Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
Evaluation of Ready-Made Food Sold for Human Consumption at City Local Market
Elgazafey Basheer H Ahmed1, Nazik EM Mustafa2, Mohamed Osman Elamin3* and Hatim A Natto32Department of Public and Environmental Health, University of Khartoum, Sudan
3Department of Public Health & Informatics, Umm Al-Qura University, KSA
Mohamed Osman Elamin, Department of Public Health & Informatics, Umm Al-Qura University, KSA, Email: elamin499@gmail.com
Received: 23-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Background: Food conveys various microorganisms that cause diseases and food poisoning in humans. Low numbers of initial microbial contamination could result in the rapid growth of spoilage or pathogenic organisms. Food-borne diseases are rapidly spreading and transmitting causing outbreaks. The number of food-borne illnesses increases every year. In Sudan, diarrheal disease was the second major disease during the years from 2003 to 2007 as reported in an annual health statistical report of the Federal Ministry of Health, Sudan. The study aims to evaluate the safety of food to the consumer. Methodology: This study was conducted at Khartoum Locality. One hundred forty-five different food samples (milk and milk products, egg, red and white meat, and their products) were collected randomly. Probable number as traditional method and E. coli, Salmonella typhi and Shigella dysentery, the incidence was done to evaluate the safety of the food samples. Results: Total coliform bacteria were detected in 53% of total food samples (30% at the level unsatisfactory and cautionary 23%). The highest presences of coliform were in red and white meat. While the lowest total coliform was encountered in eggs and milk samples. E. coli was found in 9.2% of the samples, while Salmonella typhi was found in 3.9%, and no presence of Shigella dysentery. The personal hygiene procedures, safety management during the food process, Hazard Analysis Critical Control Points (HACCP) system, and Good Manufacturing Practice (GMP) are the main important roles to prevent food contamination.
Keywords
Evaluation, Ready-made food, City market
Introduction
Food supplies the body with nutrients, but at the same time, it conveys a lot of microorganisms that cause diseases and food poisoning. Food is usually contaminated via soil, water, sewage, and air, or contaminated during harvesting of raw materials, storage, transport, handling, and processing [1].
Food-borne illness is a major international public health problem and there are several outbreaks of food-borne diseases that have been documented everywhere. Food-borne diseases seriously affect children, pregnant women, and the elderly besides [2].
FAO and WHO stated that up to be one-third of the population of developed countries may be affected by food-borne diseases each year, and the figures are more than that in developing countries [3]. Many outbreaks of food-borne diseases are due to a poor investigation of early-warning cases [4].
There are several microbiology protocols used in the detection of food-borne pathogens. One of these important groups’ pathogens is Enterobacteriaceae [5].
Objective
To evaluate the safety of food to the consumer through determining the bacterial load, coliform bacteria, and E coli presence comparing with the standard.
Food-borne Diseases as a Public Health Problem
Food-borne diseases can be caused by bacteria, viruses, or parasites. Natural (physical) and manufactured chemicals in food products also can harm people. Some diseases are caused by toxins from the disease-causing organism (germ), others by bodily reactions to the organism itself. Food-borne diseases may have no symptoms or develop symptoms ranging from mild intestinal discomfort to severe dehydration and bloody diarrhea [6-10].
The World Health Organization (WHO) reported that food-borne diseases became a major public health problem and had increased in the last years affecting populations in both developed and developing countries. The intensity of foodborne illnesses increases every year; CDC estimates that 76 million people suffer from food-borne illnesses each14 year in the United States [11].
The major factors that contribute to contamination of food are food handlers, equipment, through contact with raw foods and utensils, air, water, soil, clothes of the workers, packaging materials, distributing and retailing [12].
The useful indicators of unsanitary food and food processing are the presence or contamination with the bacterial family Enterobacteriaceae. Their presence is often considered as an indicator of unhygienic practices in production processes, their presence in high numbers (>104 per gram) in ready-to-eat foods indicates that an unacceptable level of contamination has occurred during food processing [13,14].
