Research - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 2
Effects on Hemodynamic Parameters in Patients Undergoing Caesarean Section Under Low Dose Spinal Anaesthesia
Swarbhanu Porel1, Keya Chakraborty1* and Uma Mondal22Department of Anaesthesiology, College of Medicine & Jawaharlal Nehru Memorial, Medical College, West Bengal, India
Keya Chakraborty, Department of Anaesthesiology, Ramakrishna Mission Seva Pratishthan, & Vivekananda Institute of Medical Sciences, West Bengal, India, Email: drkeyachakraborty21@gmail.com, drkeyahalder@gmail.com
Received: 27-Jan-2023, Manuscript No. ijmrhs-23-88076; Editor assigned: 01-Feb-2023, Pre QC No. ijmrhs-23-88076(PQ); Reviewed: 04-Feb-2023, QC No. ijmrhs-23-88076(Q); Revised: 18-Feb-2023, Manuscript No. ijmrhs-23-88076(R); Published: 28-Feb-2023
Abstract
Background: The purpose of our study was to compare the level of an adequate block with hemodynamic stability with a low dose of Hyperbaric bupivacaine and a conventional dose of bupivacaine in spinal anesthesia for patients undergoing lower uterine cesarean section in a sitting position. Methods: 60 pregnant patients belonging to ASA I and II undergoing elective cesarean section under spinal anesthesia were studied in this prospective, randomized double-blinded study. First group A (n=30) was given inj. Hyperbaric Bupivacaine 12.5 mg and group B (n=30) were given inj. Hyperbaric Bupivacaine 10 mg. Parameters like time for an adequate level of analgesia, peak sensory, and motor level reached, duration of sensory, motor block, and incidence of complications was noted in both groups. Result: The time of onset of an adequate level of sensory block (T10) and motor block was longer for group B than group A. Duration of sensory block and motor block was slightly more for group A but the duration was sufficient to conclude the surgery. Conclusion: It is concluded that subarachnoid block with inj. Hyperbaric Bupivacaine 10 mg is more hemodynamically stable and a better option for pregnant patients undergoing lower uterine cesarean section under spinal anesthesia
Keywords
Bupivacaine, Spinal anesthesia, Caesarean section
Introduction
Professor August Bier performed the first surgical operation using spinal anesthesia at the Royal Surgical Hospital of the University of Kiel, Germany on August 16, 1898 [1]. Attenuation of Intraoperative anxiety and stress always remains a challenge in the practice of anesthesia and it also has several detrimental effects on different systems of the human body. Neuraxial anesthesia techniques have several advantages, including a decreased risk of failed intubation and aspiration of gastric contents, avoidance of depressant agents, decreased blood loss, and the ability to remain awake and enjoy the birthing experience. Single-shot spinal anesthesia is faster, provides a superior block,and is more cost-effective as compared with epidural anesthesia. The subarachnoid block is easier to perform, has a more rapid predictable onset and may produce a more intense block, and does not have the potential for serious systemic drug toxicity, because of the smaller dose of local anesthetic employed [2-4]. The degree of arterial hypotension correlates with the level of sympathetic block which is 2-4 segments higher than the level of anesthesia [5]. Again spread of LA in the Subarachnoid space depends on the dose, volume, position of the patient, site of injection, speed of injection, baricity of the drug, direction of the needle, and barbotage. Pregnancy is known to cause a higher cephalad spread of analgesia. Levels of anesthesia and hemodynamic instability are more in LUCS due to more sensitivity of nerve fiber to local anesthetic for the hormonal influence of pregnancy [6]. There is also an increased risk due to compression of the aorta and inferior vena cava by the gravid uterus often leads to decreased cardiac output, which may precipitate hypotension. Surgical anesthesia up to T4 is sufficient for the lower uterine caesarian section [7]. Surgical anesthesia to T4-T6 was obtained within 5 minutes-15 minutes with hyperbaric bupivacaine 15 mg-20 mg in the nonpregnant patient [8]. In LUCS required dose was reduced to 30% of a normal patient. 9 mg-12 mg of Hyperbaric bupivacaine is the required dose. Hyperbaric bupivacaine is recommended because of its reliability of spread to the mid-thoracic level and appropriate duration of action. Hyperbaric L. A descend downward when sitting and toward T4 when supine.
