Case Report - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 4
General Anaesthesia for a Baby with Metachromatic Leukodystrophy
Mustafa Mohammed Salih*Mustafa Mohammed Salih, Department of Paediatric Anaesthesia, Children Welfare Teaching Hospital, Medical City, Baghdad, Iraq, Email: mustafasalih70@gmail.com
Received: 03-Mar-2023, Manuscript No. ijmrhs-23-93913; Editor assigned: 05-Apr-2023, Pre QC No. ijmrhs-23-93913(PQ); Reviewed: 15-Apr-2023, QC No. ijmrhs-23-93913(Q); Revised: 18-Apr-2023, Manuscript No. ijmrhs-23-93913(R); Published: 30-Apr-2023
Abstract
Mitochromatic Leukodystrophy is a progressive degenerative disorder of white matter. Patients with this disease frequently require anaesthesia for various diagnostic and surgical procedures. These patients pose a lot of anaesthetic problems like seizures, spasticity, risk of aspiration, and copious secretions, in addition to other organ dysfunctions. Our case report is about the provision of general anaethesia for a female child for laparoscopic cholecystectomy and gastrostomy tube placement
Keywords
Metachromatic Leukodystrophy (MLD), General anaesthesia, Paediatric
Introduction
Metachromatic Leukodystrophy (MLD) is a genetic disorder that affects nerves, muscles, other organs, and behavior. It belongs to the lysosomal sphingolipid storage group and is listed in the family of leukodystrophies [1]. It is a progressive and neurodegenerative disease mainly affecting the central nervous system’s and peripheral nervous system’s myelin sheath [2].
MLD is caused by a deficiency of the enzyme arylsulfatase A or Saposin B [3]. This deficiency leads to the accumulation of sulfatide which damages myelin in the central and peripheral nervous systems leading to loss of motor and cognitive skills [4]. So it is a typical white matter disease. White matter damage causes progressive deterioration of motor skills. Sulfatide accumulates in other organs like kidneys and gallbladder. Various types of MLD according to age are classified as:
• Late Infantile MLD: (50%‐60%) most common form. Is seen around 2 years of age. Gradual loss of speech and walking (gait disturbance), muscle tone first decrease then increase to a point of rigidity. The patient usually not survives beyond 5 years.
• Juvenile MLD: (20%‐30%) seen in ages between 3 years and 16 years. Frequent falls, convulsions, loss of muscle control, difficulties in speaking and swallowing, later end in decerebrate posture, behavioral problems and mental deterioration, poor school performance, and dementia. The patient dies 10 years‐20 years of the onset of the disease.
• Adult MLD: (15%‐20% ) seen over 16 years of age. Difficulty walking and speaking, diminished vision, loss of hearing, abnormal behavior, psychiatric symptoms like delusions or hallucinations, and progressive dementia [5,6].
MLD is reported to occur in 1in 40,000‐160,000 individuals worldwide [7]. It is inherited as an autosomal recessive trait with a gene located on chromosome 22q.13‐13 qter [8].
MLD patients often require general anaesthesia for diagnostic and therapeutic interventions e.g. magnetic resonant imaging, gastrostomy tube placement, central catheter placement and removal, tendon release surgery, abscess drainage, gastro‐esophageal hernia repair, endoscopy, tracheostomy, and change tracheostomy [9].
This group of patients presents a lot of anaesthetic concerns during the perioperative period like convulsions, risk of aspiration, airway complications, copious oral and tracheobronchial secretions, impaired swallowing, chronic immobility, dystonia, and spasticity [10]. So care must be given to avoid pressure necrosis and iatrogenic fractures during positioning and transfer.
Another anaesthetic concern is that most of these patients can be on anticonvulsant therapy, steroids, or other chronic medications which need continuation during the perioperative period. In addition, attention must be directed to investigate liver function and coagulation searching for any deterioration because of anticonvulsants or adrenal insufficiency because of steroids [11].
Temperature management is a well-known concern in these patients and requires careful consideration.