Some bacteria that belong to Enterobacteriaceae are called coliforms. They are traditional indicators of food contamination [15]. Regulatory agencies have used Enterobacteriaceae, coliform, or E. coli counts as microbiological criteria to reflect the safety of a particular food product [16].
Codex Alimentarius Commission and FDA stated that the personal hygiene of food handlers would give greater assurance of food safety than clinical examination [17,18]. World Trade Organization (WTO) described the need for regulations governing international trade in foods to be based on science and risk assessment.
According to Bryan survival of bacteria, which contaminate food, can be controlled by heat treatment and acidification [19].
Applicable control measures during production, adequate hygiene standards, and fitting cooking during final preparation should ensure that the end products are being of good quality to the consumers [20]. In addition to that, an International Food Safety Standard (IFSS) has advised farmers to change their production and marketing practices [21].
To prevent foodborne diseases associated with Enterobacteriaceae, WHO reported that Hazard Analysis Critical Control Points System (HACCP) has to be implemented to assess hazards and to establish a control system that focuses on enhancing food safety throughout the food production chain [22].
The safety of food is important for everyone-food manufacturers, catering businesses, organizations for the supply and distribution chain, retailers, and people preparing meals at home, and consumers. Recent legislation now requires a food safety management system, such as Hazard Analysis Critical Control Point (HACCP) intending to reduce the toll of death and ill-health associated with unsafe food [23,24].
WHO established a strategy to reduce the public health hazards of food-borne disease includes developing surveillance systems of food-borne diseases, improvement of risk assessments, developing methods for assessing the safety of the products of new technologies, and strengthening the role of science and public health [25].
FDA stated that only ten cells from E. coli O157:H7 could cause illness. This E. coli O157:H7 became widespread and caused food poisoning in developed countries [26].
In Sudan, E. coli among other species were isolated by Hussein from fresh meat samples; Abd ElRahman isolated E. coli from 17% of minced meat samples; Ahmed investigated E. coli in ready to eat a beef burger in Khartoum State and declared that total coliform bacteria were observed in 48.8% of samples and 9.3% of them were positive for E. coli, Hassan, NA isolated E. coli and other’s bacteria from restaurant’s food, worker’s hands and dishes in Khartoum State [27-29]. Abdalla, et al. surveyed to determine food safety knowledge of street food vendors in Khartoum city [30]. CDC Bulletin reported the incidence of Salmonella in Australia and linked them with a traveler from some countries, including Sudan [31]. Mustafa and Abdallah detected E. coli and Salmonella spp. in 6.6%, and 5%, respectively from Street-Vended Um-Jingir near industrial areas in Khartoum State [32]. Elfaki, et al. detects total coliform bacteria and total bacterial count of (Shawerma) and ice cream in Khartoum State to ensure the safety of two foods [33]. Ali and Abdelgadir estimated the incidence of E. coli, in raw cow’s milk in Khartoum State at 63% of the samples [34].
The diarrheal disease was the second major disease during the years from 2003-2007 in Sudan as reported in an annual health statistical report of the Federal Ministry of Health (FMH) (National Health Information Centre (NHIC) Table 1 [35].
| Diseases | Malaria | Diarrhoea | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | 2003 | 2004 | 2005 | 2006 | 2007 | 2003 | 2004 | 2005 | 2006 | 2007 |
| % of all outpatients | 15.8 | 11.3 | 14.4 | 18.2 | 22 | 10.5 | 8.6 | 10.8 | 4.4 | 4 |
| % of all Inpatients | 21.1 | 18 | 16.3 | 14.8 | 13.6 | 2.8 | 3.5 | 3.5 | 4.5 | 4.4 |
| % Death to the disease of admission | 1.6 | 1.3 | 1.3 | 1.3 | 1 | 3.3 | 2.5 | 2 | 1.8 | 1.4 |
| Prevalence per 1000 population. (Outpatient) | 92 | 60.3 | 71 | 51.6 | 96 | 61 | 46 | 53 | 12.4 | 20 |
| Adapted from NHIC [35] | ||||||||||
Materials and Methods
Study Area
This study was conducted at Khartoum State, Locality of Khartoum in the period from January 2014 to December 2015.