The purpose of our study was to compare the level of the adequate block with hemodynamic stability with a low dose of Hyperbaric bupivacaine in a lower uterine cesarean section in a sitting position.
Methods
After approval of the institutional ethical committee and informed consent for spinal anesthesia, 60 pregnant patients were randomly divided into 2 equal groups, belonging to ASA I & II, aged 20 to 35 years undergoing elective cesarean section under spinal anesthesia were studied in this prospective, randomized double-blinded trial. Patients with a history of allergy to local anesthetics, any contraindication to subarachnoid block, requiring any intraoperative added general anesthetic aid, deaf, mentally retarded patient/dementia, or with a psychiatric disorder were excluded from the study.
Patients were kept fasted for solid food for at least 8 hours before the operation and clear water till 2 hours before the operation. Intravenous access was obtained in the upper limb with an 18 G cannula and aspiration prophylaxis was given in the form of intravenous Ranitidine 50 mg and Ondansetron 4 mg 30 minutes before the operation. Baseline parameters: Pulse, blood pressure, and SpO2 were recorded. Under all aseptic and antiseptic precautions, lumbar puncture was performed in a sitting position in L3-L4 space by 25 Gauge Quincke point needle. First group A (n=30) was given inj. Hyperbaric Bupivacaine 12.5mg & group B (n=30) was given inj. Hyperbaric Bupivacaine 10 mg and sensory level of T6-T8 was achieved. Patients were given oxygen by nasal cannula at 3 L/minute. Continuous Electrocardiography in lead II, Systolic blood pressure, Diastolic blood pressure, Mean Arterial Pressure, Heart rate, Respiratory rate, and SpO2 were recorded 15 minutes before and at the time of spinal anesthesia, then at 1 minute, at 3 minutes, at 5 minutes, thereafter at 5 minutes interval throughout the entire surgical procedure and 15 minutes interval during first 60 minutes of the postoperative period.
Hypotension was defined as SBP of <90 mm of Hg or a decrease of more than 30% from baseline mean arterial pressure which was treated with an incremental IV bolus of Mephentermine 6 mg. Bradycardia (heart rate<60 bpm) was treated with IV atropine. Inj Paracetamol infusion was given intravenously at 15 mg/kg body weight dosage over 15 minutes duration when the patient first complained of pain. Parameters like time for an adequate level of analgesia, peak sensory, and motor level reached a duration of sensory, motor block, the time when first rescue analgesic is given and incidence of complications were noted in both groups The motor block was assessed using a modified Bromage scale
No paresis – full movements of lower limbs
• Partial paresis-flex knees and ankles
• Partial paresis-flex ankles
• Partial paresis-flex toes only
• Full paresis-no movement
Results
All the statistical analysis was carried out using Microsoft Excel, 2013, and STATA 14 software. Student’s t-test was used to test the null hypothesis that the mean of the two groups is the same at a 5% level of significance. The demographic data (age, weight, sex, and American Society of Anaesthesiologists (ASA) grading) were comparable and statistically nonsignificant (Table 1). The average duration of surgery was 90 minutes.
| Parameters | Group A: Normal | Group B: Low |
|---|---|---|
| Age (yrs) | 25.5 ± 2.55 | 46.54 ± 12.26 |
| Height (cms) | 63.02 ± 2.21 | 63.66 ± 2.39 |
| Weight (kgs) | 58.52 ± 4.90 | 62.72 ± 5.84 |
| Duration of Surgery (mins.) | 90 ± 25.71 | 93.6 ± 24.72 |
| Male: Female | 31:19:00 | 28:22:00 |
| ASA PS Grade I:II | 28:22:00 | 25:25:00 |
| Parameters | Group A: Normal | Group B: Low |
| Age (yrs) | 25.5 ± 2.55 | 46.54 ± 12.26 |
| Height (cms) | 63.02 ± 2.21 | 63.66 ± 2.39 |
| Weight (kgs) | 58.52 ± 4.90 | 62.72 ± 5.84 |
| Duration of Surgery (mins.) | 90 ± 25.71 | 93.6 ± 24.72 |
| Male : Female | 31:19:00 | 28:22:00 |
| ASA PS Grade I:II | 28:22:00 | 25:25:00 |
• T1: onset of sensory block: The ‘Low’ dose, Group B has a mean onset time of sensory block of 6.54 minutes whereas the ‘conventional’ dose, Group A has an onset time of 4.33 minutes. The mean difference is of 2.21 minutes which is significant at a 5% level of significance (Table 2).