Case Presentation
Our case is 33 months old girl with a weight of 12 kg. Presented for laparoscopic cholecystectomy and feeding gastrostomy tube placement in Children Welfare Hospital in Baghdad on November 22nd of 2022. Her disease started 3 months ago as progressive muscle weakness started in both lower limbs ascending to include the abdomen and then upper limbs associated with spasticity which led to contractures in both upper and lower limbs, later involving the pharynx leading to difficulties in swallowing.
The patient was on oral Baclofen 4 mg twice daily. It was not interrupted till the time of operation. No history of convulsions or anticonvulsant therapy
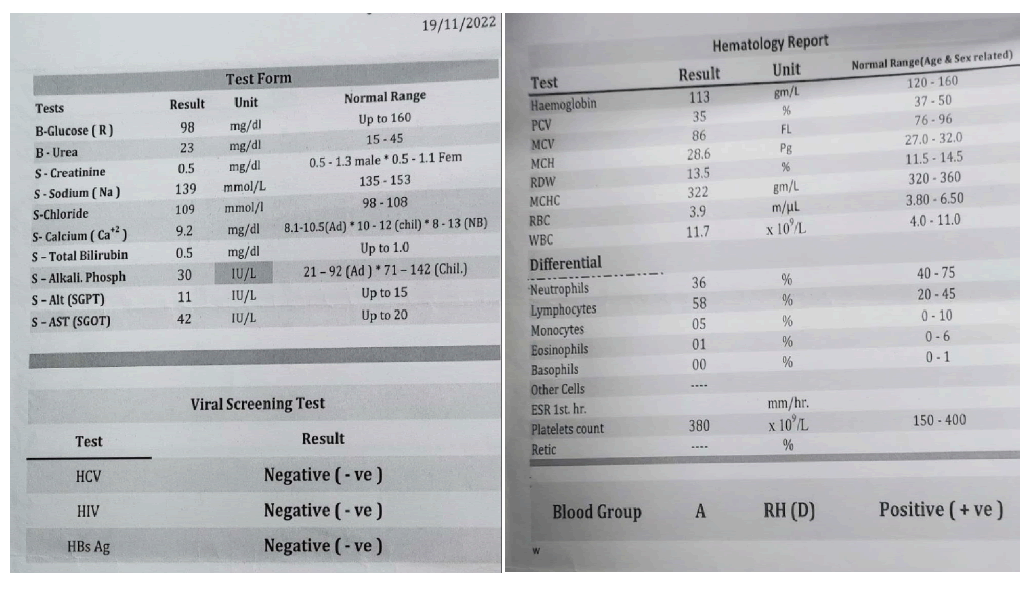
Preoperative laboratory investigations were done including a complete blood picture, blood glucose, serum electrolytes, renal and hepatic function tests, and a coagulation study (Figure 1). All results were within normal apart from an increase in AST level which is explained as a result of Baclofen.
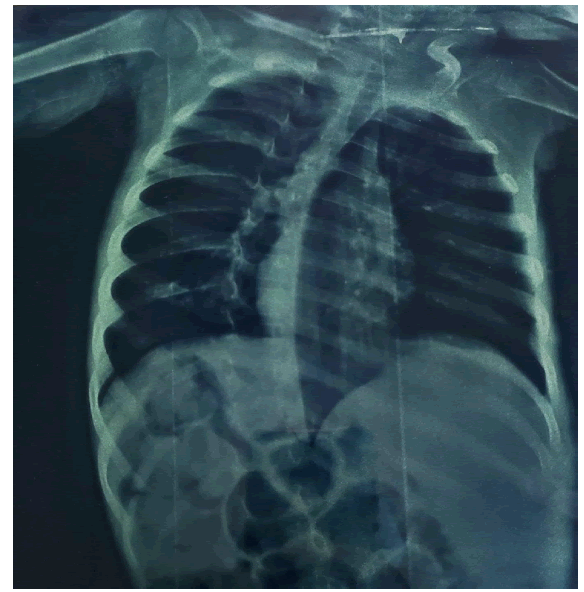
Chest x‐ray shows the lateral deviation of the vertebral column due to spasticity (Figure 2). The ECHO study was normal. Problems expected with induction of Anaesthesia were immobility, spasticity, copious oral secretions, risk of aspiration, and difficult intubation.