Inspection of Food Samples from the Market
A total of one hundred forty-five different food samples (Table 2) were collected from the Khartoum locality randomly.
| Type of food | Cooked | Uncooked | Total |
|---|---|---|---|
| Vegetable | 0 | 25 | 25 |
| Milk and milk Products | 20 | 10 | 30 |
| Red meat and its products | 25 | 10 | 35 |
| White meat and its products | 25 | 10 | 35 |
| Egg | 15 | 5 | 20 |
| Total | 85 | 60 | 145 |
Food samples were placed in a sterile plastic bag, labeled, and transported to the laboratory in the portable cooler at 4°C. Samples were investigated directly in the laboratory.
Most Probable Number (MPN)
MPN means a statistical estimate of the number of bacteria per unit volume and is determined from the number of positive results in a series of fermentation tubes.
Twenty-five grams of the samples were placed into a stomacher bag with 225 ml of buffer peptone water and blended for 2 min at 230 rpm using a Stomacher (Stomacher 400, Seward, and Norfolk, UK). From the homogenized samples, sufficient diluents were made.A series of nine sets of MacConkey’s broth medium containing Durham’s tubes were divided into three parts and each was inoculated with 10 mL, 1 mL, and 0.1 mL of aliquot sample, then incubated at 37ºC for 48 ± 2 h. Productions of gas and turbidity bubbles were observed after incubation. The number of organisms in the original culture was estimated from an MPN Determination Chart to determine the MPN index per gram [36].
Confirmatory Test
From each positive gassing tube, a loopful of suspension was transferred to a tube of Brilliant Green LB broth, incubated at 35°C for 48 ± 2 h, and examined for gas production. Calculation of the Most Probable Number (MPN) was done [36,37].
Results
Most Probable Number (MPN) of Coliform Bacteria
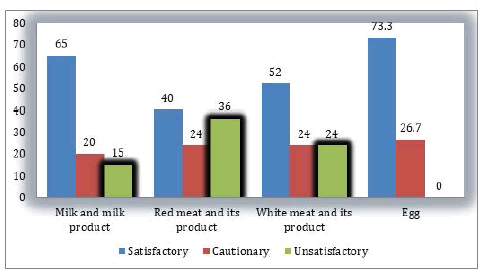
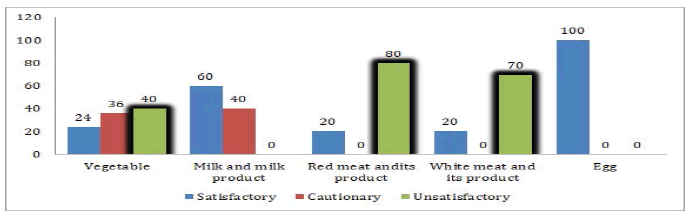
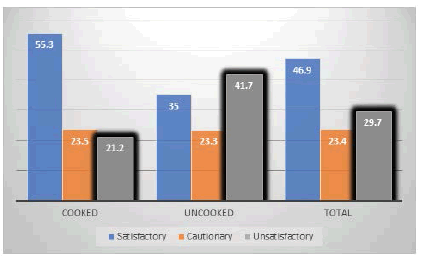
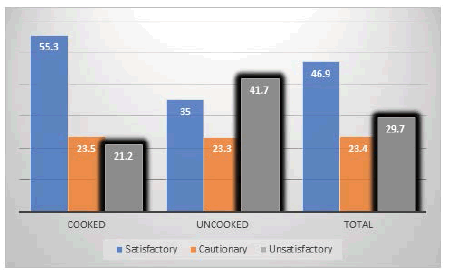
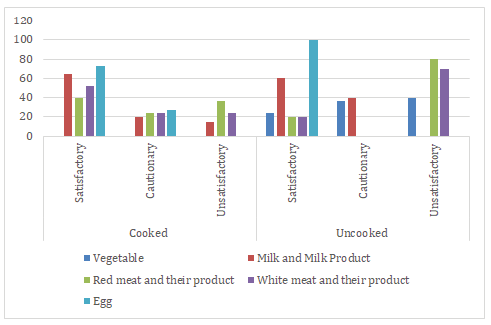
In this study coliform count was detected in different proportions in food samples. The highest unsatisfactory concentration of coliform bacteria was found in red meat and their products followed by white meat and their products, while egg and milk samples were less contaminated than other types of food in both cooked and uncooked food samples (Table 3, Figure 1, Figure 2 and Figure 3).