| Parameters | Group A: Normal | Group B: Low |
|---|---|---|
| Onset of Sensory Block | 4.33 ± 0.43 | 6.54 ± 0.66 |
| Onset of motor block | 8.83 ± 1.08 | 8.68 ± 1.27 |
| Time to reach peak sensory level | 8.06 ± 0.34 | 9.53 ± 0.70 |
| The duration of sensory block | 121.81 ± 8.14 | 96.14 ± 5.20 |
| Duration of motor block | 231.5 ± 8.57 | 195.86 ± 9.10 |
| Duration of spinal anaesthesia | 261.84 ± 10.78 | 225.96 ± 7.19 |
| Time when first rescue analgesia was given | 397.32 ± 21.51 | 311.9 ± 16.06 |
| Values are reported in the form of Mean ± Standard deviation | ||
• T2: Onset of motor block: The ‘Low’ dose, Group B has a mean onset of 8.68 minutes whereas the ‘conventional’ dose, Group A has an onset of 8.83 minutes. The mean difference is of 0.15 minutes which is not significant at a 5% level of significance with a p-value of 0.52. The difference is low concerning the magnitude and statistically insignificant.
• T3: Time to reach peak sensory level: The ‘Low’ dose, Group B has a mean time to reach the peak sensory level of 9.53 minutes whereas the ‘conventional’ dose, Group A has a mean time of 8.06 minutes. The mean difference is of 1.47 minutes which is significant at a 5% level of significance with a p-value of 0.00.
• T4: The duration of sensory block: The ‘Low’ dose, Group B has a mean duration of 96.14 minutes whereas the ‘conventional’ dose, Group A has a duration of 121.81 minutes. The mean difference is of - 25.67 minutes which is significant at a 5% level of significance with a p-value of 0.00. Though, the duration of the sensory block is 96.14 which is lower than the Normal group the duration is sufficient to conclude the surgery. This is because the mean required duration for surgery is 90 minutes.
• T5: Duration of motor block: The ‘Low’ dose, Group B has a mean duration of 195.86 minutes whereas the ‘conventional’ dose, Group A has a duration of 231.5 minutes. The mean difference is of -35.64 minutes which is significant at a 5% level of significance with a p-value of 0.00. Though, the duration of the motor block is 195.86 minutes which is lower than the conventional group the duration is sufficient to conclude the surgery.
• T6: Duration of spinal anesthesia: The ‘Low’ dose, Group B has a mean duration of spinal anesthesia of 225.96 minutes whereas the ‘conventional’ dose, Group A has a duration of 261.84 minutes. The mean difference is of 35.88 minutes which is significant at a 5% level of significance with a p-value of 0.00. Though, the duration of spinal anesthesia is 225.96 minutes which is lower than the conventional group the duration is sufficient to conclude the surgery.
• T7: A time when first rescue analgesia was given: The ‘Low’ dose, Group B has a mean time of 311.90 minutes when the first rescue analgesia was given whereas the ‘conventional’ dose, Group A has a duration of 397.32 minutes. The mean difference is of 85.42 minutes which is significant at a 5% level of significance with a p-value of 0.00. Though, the time when the first rescue analgesia was given is 311.9 minutes which is lower than the Normal group the duration is sufficient to conclude the surgery.