At the induction of Anaesthesia vital signs were: Heart Rate (HR)=110 BPM, Respiratory Rate (RR)=22, Blood Pressure (BP)=110/50 mmHg, body temperature=36.6 C, Oxygen saturation (SpO2)=97% (on room air) the patient was anxious and crying. Monitors were connected which included: Pulse oximetry, ECG, NIBP, and Temp. (nasal probe).
The patient was premedicated with Glycopyrrolate 100 µg. I.V. and Esomeperaozole 10 mg. I.V. followed by preoxygenation with 100% O2 for 2 minutes then Midazolam 0.5 mg I.V., oral suctioning, Propofol 20 mg, Remifentanil 10 µg, and Rocuronium 15 mg, cricoid pressure (Rapid Sequence Induction (RSI)), then Laryngoscopy using the usually curved blade, and intubation with 4.5 mm ID cuffed Endotracheal Tube (ETT). We noticed a decrease in the spasticity after propofol which rendered intubation easy. A Nasogastric (NG) tube size 12 FG was inserted easily.
Ventilation was with Pressure-Controlled Volve (PCV) using Inspiratory Pressure (IP) of 11 cm H2O, RR=18, Positive end-Expiratory Pressure (PEEP) =4 cm H2O.
After induction, vital signs were: HR=130 BPM, BP=120/80, EtCO2 =33 mmHg
Maintenance was with Sevoflurane 2% in O2 50%, with Remifentanyl infusion at a rate of 2 ug/min. now HR=104, BP=90/50, Temp=36.1â?? Laparoscopic cholecystectomy started with insufflation pressure of 10 cmH2O, flow of 2 L/min, EtCO2 increased to 40 mmHg. So RR increased to 22/min. The operation lasted 80 minutes (65 minutes laparoscopy and 15 minutes gastrostomy tube placement).
2 increment doses of Rocuronium (2 mg) were given at minutes 30 and 50. 220 ml of Ringer’s solution was given. And Paracetamol 150 mg given. Temperature control was with a forced air warming device (Bair‐Hugger) set at 38℃ which increased to 43℃ to manage the drop in the patient’s temperature to 36.1℃.
At the end of the surgery, the Remifentanyl infusion stopped, after 5 minutes, with the effort of spontaneous breathing, Sugamadex 25 mg was given to reverse muscle relaxant. The patient responded with adequate spontaneous breathing (Vt=140 ml, RR=24/min), she opened her eyes, and coughed. Extubation done.
The patient developed mild spasticity and shivering, she was managed by active warming and Midazolam 0.5 mg. After 15 minutes she was calm, waking with simple tactile stimulation, and breathing comfortably, her SpO2 was 97% with room air, then started crying searching for her parents. So transferred to PICU.
In the PICU, the patient was conscious, crying, spontaneously breathing with an oxygen nasal cannula, and looked in pain, Morphine 1 mg iv., and Baclofen 4 mg were given through a gastrostomy tube. At night spasticity returned to a preoperative state, the night dose of Baclofen 4 mg was given through a gastrostomy tube.
Postoperative day; spasticity continued as same, and vital signs were stable. The patient was discharged to the ward.
Discussion
MLD is a white matter disease. It is a disorder of myelin sheath that affects central and peripheral nervous systems. In the late infantile type, as in our case, peripheral neuropathy can be the initial symptom, before central progression [1].
Continuation of the usual treatment of anticonvulsants, steroids, or muscle relaxants (Baclofen) is very important, as sudden withdrawal may lead to convulsions, adrenal insufficiency, and increased spasticity.