| Type of food | Cooked | Uncooked | ||||
|---|---|---|---|---|---|---|
| Satisfactory | Cautionary | Unsatisfactory | Satisfactory | Cautionary | Unsatisfactory | |
| Vegetable | 0 | 0 | 0 | 6 | 9 | 10 |
| Milk and milk product | 13 | 4 | 3 | 6 | 4 | 0 |
| Red meat and its product | 10 | 6 | 9 | 2 | 0 | 8 |
| White meat and its product | 13 | 6 | 6 | 2 | 1 | 7 |
| Egg | 11 | 4 | 0 | 5 | 0 | 0 |
| Total | 47 | 20 | 18 | 21 | 14 | 25 |
| Satisfactory <100; Cautionary <1,000; Unsatisfactory ≥ 1,000. (According to British Columbia Centre for Disease Control-BCCDC; and Wong) [38,39] | ||||||
In Figure 4 the safe and hygienic food samples (satisfactory) were approximately only half of the samples (47%).
In the comparison between cooked and uncooked food, Figure 1 and Figure 2 show unsatisfactory coliform levels in uncooked food more than in cooked food, especially in white and red meat and its products (Figure 5). The same MPN result for total samples was shown in Figure 3.
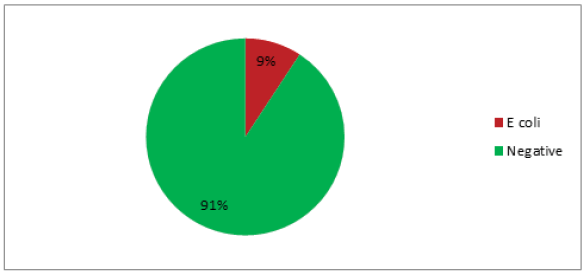
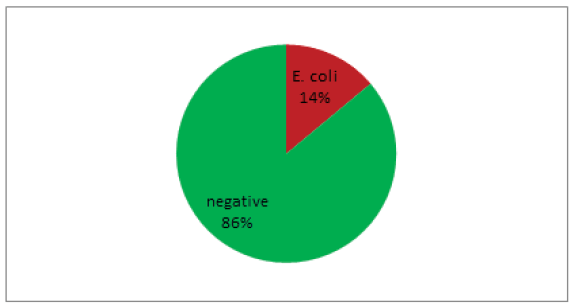
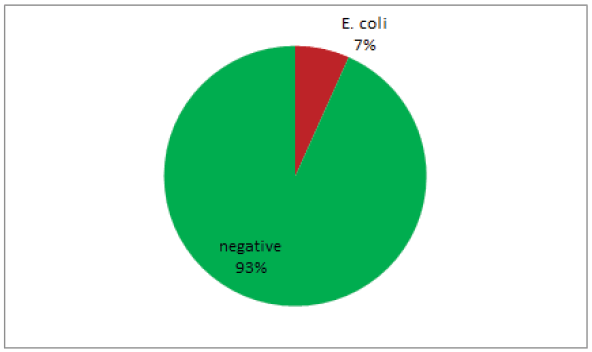
E. coli was found in 9% of the total samples (Figure 6). The incidence of E. coli in cooked food samples was 14% (Figure 7) and in uncooked samples was 7% (Figure 8).
