the remaining 102 patients, 6 have had more than one complication. The average age has been 6.51 ± 5.74 years with extremes ranging from 1 month to 29 years. The most represented age group has been that of 0 to 5 years. The time elapsed before the consultation has been 1.86 years with extremes from 30 minutes to 16 years. The main reason for the consultation has been urine leakage through the urethral fistula (26.47%) followed by dysuria (24.51%). We found that 23.5% of patients have been circumcised outside the hospital. Paramedics have been responsible for the main complications (66.7%). The most common complication has been urethral fistula 27.5% followed by stenosis of the urethral meatus 24.5%. The study showed that 16.66% of patients required emergency treatment, among which compression bandages for 58.80%, hemostatic suture for 29.40%, antibiotics therapy for 17.60%, and blood transfusion for 5.90%, and urinary catheter for other 5.9%. A total of 95 patients received surgical repair. The clinical course has been satisfactory in 96.10% of cases and 3.90% had a reserved opinion. Conclusions: Circumcision which is known as the most practised surgical act almost all over the world must be performed by competent and trained staff to avoid the occurrence of complications.
Keywords
Circumcision, Complication, Epidemiology, Clinic, Therapy, Douala
INTRODUCTION
Circumcision is the removal of part or the entire foreskin. It is a ritual practised on males’ sexual organs for thousands of years because of cultural and/or religious reasons. Practised since antiquity, it is widely spread throughout the world regardless of ethnicity. The said practice is mainly of public health interest. The estimated percentage of circumcised males in each country and territory varies considerably. The global prevalence of males is around 38.7%. Circumcision presents several advantages. Evidence shows that circumcision drastically reduces the risk of catching HIV infection during sexual intercourse and also the risk of penile cancer. Otherwise, thickening of the skin covering the glans as a result of circumcision would reduce problems of premature ejaculation [1,2]. The trivialization of circumcision and its practice by non-experienced personnel, without any notion of anatomy and complete training, explain the multiple complications observed. Circumcision complication rates vary from one country to another depending on one’s level of development. This rate varies from 2% to 5% in industrialized countries and can reach 85% in developing countries [3]. Complications of circumcision can be low or high sometimes depending on the level of urinary and sexual prognosis. These complications are grouped into early complications (bleeding, amputation of the glans, complete denudation of the penis, infection, necrosis, late slippage or early circumcision devices, and very rarely death) and late complications (sensitivity disorder of the glans, inadequate removal of the skin, inclusion cysts, adhesions, urethrocutaneous fistulas, meatal stenosis, buried penis and phimosis secondarily, skin bridges) [3]. When qualified personnel are available, the management should be multidisciplinary. This work aims to list the cases of circumcision complications carried out in three hospitals in the city of Douala and highlight their epidemiological, clinical and therapeutic profile.
Methods
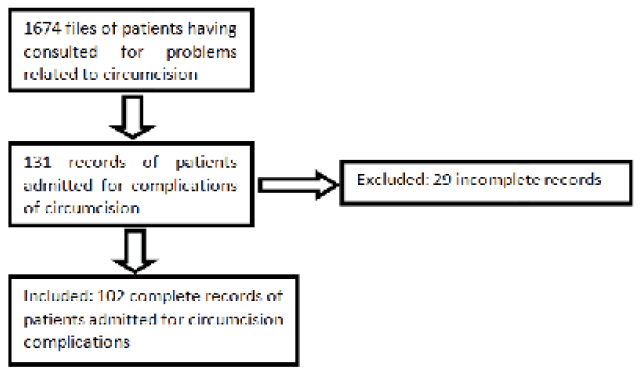
This was a retrospective descriptive cross-sectional study over a study period of 10 years, from 1st January 2011 to 31st, December 2020 in the urology Departments of the hospital Laquintinie, the Douala General Hospital, and the Douala Catholic Hospital Notre Dame de l’Amour. Our study population consisted of all patients seen in medicosurgical emergencies and urological consultations in these health facilities during the study period. The patients were treated in our recruiting hospitals but came all from outside. Any patient records whose diagnosis of circumcision complications had been confirmed by clinical examination and treated in our recruiting hospitals were included in our study. Confirmation of each case of complication of circumcision was made by at least two urological surgeons. We excluded from our study all incomplete files due to missing essential information. Our sampling method was consecutive and exhaustive, including all complete files of patients meeting our inclusion criteria during the period of study Figure 1.