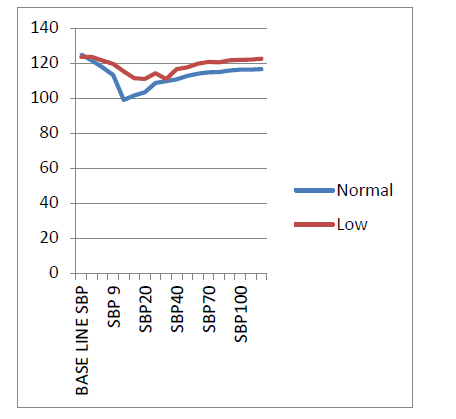
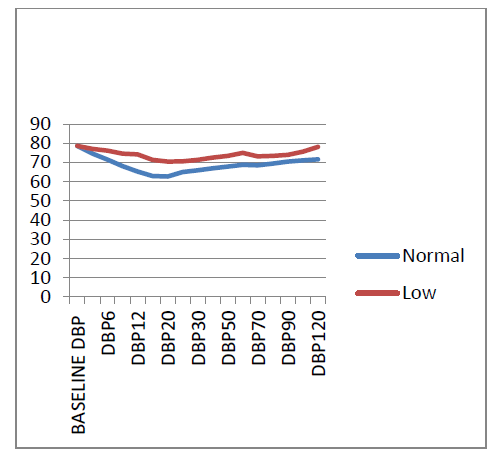
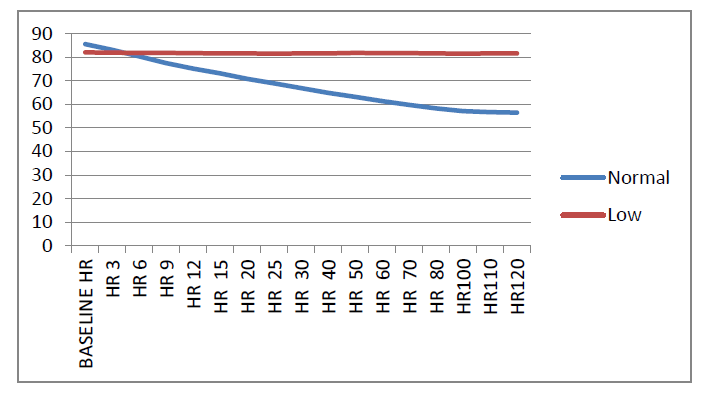
• Incidence of hypotension and bradycardia was more in group A and was found to be statistically significant (Figure 1-3).
None of the patients had nausea, vomiting, respiratory depression, or shivering.
Discussion
Maintenance of body physiology as near normal as possible during anesthesia is one of the primary goals of the anaesthesiologist. Marked hemodynamic derangements are often seen following subarachnoid block, especially in pregnant, trauma, and elderly patients. Hyperbaric bupivacaine is recommended because of its reliability of spread to the mid-thoracic level and appropriate duration of action. Hyperbaric L. A descent downward when sitting and toward T4 when supine.
In our present study, the goal was to compare the level of the adequate block with hemodynamic stability like blood pressure, heart rate changes, and motor and sensory profiles of the block with a low dose of 0.5% Hyperbaric bupivacaine (10 mg) compared to conventional dose (12.5 mg) in lower uterine cesarean section in sitting position. The incidence of hypotension and bradycardia in group A was found to be statistically significant (Figure 1-3).
The ‘Low’ dose, Group B has a mean onset time of sensory block of 6.54 minutes whereas the ‘conventional’ dose, Group A has an onset time of 4.33 minutes. The mean difference is of 2.21 minutes which is significant at a 5% level of significance. The ‘Low’ dose, Group B has a mean duration of 96.14 minutes whereas the ‘Normal’ dose, Group A has a duration of 121.81 minutes. The mean difference is of -25.67 minutes which is significant at a 5% level of significance with a p-value of 0.00. Though, the duration of the sensory block is 96.14 which is lower than the Normal group the duration is sufficient to conclude the surgery. This is because the mean required duration for surgery is 90 minutes (Table 2).
In the study by Russel and Holm Quist injection of Hyperbaric, 0.5% bupivacaine 2.5 ml (12.5 mg) with the patient in the lateral position produced maximum analgesia greater than in the present study. With block rising to the cervical dermatomes in 25% of patients [9].