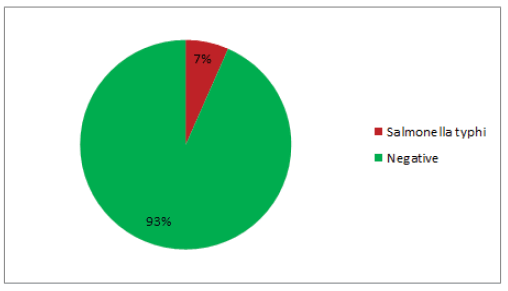
The Salmonella typhi detection result was shown in Figure 9, it was found in 7% of total samples.
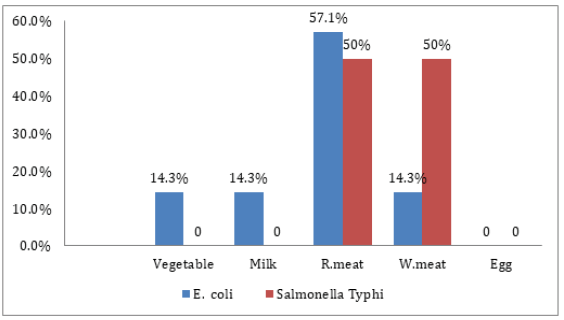
In all food samples analyzed for bacterial contaminants; the (E. coli, Salmonella typhi, and Shigella dysentery) bacterial species were not found in egg samples (Table 4). 57.1% of positive E. coli results were detected in red meat, equal positive Salmonella typhi results were obtained from PCR analysis of white and red meat (50%) Figure 10.
| Type of food | E. coli | Salmonella typhi |
|---|---|---|
| Vegetable | 1 | 0 |
| Milk | 1 | 0 |
| R.meat | 4 | 2 |
| W.meat | 1 | 2 |
| Egg | 0 | 0 |
| Total | 7 | 4 |
Eggs and milk were less contaminated than white and red meat, no presence of Shigella dysentery was detected in these food samples (Figure 10).
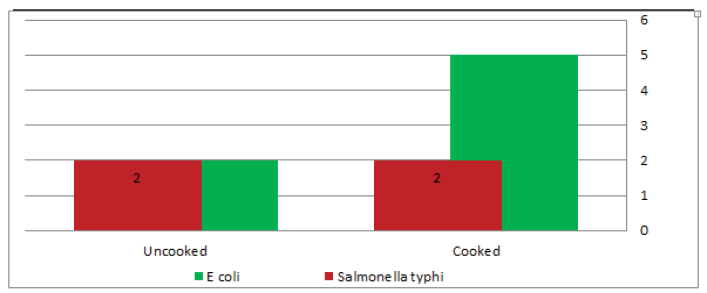
From total Escherichia coli positive samples, 71.4% were identified in cooked food. Salmonella typhi positive results were divided equally among cooked and uncooked samples (Table 5 and Figure 11).
| Bacteria | Total +ve | Cooked food | Uncooked food | ||
|---|---|---|---|---|---|
| +ve | % | +ve | % | ||
| Escherichia coli | 7 | 5 | 71.4 | 2 | 28.6 |
| Salmonella Typhi | 4 | 2 | 50 | 2 | 50 |
| Shigella dysentery | 0 | 0 | 0 | 0 | 0 |
Discussion
Coliform bacteria are used as indicator organisms. In this study coliform bacteria were found at levels that are cautionary and unsatisfactory in 53% of the samples (≥ 1000/g), this was closely identical to a study done by Charles, et al., who found coliform bacteria in 51% of the samples [40]. In the present study, coliform bacteria were encountered in various types of food similar to results obtained by Odu and Akano who analyzed the microbial quality of shawarma purchased in Port Harcourt city, Nigeria, and found the total coliform count ranged from 1.9 × 103 to 9.4 × 105 [41].