Results
A total of 131 patients were admitted for complications of circumcision. Thus, the annual frequency of Circumcision complications was 13.1 cases/year. 29 patients were secondarily excluded from statistical analyses because of incomplete files. Among the remaining 102 patients, 6 had more than one complication. The average age at the time of consultation for complications of circumcision varied from 0 years to 30 years with an average of 6.51 ± 5.74 years with extremes ranging from 1 month to 29 years. The consultation times were of 16341.19 ± 240.3 hours or 1.86 ± 0.78 years with extremes ranging from 30 minutes to 16 years old. They are predominant in children from 0 years to 5 years old. The reasons for consultation are reported in Table 1.
| Reason for consultation | n | % |
|---|---|---|
| Leakage of urine through the fistula | 27 | 26%, 47% |
| Dysuria | 25 | 24%, 51% |
| Unsightly appearance of the penis | 23 | 22%, 55% |
| Bleeding from the wound | 21 | 20%, 59% |
| Painful penis | 4 | 3%, 92% |
| Swelling of the penis | 1 | 0, 98% |
| Hypogastric pain | 1 | 0, 98% |
| Total | 102 | 100% |
According to table 1, leakage of urine through the fistula was the most frequent reason for consultation (26.47%) followed by dysuria (24.51%), the unsightly appearance of the penis (22.55%), and bleeding from a wound (20.59%). The distribution of complications according to the qualification of the circumciser is reported in table 2.
| Qualification of the circumciser | n | % |
|---|---|---|
| Paramedics | 68 | 66%, 7% |
| Traditional Practitioner | 24 | 23%, 5% |
| General Practitioner | 9 | 8%, 8% |
| Surgeon | 1 | 1% |
| Total | 102 | 100% |
Table 2 reveals that 66.7% were personal paramedics, 23.5% of traditional practitioners, 8.8% of doctors, and 1% of surgeons. The types of complications according to the qualification of the circumciser are detailed in table 3.
| Complications | Surgeon n(%) | General practitioner n(%) | Paramedics n(%) | Traditional Practitioner n(%) | Total |
|---|---|---|---|---|---|
| Post circumcision haemorrhage | 0(0) | 0(8.3%) | 4(33.3%) | 7(58.3%) | 11(11.8%) |
| Infection of the penis | 0(0) | 0(0) | 2(100%) | 0(0) | 2(2%) |
| Glans amputation | 0(0) | 0(0) | 1(25%) | 3(75%) | 4(3.9%) |
| Urethral fistula | 1(3.6%) | 1(3.6%) | 21(75%) | 5(17.9%) | 28(27.5%) |
| Denudation of the penis | 0(0) | 2(22.2%) | 1(11.1%) | 6(66.7%) | 9(8.8%) |
| Urethral meatal stenosis | 0(0) | 3(12%) | 19(76%) | 3(12%) | 25(24.5%) |
| Incomplete circumcision | 0(0) | 0(0) | 9(100%) | 0(0) | 9(8.8%) |
| Skin adhesion | 0(0) | 2(28.6%) | 4(57.1%) | 1(14.3%) | 7(6.9%) |
| Inclusion cyst | 0(0) | 0(0) | 3(100%) | 0(0) | 3(2.9%) |
| Penile granuloma | 0(0) | 0(0) | 3(75%) | 1(25%) | 4(3.9%) |
| Cicatricial phimosis | 0(0) | 0(0) | 4(80%) | 1(20%) | 5(4.9%) |
| Total | 1(0.98%) | 8(7.84%) | 71(69.60%) | 27(26.47%) | 107(100%) |
Table 3 reveals that the most common complications were urethrocutaneous fistula 22.7% then stenosis of the urethral meatus 24.5%, post circumcision haemorrhage 11.8%, penile denudation and incomplete circumcision 8.8%, skin adhesion 6.9%, phimosis scarring 4.9%; penile granuloma and amputation of the glans 3.9%, inclusion cyst 2.9%, penile infection 2% (Table 3). The distribution according to the emergency management figure 1.