Baclofen acts on GABA‐B receptors in the dorsal horn of the spinal cord. So it is a centrally-acting muscle relaxant that is effective in relieving muscle spasms. Sudden withdrawal leads to seizures [1]. Interferences are possible between baclofen and curare and general anaesthetics. They may be responsible for neuromuscular block augmentation, heart rhythm disorders, arterial hypotension, or increased sedation but weaning is much more [12]. However, it is documented that Baclofen can cause hepatic injury and elevated liver enzymes [13]. As the disease progresses it leads to dysphagia and drooling of secretions that need placement of gastrostomy which facilitates feeding. The risk of aspiration is present because of that. So Rapid Sequence Induction (RSI) is the choice. Premedication started with Glycopyrrolate to decrease copious secretions with minimal effect on heart rate, and Proton Pump Inhibitor (Esomeprazole) is given to decrease gastric acidity. Midazolam is given to decrease muscle tone and increase the convulsion threshold.
Both inhalation and intravenous induction are safe. However, intravenous induction is preferred because of rapid onset which meets the requirement of RSI, in addition to the availability of IV. line. Propofol, Thiopentone, 10 Sevoflurane, Isoflurane, opiates, and local anaesthtics all have been used without complication [1]. Ketamine should be avoided due to its ability to lower the seizure threshold [14].
We avoided Succinylcholine due to the theoretical risk of hyperkalemic cardiac arrest because of exrtraâ?ÂÂjunctional receptors proliferation. However, there are no reported cases of its use in MDL [1]. Another cause to avoid Succinylcholine is its fasciculation which may cause iatrogenic bone fracture
So, RSI reverted to the modified version; using Rocuronium 1 mg/kg with cricoid pressure. Non-depolarizing neuromuscular blockers (Atracurium, Rocuronium, and vecuronium) have been noted to be safe in these patients.1 Intraoperative doses of IV. anaesthetics and muscle relaxants need to be increased due to increased hepatic enzyme function seen in patients on chronic anticonvulsant therapy [15].
Maintenance continues with Sevoflurane and Remifentanil infusion as both are documented to be safe for this child, in addition to their properties in being short-acting agents which do not prolong the postoperative period [16]. Special care is given to temperature control to avoid shivering and increase oxygen demand. Measures such as raising operating room temperature, warming of IV. Fluid, using a closed circuit, and using of forced air warmer device which is an effective method to avoid hypothermia [17].
Care is also given to posture and transport to avoid pressure necrosis and iatrogenic fractures which result from malnutrition and spasticity [15].
Reversal of neuromuscular blockade is done with Sugammadex (2 mg/kg) which is an effective reversal of Rocuronium, although Neostigmine is also appropriate and documented for antagonism of neuromuscular blockers for these patients [1].
Potential complications from sedation are hypoxia, vomiting, bradycardia, arrhythmia, and convulsion. Documented complications post‐extubations are hypothermia, aspiration pneumonia, and bronchospasm [16].
Postoperative critical care is required for frequent suctioning, chest physiotherapy, and positioning. It is important to consider pain management, temperature control, continuous monitoring, and most important, continuation of preoperative medications (anticonvulsants, steroids, etc.) to avoid withdrawal symptoms of these drugs. The patient was not on chronic steroid therapy, so we did not find an indication to add steroids to the management as it is not wise to add side effects of steroids in the face of uncertain benefits. The patient was not on chronic steroid therapy, so we did not find an indication to add steroids to the management as it is not wise to add side effects of steroids in the face of uncertain benefits
Regional anaesthesia has been relatively contraindicated in patients with a neurological disorder, in addition, to abnormal posture and difficult communication with the baby. But Hernandez‐Palazon et al. used epidural anaesthesia in patients with metachromatic leukodystrophy for pain management [1].
Conclusion
MLD frequently requires general anaesthesia for surgical procedures aimed to correct the sequelae of the disease. It presents a lot of anaesthetic problems during the perioperative period and carries risks of many anaesthetic complications. However, the management of these patients needs special attention and a thorough knowledge of these issues that will result in better outcomes. Identification of these issues in the preoperative assessment of the patient and careful selection of anaesthetic techniques will allow the provision of safe anaesthetic care.
Nevertheless, reports suggest that the complication rate may be substantially lower than suspected, and the benefits of the necessary procedures significantly outweigh the risks. So we can say confidently, that in experienced hands general anaesthesia is well tolerated in most of these children.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This research did not receive any specific grant or funding from agencies, the public, commercial, or not-for-profit sectors.