In this study, the highest concentrations of coliform were detected in red and white meat. This confirms the high probability of the presence of food-borne bacteria in red or white meat. The contamination may be from personal activities, the meat itself, during the slaughtering process or manufacturing, working tables, or displays for sale.
Eggs samples analyzed showed the lowest total coliform bacteria (there was no unsatisfactory level detected), this may be due to the nature of the egg which has good protection by their intrinsic parameters that minimize the entry of microorganisms. These intrinsic parameters include the outer waxy shell membrane, lysozyme in egg white, avidin which forms a complex with biotin making this vitamin unavailable to microorganisms, conalbumin which forms a complex with iron making it unavailable to microorganisms and a high pH (about 9.3) of egg white [42].
Unlike previous studies carried in Sudan, milk samples showed a low level of total coliform bacteria. This might be because the milk samples contain inhibitory substances such as residues of antibiotics used in animal treatment or for preservation purposes. If so, it has health hazards. The use of antibiotics in food leads to an increase in the number of antibiotic-resistant microorganisms which is not responding to traditional antibiotic treatment. Also cause a mutation and plasmid in microorganism which may harm the human and animal [43-45].
The presence of total coliforms bacteria in the samples is considered a hazardous result not only their amounts in food as mentioned before by the Connecticut Department of Public Health-CDPH [46].
In the present study, coliform was detected in uncooked foods more than cooked foods especially in white and red meat and their product. This is obvious as heat treatment destroys all coliform bacteria. Any coliform bacteria that occur after heat treatment is referred to as cross-contamination.
In this study, the presence of E. coli, Salmonella typhi, and Shigella dysentery by PCR were detected in samples that had coliform more than cautionary. E. coli was found in 6 out of 7 at the level of cautionary and unsatisfactory. All Salmonella typhi were at an unsatisfactory level. It indicates that total coliform is a good indicator for pathogenic bacteria.
Conclusion
This study investigated a total coliform count as the traditional method to evaluate the safety of ready-to-eat food. Coliform is an indicator organism was found at the level cautionary and unsatisfactory in 51% of the samples in the different types of food. Their presence was varying from type to type of food. The highest presences of coliform were in red meat and white meat. While the hygienic food samples were eggs which have the lowest total coliform bacteria, this may be due to the nature of the egg. Milk was also having lower total coliform bacteria and this might be due to the addition of antibiotics during milk production. Coliform was detected in uncooked foods more than cooked foods especially in white and red meat and their product. E. coli was found in 9.2% of the samples, while Salmonella typhi was found in 3.9%, and no presence of Shigella dysentery. E. coli was identified 71.4% in cooked food from total positive samples. Salmonella typhi divided (50%) in cooked and (50%) in uncooked positive samples. Cooked food was more contaminated, especially with E. coli. That means the contamination or cross-contamination was coming to food due to food handlers, utensils, or unsafely ways of food preparations. The presence of E. coli, Salmonella typhi, and Shigella dysentery were detected in samples that had coliform of more than 1110/gram.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Badru, OA. "Isolation of pathogenic bacteria from some foods sold at selected private schools in Akoka area of Yaba Lagos, Nigeria." African Journal of Food Science, Vol. 6, No. 3, 2012, pp. 65-69.
- World Health Organization. "WHO global strategy for food safety: Safer food for better health." WHO, 2010.
- World Health Organization. "Food safety risk analysis: A guide for national food safety authorities." 2006.
- World Health Organization. "Foodborne disease outbreaks: Guidelines for investigation and control." World Health Organization, 2008.
- Foundation, American Nurses Association-American Nurses, et al. "Diagnosis and management of foodborne illnesses: A primer for physicians and other health care professionals." MMWR. Recommendations and reports: Morbidity and Mortality Weekly Report. Recommendations and reports, Vol. 53, No. RR-4, 2004, pp. 1-33.