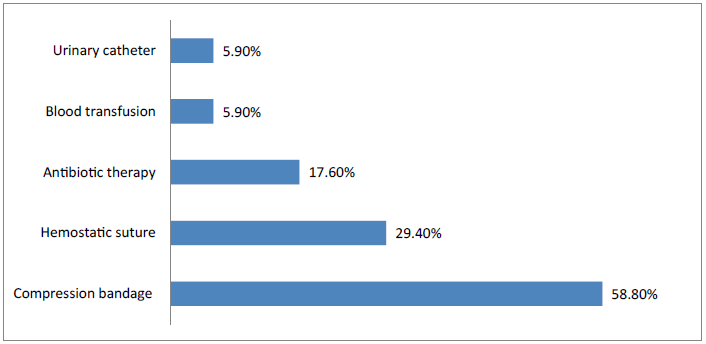
A total of 17 patients (16.66%) required emergency treatment among which compression bandage for 58.80%, hemostatic suture for 29.40%, antibiotics therapy for 17.60%, blood transfusion for 5.90%, and urinary catheter for other 5.9% (Figure 2). The repairment procedure is detailed in table 4.
| Reason for consultation | n | % |
|---|---|---|
| No surgical treatment | 7 | 6.86% |
| Surgical repairment | 95 | 93.14% |
| Adhesiolysis | 12 | 12.6% |
| Cure of urethrocutaneous fistula | 28 | 29.5% |
| Granuloma excision | 3 | 3.2% |
| Excision of penile cyst | 3 | 3.2% |
| Skin graft on penis | 6 | 6.3% |
| Meatomy | 17 | 16.6% |
| Meatoplasty | 7 | 6.86% |
| Prosthectomy | 9 | 9.5% |
| Reimplantation of the penis | 4 | 4.2% |
| Hemostasis suture | 3 | 3.2% |
| Hemostasis suture+penile skin graft | 3 | 3.2% |
| Total | 102 | 100% |
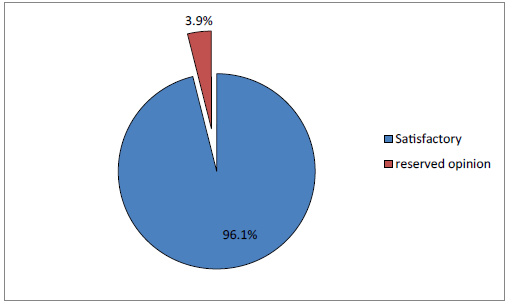
According to table 4, the majority of patients (93.14%) required surgical repair. The repair surgical procedures most used were: the cure of urethrocutaneous fistula (29.5%) followed by meaty (16.6%), Adhesiolysis (12.6%), Meatoplasty (6.86%), Skin graft on the penis (6.3%), etc. The clinical course is reported in figure 2.
The clinical course was satisfactory in 96.1% of cases and 3.9% had a reserved opinion (Figure 3).
Discussion
The consultation time varies greatly depending on the type of complication and the mentality of the people. This is how patients with hemorrhagic complications or amputation of the glans will consult earlier than those presenting a urethral fistula. This periodicity consult could be explained by the spectacular aspect of the lesions thus pushing parents to wonder about the later virility of their children. The average consultation time in our study was 1.86 ± 2.7 years with extremes of 30 minutes to 16 years. Some authors have found longer periods; in particular, Sine, et al. in 2018 in Senegal found an average consultation delay of 5.1 ± 6.9 years [4]. In the same country, Sylla, et al. found an average delay of 4.6 years [5,6]. Rimtebaye, et al. in Chad found a delay of 2 years and 164 days [5]. Mouaffo and al in 2015 in Cameroon found more shortened of 10 months [6]. The delay in consultation in these countries could be explained by the lack of information of the populations who are unaware of the seriousness of the complications and bring their child to consult only when urinary sequelae appear.
