Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 6
Glycemic Indices in Overweight or Obese Subjects with or without Obstructive Sleep Apnea: A Cross-Sectional Analytical Study
Nitin Damsadekar1* and Swati Varshney22Department of Hospital Administration, Armed Forces Medical College, Pune, India
Nitin Damsadekar, Department of Internal Medicine, Base Hospital,, Tezpur, Assam, India, Email: nitindams@gmail.com
Received: 19-May-2021 Accepted Date: Jun 23, 2021 ; Published: 30-Jun-2021
Abstract
Background: Obesity is a known risk factor for both Type 2 Diabetes Mellitus (DM) and Obstructive Sleep Apnea (OSA). The relationship between obesity and these two disorders is complex and multifactorial. The aim is to study the prevalence of OSA in overweight and obese subjects and its association with Type 2 DM and other metabolic abnormalities.
Materials and Methods: This cross-sectional analytical study was performed on 100 subjects with overweight/obese subjects in the age group of 18-65 yrs. OSA was diagnosed by overnight Polysomnography (PSG) and DM was confirmed with an oral glucose tolerance test, insulin resistance and secretion status were assessed by C-peptide and HOMA-IR.
Results: Mean weight of patients with OSA was 79.41 kg while that of those without OSA was 72.62 kg. Further, the mean fasting blood glucose of those with OSA was 142.4 ± 17.3 mg% and of those without OSA was 133.3 ± 7.7 mg%. Similarly, the mean fasting insulin level of those with OSA was 16.11 ± 10.47 uIU/mL while of those without OSA was 18.3 ± 22.06 uIU/mL. These correlations were found to be statistically significant.
Conclusion: Obesity, Type 2 DM, and cardio-metabolic events are all correlated. The study provides clear evidence that obstructive sleep apnea is associated with insulin resistance. Evaluation of insulin resistance in obese individuals with OSA should be highlighted and evaluated for early detection of metabolic diseasese.
Keywords
Obstructive sleep apnea, Type 2 diabetes mellitus, Obese, C-peptide, HOMA-IR
Introduction
Background
Obesity is now an epidemic worldwide and has been recently recognized as a disease by the United States in 2013 [1]. In 2016 over 1.9 billion adults worldwide were overweight, of whom more than 650 million were obese (39% vs. 13% of the global population respectively) [2]. Obesity is considered a major precipitating factor for many systemic illnesses.
Obstructive Sleep Apnea (OSA) is defined as cessation of airflow due to upper airway collapse lasting at least 10 seconds. Obstructive hypopneas are characterized by ≥ 50% decrease in airflow from baseline lasting at least 10 seconds associated with 4% oxygen desaturation [3]. These disruptions in breathing lead to intermittent blood gas disturbances (hypercapnia and hypoxemia) and surges of sympathetic activation which result in cyclical breathing patterns and fragmented sleep as the patient oscillate between wakefulness and sleep.
OSA is found to be two to three times greater in men than in women [4]. Prevalence estimates of OSA in obese adults (aged 30-69 years) range from 33% to 77% in men and 11% to 46% in women [5]. Moreover, weight gain increased the incidence and severity of OSA [6]. There is emerging evidence to suggest that OSA is an independent risk factor for a variety of adverse cardiovascular outcomes [7]. The clinical disorder, defined as more than five abnormal breathing disturbances (hypopneas or apnea) per hour of sleep combined with symptoms of daytime sleepiness, affects at least 2%-4% of the adult population [8]. Indeed, an increase in body mass index, central accumulation of adipose tissue, and neck circumference are strong predictors of disease [9,10]. Also, there is a rising interest in studying cardio-metabolic derangements associated with OSA [11-13]. Data suggesting the role of OSA in adverse cardiovascular outcomes exists in multiple studies [14-16].