- National Institute of Allergy and Infectious Disease. "Food-borne Diseases, Overview and papers" U.S Department of Health and Human Services, 2005.
- Su, Chinyu, and Lawrence J. Brandt. "Escherichia coli O157: H7 infection in humans." Annals of Internal Medicine, Vol. 123, No. 9, 1995, pp. 698-707.
- Lynch, Michael, et al. "Surveillance for foodborne-disease outbreaks: United States, 1998-2002." 2006.
- Van, Thi Thu Hao. "Detection of enteric bacteria in raw food samples from Vietnam and evaluation of antibiotic resistance." Diss. Ph. D. dissertation, RMIT University, Melbourne, Victoria, Australia, 2007.
- Newell, Diane G., et al. "Food-borne diseases-the challenges of 20 years ago still persist while new ones continue to emerge." International Journal of Food Microbiology, Vol. 139, 2010, pp. S3-S15.
- CDC. "CDC estimates of foodborne illness in the United States." 2011.
- Andrew, S. P. "Manual of food quality control (microbiological analysis)." FAO, Rome, 1994, pp. 116-73.
- Food Standards Australia New Zealand. "Guidelines for the microbiological examination of ready-to-eat foods." 2001.
- Walsall C "Sampling food for microbiological examination." Food Safety-Environmental Health Services Division; Huntingdonshire District Council. 2007. www.huntsdc.gov.uk
- Food Safety Authority of Ireland. "Guidelines for the Interpretation of Results of Microbiological Testing of Ready-to-eat Foods Placed on the Market (Revision 1)." Food Safety Authority of Ireland, 2014.
- Downes, F. P., and K. Ito. "Compendium of methods for the microbiological examination of foods Washington (676 p.). USA: American Public Health Association." 2001.
- Codex Alimentarius Commission. "Recommended international code of practice general principles of food hygiene." CAC/RCP, Rev 4, 2003, pp. 1-1969.
- Food, U. S. "The Bad Bug Book: Food-borne pathogenic microorganisms and natural toxins handbook." Second ed, 2012.
- Bryan, Frank L., and World Health Organization. "Hazard analysis critical control point evaluations: a guide to identifying hazards and assessing risks associated with food preparation and storage." World Health Organization, 1992.
- Food and Environmental Hygiene Department (FEHD). "Microbiological guidelines for ready‐to‐eat food." 2006.
- Okello, Julius Juma. "Compliance with international food safety standards: The case of green bean production in Kenyan family farms." Michigan State University, 2005.
- WHO. "Hazard Analysis Critical Control Points System (HACCP) of food processing and food manufacturing." Report of a WHO Consultation; Geneva: WHO, 1997.
- Vaclavik, Vickie A., Elizabeth W. Christian, and Tad Campbell. "Essentials of food science." Vol. 42, New York: Springer, 2008.
- Stranks, Jeremy W. "The AZ of food safety." Thorogood, 2007.
- Series, Microbiological Risk Assessment. "Risk assessments of Salmonella in eggs and broiler chickens." World Health Organization, 2002.
- "Escherichia coli O157:H7." In Foodborne Pathogenic Microorganisms and Natural Toxins Handbook. U.S. Food & Drug Administration, Center for Food Safety & Applied Nutrition, 2002. http://www.cfsan.fda.gov/~mow/chap15.html
- Abd Elrahman, A. E. "Some aerobic bacteria in minced meat sold in Retail shops in Elmukhtar municipality." Diss. M. Sc. Thesis University of Khartoum, Sudan, 1999.
- Ahmed E.B. "Escherichia coli and bacterial load in fried burger sold at Alarabi market, locality of Khartoum." Journal of Art and Sciences, Dallanj University, Vol. 2, 2006 pp. 1-26.
- Hassan, N.A. "Bacterial Contamination of Restaurant food in Khartoum State." M.V.Sc thesis-University of Khartoum, 2006.