Early complications of circumcision
Post circumcision haemorrhage accounted for 11.8% of our complications, amputation of the glans 3.9%, infection of the penis 2%, and denudation of the penis 8.8%. Dieth, et al. in Cote d’Ivoire reported a frequency of 14% post circumcision haemorrhage, 6% infection of the post circumcision penis, and 11% of cases of glans amputation. There were no cases of denudation of the penis and compared to our study this can be explained by their place of study which included only one health facility that could also explain their reduced number of patients (35 cases) compared to ours which is 102 cases and including 3 health facilities in the city of Douala. Diallo, et al. in Guinea Conakry had over 8.5 years of 44 cases including 22.7% post circumcision haemorrhage, 4.5% amputation of the glans, and 2.5% amputation of the urethral floor [4-12]. There were also no cases of denudation of the penis but also infection of the penis could be explained by their place of study which has not included only one health facility and the duration of their smaller study as well as the number of cases found compared to ours which was 10 years old with several 102 cases and including 3 health facilities in the city of Douala.
Mahamat, et al. over 3 years had 31 cases including 16% post haemorrhage circumcision, 10% glans amputation post circumcision, and 16% glans infection. In their series, they did not also have cases of denudation of the penis. This is also explained by their shorter period of study, their place of study also including a single health facility, and their reduced number of cases, unlike our series [13]. Sylla, et al. in Senegal had 63 cases of complications, 14.2% amputation of the glans, 1.5% denudation of the penis, 9.5% haemorrhage, and 1.5% sepsis following a penis infection. This number of cases was low as compared to ours and could also be explained by the place of study which concerned only one health facility. The proportions found in these different comparative studies above are variable depending on the practitioner who performed the circumcision [14,15].
Diallo, et al. in Guinea Conakry had 44 cases over 8.5 years, including 22.7% post-circumcision haemorrhage, 4.5% amputation of the glans, and 2.5% of amputation of the urethral floor. They also did not have cases of denudation of the penis but cases of infection of the penis. This could be explained by their place of study which included only one health facility and the duration of their study as well as the number of cases found compared to ours which was 10 years with several 102 cases. Mahamat, et al. over 3 years had 31 cases including 16% post circumcision haemorrhage, 10% post circumcision glans amputation, and 16% glans infection. In their series, they also did not have any cases of denudation of the penis; this is also explained by their shorter study period, their study site also including a single health facility, and their reduced number of cases, unlike our series. Sylla, et al. in Senegal had 63 cases of complication, 14.2% amputation of glans, 1.5% denudation of the penis, 9.5% haemorrhage, and 1.5% sepsis following a penile infection, this number of cases was low compared to ours and could also be explained by the place of study which concerned only one health structure. The proportion found in these different comparative studies above is variable depending on the practitioner who performed the circumcision [12,15].