In the present study, we used 10 mg and 12 mg of hyperbaric bupivacaine. This study differs from that of Russel in dose and volume. The study of MA Karim showed that the dose, volume, and position of the patient when the hyperbaric local anesthetic solution was injected in subarachnoid space for LUCS are significant factors [10].
Robin Russell stated that in LUCS when injected while sitting 10 mg of Hyperbaric bupivacaine produces less satisfactory results than 12.5 mg, while 12 mg in the lateral position is more reliable in achieving bilateral spread than 15 mg in the sitting position [11].
Conclusion
From the current study, it was concluded that the onset of sensory block and the time to reach the peak sensory level is significantly lower for the conventional dose as compared to the ‘Low’ dosage. The duration of sensory and motor block is significantly lower for the ‘Low’ doses than the conventional doses but the duration is sufficient to conclude the surgery. The incidence of hypotension and bradycardia was significantly higher for the conventional dose as compared to the ‘Low’ dosage.
Hence subarachnoid block with 10 mg Hyperbaric bupivacaine 0.5% is a safer and better option, than a conventional dose of 12.5 mg Hyperbaric 0.5% Bupivacaine, both in terms of maintaining hemodynamic stability and lower incidence of complications without compromising the surgical condition for pregnant patients undergoing lower uterine cesarean section under spinal anesthesia. The lower dose can be considered to be a safer alternative for pregnant patients, which can reduce the rate of hypotension, bradycardia, or other complications who may have more hypotension after a conventional dose of bupivacaine.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Van Zundert, Andre, and Michael Goerig. "August Bier 1861-1949." Regional anesthesia and pain medicine, Vol. 25, No. 1, 2000, p. 26.
Google Scholar Crossref - Bacon, D. R. "Regional anesthesia and chronic pain therapy: A history." Regional anesthesia and analgesia. Philadelphia: WB Saunders, 1996, pp. 14-15.
Google Scholar - Rawal, Narinder, et al. "Combined spinal-epidural technique." Regional Anesthesia and Pain Medicine, Vol. 22, No. 5, 1997, pp. 406-23.
Google Scholar Crossref - Islam, Md-Saiful, Shamsun Nahar, and Sk S. Huq. "Efficacy of low dose hyperbaric bupivacaine in spinal anaesthesia for LUCS." Bangladesh Medical Journal Khulna, Vol. 45, No. 1-2, 2012, pp. 15-18.
Google Scholar Crossref - Dyer, R. A., et al. "Prevention and treatment of cardiovascular instability during spinal anaesthesia for caesarean section." South African Medical Journal, Vol. 94, No. 5, 2004, pp. 367-72.
Google Scholar - O'Gorek, Elizabeth K., "Cutting it out: social, medical and professional change and the history of the decline of infant circumcision in Canada, 1945-1996". Library and Archives Canada=Bibliotheque et Archives Canada, Ottawa, 2007.
Google Scholar - Karim, M. A., et al. "effect of site of injection on spread of spinal anaesthesia with Hyperbaric Bupivacaine." Bangladesh Journal of Obstetrics & Gynaecology, Vol. 23, No. 1, 2008, pp. 15-19.
Google Scholar Crossref - Yentis, Steven M., Nicholas Hirsch, and Gary B. Smith. "Anaesthesia AZ: An Encyclopaedia of Principles and Practice." Butterworth-Heinemann, 1993.
Google Scholar - Russell, I. F., and E. L. O. Holmqvist. "Subarachnoid analgesia for caesarean section: a double-blind comparison of plain and hyperbaric 0.5% bupivacaine." British Journal of Anaesthesia, Vol. 59, No. 3, 1987, pp. 347-53.
Google Scholar Crossref - Karim, M. A., et al. "Effect of site of injection on spread of spinal anaesthesia with Hyperbaric Bupivacaine." Bangladesh Journal of Obstetrics & Gynaecology, Vol. 23, No. 1, 2008, pp. 15-19.
Google Scholar Crossref - Bongain, Andre, Veronique Isnard, and Jean-Yves Gillet. "Obesity in obstetrics and gynaecology." European Journal of Obstetrics & Gynecology and Reproductive Biology, Vol. 77, No. 2, 1998, pp. 217-28.
Google Scholar Crossref