- Abdalla, M. A., et al. "Food safety knowledge and practices of street food vendors in Khartoum City." The Sudan Journal of Veterinary Science and Animal Husbandry, Vol. 47, No. 1&2, 2008, pp. 126-36.
- OzFoodNet Working Group. "Monitoring the incidence and causes of diseases potentially transmitted by food in Australia: Annual report of the OzFoodNet Network, 2009." Communicable Diseases Intelligence Quarterly Report, Vol. 34, No. 4, 2010, pp. 396-426.
- Mustafa, Nazik EM, and M. S. Abdallah. "Bacteriological quality of street-vended Um-Jingir: A traditional Sudanese food." African Journal of Food, Agriculture, Nutrition and Development, Vol. 11, No. 5, 2011, pp. 5220-31.
- Elfaki, Ahmed Elawad, and Sally Ali Abdalla Elhakim. "Quality evaluation of two Sudanese street foods of animal origin." Advance Journal of Food Science and Technology, Vol. 3, No. 3, 2011, pp. 219-23.
- Ali, Asmahan A., and Warda S. Abdelgadir. "Incidence of Escherichia coli in raw cow’s milk in Khartoum state." British Journal of Dairy Sciences, Vol. 2, No. 1, 2011, pp. 23-26.
- National Health Information Centre (NHIC). "Annual Health Statistical Report 2007." Federal Ministry of Health-Sudan, 2007.
- Benson, Harold J. "Microbiological applications; a laboratory manual in general microbiology." 1967.
- Cakir, Ibrahim, et al. "The need for confirmation in coliform and E. coli enumeration in foods." Turkish Journal of Veterinary and Animal Sciences, Vol. 26, No. 5, 2002, pp. 1049-53.
- Food Quality Check Program, Microbiological Recommendations, Food Laboratory, Environmental Microbiology BC Public Health Microbiology & Reference Laboratory. British Columbia Centre for Disease Control (BCCDC) 2011. http://lmlabs.phsa.ca/Documents/FoodQualityMicroRecommendations2012_16Dec2011.pdf
- Wong, Julie, Joe Fung and Lynn Wilcott. "Food Quality Check Program Microbiological Recommendations." Food Laboratory, Environmental Microbiology, Public Health Microbiology and Reference Laboratory, 2011.
- Williams, David L., et al. "Assessment of the potential for cross-contamination of food products by reusable shopping bags." Food Protection Trends, Vol. 31, No. 8, 2011, pp. 508-13.
- Odu, N. N., and U. M. Akano. "The microbiological assessment of ready-to-eat-food (Shawarma) in Port Harcourt City, Nigeria." Nature and Science, Vol. 10, No. 8, 2012, pp. 1-8.
- Jay, James Monroe. "Modern food microbiology. Maryland." 2000, pp. 549-63.
- Farzana, Kalsoom, Syed Nisar Hussain Shah, and Farzana Jabeen. "Antibiotic resistance pattern against various isolates of Staphylococcus aureus from raw milk samples." Journal of Research (Science), Vol. 15, No. 2, 2004, pp. 145-51.
- Ray, Bibek, and Arun K. Bhunia. "Fundamental food microbiology." 3rd ed., 2005.
- Ashraf, Rabia, and Nagendra P. Shah. "Antibiotic resistance of probiotic organisms and safety of probiotic dairy products." International Food Research Journal, Vol. 18, No. 3, 2011, pp. 837-53.
- Connecticut Department of Public Health (CDPH), Connecticut Association of Directors of Health (CADH), Inc. and Connecticut Environmental Health Association (CEHA). "Guidance Document: Presence of Total Coliform or Fecal Coliform/ E. coli Bacteria in the Water Supply at Food Service Establishments." 2010.https://authoring-stage.ct.egov.com/-/media/Departments-and Agencies/DPH/dph/drinking_water/pdf/PresenceofTotalColiformatFoodServicepdf.pdf