Late complications of circumcision
In our series, the urethral fistula is the most frequently reported complication with a proportion of 27.5%. The reason for consultation was the leakage of urine by the fistula. As late complications, we had urethral stenosis which represented 25%, incomplete circumcision 8.8%, skin adhesion 6.9%, inclusion cyst 2.9%, penile granuloma 3,9%, and cicatricial phimosis 4.9%. Sylla, et al. in Senegal had 63 cases among which the urethral fistula represented 65.07%, the urethral stenosis 12.69%, and pseudo elephantiasis of the penis 3.17% [15]. There were no cases of skin adhesion, incomplete circumcision, penile granuloma, cicatricial phimosis, or an inclusion cyst. This could also be explained by their place of study which concerned only one health facility. Unlike our study, the high proportion of certain late complications such as urethral stricture compared to our series could be explained by the traditional method of circumcision predominant in this study because of poor hemostasis of the frenulum artery or the possible adhesions which can increase the vulnerability of the urethra at the level of the balance-prenuptial furrow where it is more superficial. Diallo, et al. in Guinea Conakry had some 44 cases of the urethro-cutaneous fistula which also represented the most frequent complication (63.6%), the stenosis of the urethral meatus (2.3%), the unsightly aspect of the penis (2.3%) [12]. This could also be explained by the place of study which included only one health facility and their period of short study (8.5 years), unlike our study which included 3 hospitals for study over 10 years. Dieth, et al. in Cote d’Ivoire had 35 cases in their seriesn [1]. This is lower than ours and this over 14 years. The stenosis of the urinary meatus was the main complication (49%). In late complications, we also had urethral fistulas 9%, and incomplete circumcision 9%. In this series, there were no cases of pseudo elephantiasis of the penis, skin adhesion, penile granuloma, cicatricial phimosis, or an inclusion cyst. This could be explained by the place of their study which included only one health facility. In addition, the predominance of stenosis of the urethral meatus here could be explained by the method of circumcision which was performed here in the majority of cases by the traditional practitioner. The common point in all this comparative study is the aetiology of the complications attributed to the practitioner. Circumcision techniques were those using pliers, in particular the Guillotine technique.
Therapeutic aspect
The emergency management of its complications in our series was a compression bandage for a post circumcision haemorrhage (6 cases) or denudation of the penis (2 cases) or the combination of the 2 complications above (2 cases); emergency antibiotic therapy was used for infections (3 cases). Only 1 case of post circumcision haemorrhage has been done under questionable asepsis conditions and by a traditional practitioner. Necessity hemostatic stitches (5 cases) were performed in the emergency room, including 3 cases of post-circumcision haemorrhage and 2 cases of denudation of the penis. One patient had a blood transfusion for a hemorrhagic-type post circumcision complication and one patient had a mentoplasty indicated for stenosis of the urethral meatus complicated by acute retention of urine.
In our series, among 102 patients we had, the management of early complications was reimplantation of the penis in cases of amputation of the glans (4.2%), hemostasis suture in cases of post circumcision haemorrhage (3.2%), hemostasis suture and penile skin graft in cases of post circumcision haemorrhage associated with denudation of the penis (3.2%). Dieth, et al. in Cote d’Ivoire in their study which concerned 35 cases had 14% of post circumcision haemorrhage taken care of by coagulation with the electric bistoury, 6% corresponding to the infections of the rod were taken in charge by local care and antibiotic therapy, patients who had an amputation of the glans lost sight of. Diallo, et al. in Guinea Conakry in their series on 44 cases, had as management of early complications the resumption of hemostasis in the event of haemorrhage in 19.5% of cases, 2.5% corresponding to glans amputations that were treated by penile reimplantation, 2.5% corresponding to partial glans amputations that were treated by mentoplasty [4,12]. Mahamat, et al. in Chad, in their series which involved 31 cases had 6.6% corresponding to post circumcision haemorrhages in haemophiliac patients who were treated by blood transfusion associated with local care, 9.67% of cases of post circumcision haemorrhage were managed by hemostatic suture associated with local care, 16.2% had local care associated with antibiotic therapy.
Late complications were treated by the cure of urethro-cutaneous fistula indicated for urethro-cutaneous fistula (29.5%), excision of granuloma (3.2%), excision of the penile cyst (3.2%), anatomy associated with Mentoplasty (23.46%), Prostatectomy (9.5%), Adhesiolysis (12.6%). Dieth, et al. in Côte d’Ivoire had 9% of cases of fistula repairment, 9% of meatoplasty and 49% of cases [4]. Diall, et al. in Guinea had 63.6% of urethro-cutaneous fistula repairmen and 2.5% cases of penile skin plasty [12].