References
- Hernandezâ?Palazon, Joaquin. "Anaesthetic management in children with metachromatic leukodystrophy." Pediatric Anesthesia, Vol. 13, No. 8, 2003, pp. 733-34.
Google Scholar Crossref - Kevelam, Sietske H., et al. "Update on leukodystrophies: a historical perspective and adapted definition." Neuropediatrics, Vol. 47, No. 06, 2016, pp. 349-54.
Google Scholar Crossref - Roghi, Christian, et al. "Golgi reassembly stacking protein 55 interacts with membraneâ?type (MT) 1â?matrix metalloprotease (MMP) and furin and plays a role in the activation of the MT1â?MMP zymogen." The FEBS journal, Vol. 277, No. 15, 2010, pp. 3158-75.
Google Scholar Crossref - Shaimardanova, Alisa A., et al. "Metachromatic leukodystrophy: diagnosis, modeling, and treatment approaches." Frontiers in medicine, Vol. 7, 2020.
Google Scholar Crossref - Kwon, Jennifer M. "Neurodegenerative disorders of childhood." Nelson Textbook of Pediatrics, 21st ed, 2016, pp. 2011-73.
Google Scholar - Turnpenny, P. D., S. Ellard, and R. Cleaver. "Inborn errors of metabolism." Emery’s Elements of Medical Genetics. 15th ed. Philadelphia, PA: Elsevier 2017.
Google Scholar - Deconinck, Nicolas, et al. "Metachromatic leukodystrophy without arylsulfatase A deficiency: a new case of saposin-B deficiency." European Journal of Paediatric Neurology, Vol. 12, No. 1, 2008, pp. 46-50.
Google Scholar Crossref - Gupta, Arun Kumar, et al. "Anaesthetic Implications in a Case of Metabolic Leukodystrophy." Colombian Journal of Anestesiology, Vol. 38, No. 2, 2010, pp. 234-39.
Google Scholar - Escolar, Maria L., et al. "Clinical management of K rabbe disease." Journal of neuroscience research, Vol. 94, No. 11, 2016, pp. 1118-25.
Google Scholar Crossref - Mattioli, Cristina, et al. "Sedation for children with metachromatic leukodystrophy undergoing MRI." Pediatric Anesthesia, Vol. 17, No. 1, 2007, pp. 64-69.
Google Scholar Crossref - Kindopp, A. Shawn, and Ted Ashbury. "Anaesthetic management of an adult patient with X-linked adrenoleukodystrophy." Canadian journal of anaesthesia, Vol. 45, 1998, pp. 990-92.
Google Scholar Crossref - Mohammed, Imran, and Asif Hussain. "Intrathecal baclofen withdrawal syndrome-a life-threatening complication of baclofen pump: a case report." BMC Clinical Pharmacology, Vol. 4, No. 1, 2004, pp. 1-5.
Google Scholar Crossref - Chen, Minjun, et al. "DILIrank: the largest reference drug list ranked by the risk for developing drug-induced liver injury in humans." Drug Discov Today, Vol. 21, No. 4, 2016, pp. 648-53.
Google Scholar Crossref - Gemma, M., et al. "Sedation in paediatric patients affected by Metachromatic Leukodystrophy: A-626." European Journal of Anaesthesiology, Vol. 23, 2006, p. 163.
Google Scholar - Tobias, Joseph D. "Anaesthetic considerations for the child with leukodystrophy." Canadian journal of anaesthesia, Vol. 39, 1992, pp. 394-97.
Google Scholar Crossref - Taguchi, Akiko, et al. "Effects of a circulating-water garment and forced-air warming on body heat content and core temperature." The Journal of the American Society of Anesthesiologists, Vol. 100, No. 5, 2004, pp. 1058-64.
Google Scholar Crossref - Bascou, Nicholas A., et al. "General anesthesia safety in progressive leukodystrophies: A retrospective study of patients with Krabbe disease and metachromatic leukodystrophy." Pediatric Anesthesia, Vol. 29, No. 10, 2019, pp. 1053-59.
Google Scholar Crossref