Conclusion
Circumcision is the most practised surgical act. This surgical procedure must be performed by informed and trained personnel to avoid the occurrence of complications, especially, since the frequency is still high. In this study, paramedical personnel were responsible for the majority of the complications because of their incompetence in the matter and poor control of the technique used. These complications were dominated by an urethrocutaneous fistula and stenosis of the urethral meatus.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author contributions
• Nwaha Makon Axel Stephane: Conception; Design, data collection, data analysis and writing.
• Epoupa Ngalle Guy Frantz: Conception and writing.
• Kengni Sipowo Adam Franck: Analysis and writing.
References
- Dave, Sumit, et al. "CUA guideline on the care of the normal foreskin and neonatal circumcision in Canadian infants (abridged version)." Canadian Urological Association Journal, Vol. 12, No. 2, 2017, pp. 18-28.
Google Scholar - Diallo, Abdoulaye B. "Uretro-Cutaneous fistula after Circumcision: analysis Of 38 Cases at the conakry chu, guin." African Journal of Urology and Andrology, Vol. 1, No. 7, 2017.
Google Scholar - Dieth, A. G., et al. "Accidents de circoncision chez l’enfant à Abidjan, Côte d’Ivoire." Bulletin de la Societe de Pathologie Exotique, Vol. 101, No. 4, 2008 pp. 314-15.
Google Scholar - Rimtebaye, Kimassoum, et al. "Caractéristiques épidémiologiques, anatomocliniques et thérapeutiques des complications de la circoncision." Revue Africaine d'Urologie et d'Andrologie, Vol.1, No. 5, 2016.
Google Scholar - Tambo, Mouafo F, et al. "Aspects anatomocliniques et thérapeutiques des accidents de la circoncision à l’hôpital Gynéco-obstétrique et pédiatrique de Yaoundé (HGopY): à propos de 15 cas." African Journal of Pediatric Surgery, Vol. 8, No. 3, 2014, pp. 15-18.
Google Scholar Crossref - Diabaté, I., et al. "Prise en charge des complications de la circoncision." Sexologies, Vol. 26, No. 3, 2017, pp. 169-75.
Google Scholar Crossref - Kim, Jin K., et al. "Assessment of risk factors for surgical complications in neonatal circumcision clinic." Canadian Urological Association Journal, Vol. 13, No.4, 2019, p. e108.
Google Scholar Crossref - Brisson, Paul A., Haroon I. Patel, and Neil R. Feins. "Revision of circumcision in children: Report of 56 cases." Journal of pediatric surgery, Vol. 37, No. 9, 2002, pp. 1343-46.
Google Scholar Crossref - Tambo, Faustin F. M. "Les accidents de la circoncision à Yaoundé, Cameroun: à propos de cinq observations cliniques." progrès en urologie, Vol. 22, No. 1, 2012, pp. 63-6.
Google Scholar Crossref - Sine, B., et al. "Clinical and therapeutic profile of complications of circumcision over the last decade." African Journal of Surgery and Specialties, Vol. 12, No. 2, 2018, pp. 9-13.
Google Scholar - Diallo, Abdoulaye B., et al. "Circumcision accidents: anatomo-clinical and therapeutic aspects at the University Hospital of Conakry, Guinea. Apropos of 44 cases." Andrology, Vol. 18, No. 1, 2008, pp. 10-16.
Google Scholar - Chaim, Ben, J. et al. "Complications of circumcision in Israel: a one year multicenter survey." Israel Medical Association Journal, Vol. 7, No. 6, 2005, pp. 368-70.
Google Scholar - Yegane, Rooh-Allah, et al. "Late complications of circumcision in Iran." Pediatric surgery international, Vol. 22, No. 5, 2006, pp. 442-45.
Google Scholar Crossref - Sylla, Cheickna, et al. "Complications of circumcision. About 63 cases." Progres en Urologie, Vol. 13, No. 2, 2003, pp. 266-72.
Google Scholar - Mahamat, Mahamat A., et al. "Complications of Circumcision: A Three-Year Experience in N’Djamena Mother and Child Hospital (Chad)." Open Journal of Urology, Vol. 6, No. 4, 2016, pp. 55-62.
Google Scholar Crossref