Objectives
• To study the prevalence of OSA in overweight and obese subjects
• To compare blood glucose levels in overweight and obese individuals in those with and those without obstructive sleep apnea
• To determine the correlation between insulin level and resistance with obstructive sleep apnea
Despite the independent associations between OSA and abnormal glucose metabolism and the high prevalence of OSA in patients with type 2 DM, data on whether the presence and severity of OSA compromise glycemic control in patients with type 2 DM is lacking. Currently, both physicians and patients are challenged by rising concerns about the safety of widely used pharmacologic treatment options [17]. Determining whether OSA has an adverse effect on glucose control in patients with diabetes has major clinical implications because effective treatment of OSA could be a non-pharmacologic strategy to improve glucose control in the management of patients with type 2 DM. Furthermore, successful initiation of Continuous Positive Airway Pressure (CPAP) therapy may be associated with improved insulin sensitivity and reduced HbA1c levels, suggesting a potential contributory role of sleep-disordered breathing in dysglycaemia [18,19]. The present cross-sectional analytical study was done at a tertiary care center to determine the prevalence of sleep apnea among the overweight and obese population and compare glycaemic indices in obese subjects with or without sleep apnea.
Methodology
After approval from the Institutional Ethical Committee, valid informed consent was taken in writing from all the subjects. Once the patients were enrolled for the study, a thorough history and physical examination were done as per proforma.
Inclusion Criteria
• Age between 18-65 years
• BMI ≥ 23 kg/m2
Exclusion Criteria
• Pre-existing DM
• Pre-existing Hypertension
• Pregnancy
• Chronic Liver/Kidney disease
• Patient on steroid therapy for any cause for >3 months
• Concomitant use of any nephrotoxic drug for >3 months
Data were recorded for each patient including demographic details, anthropometric and clinical variables, including Body Mass Index (BMI), smoking history, alcohol intake with details of comorbidities, and medication use. Initial screening was done to exclude all pre-existing systemic illnesses as per the inclusion/exclusion criteria. BMI was calculated with height and weight assessment.
Overnight PSG (for ≥ 6h) was done for all the subjects at the hospital wherein apnea was defined as the termination of respiratory airflow for ≥ 10s, and hypopnea defined as ≥ 50% decrease in ventilation accompanied by ≥ 4% decrease in oxygen saturation.
The cases and controls were decided by the presence or absence of OSA depending on the results of PSG. Prevalence of risk factors for metabolic syndrome, i.e. assessment of glycemic indices was done for both cases and controls.
Statistical Analysis
Quantitative data are presented with the help of mean and standard deviation. Comparison among the study groups is done with the help of unpaired t-test as per results of normality test. Qualitative data are presented with the help of frequency and percentage tables. Association among the study groups is assessed with the help of the Fisher test, Student ‘t’ test, and Chi-Square test. p-value less than 0.05 is taken as significant.
Pearson’s Chi-Squared Test
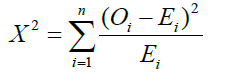
Where Χ2=Pearson’s cumulative test statistic;
Oi=an observed frequency;
Ei=an expected frequency, asserted by the null hypothesis;
n=the number of cells in the table
Results are graphically represented where deemed necessary.
Appropriate statistical software, including but not restricted to MS Excel, SPSS ver. 20 was used for statistical analysis. Graphical representation is done using MS Excel 2010.
Results
A total of 100 patients were studied to determine the prevalence of sleep apnea among the overweight or obese population and to compare the indices of glycemia and insulin in subjects with or without sleep apnea. Following were the findings
Gender Variation
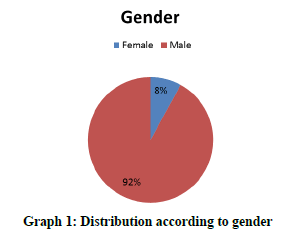
92% of patients were males while 8% of patients were females (Graph 1).
Presence of OSA
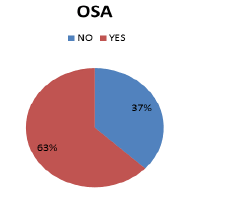
Obstructive Sleep Apnea (OSA) was found in 63% of patients while 37% of patients did not have OSA (Graph 2).
Age Association
No significant association between age and obstructive sleep apnea was observed. The mean age of those with OSA present was 47.83 ± 11.16 years and those with OSA absent were 45.92 ± 8.315 years (Table 1).
| Age (Years) | N | Mean | Std. Deviation | Minimum | Maximum | F | p-value |
|---|---|---|---|---|---|---|---|
| OSA Present | 63 | 47.83 | 11.165 | 27 | 74 | 0.813 | 0.37 |
| OSA Absent | 37 | 45.92 | 8.315 | 22 | 61 | ||
| Total | 100 | 47.12 | 10.201 | 22 | 74 |
Table 1: Association of age with obstructive sleep apnea
BMI Association
No significant association of BMI with obstructive sleep apnea was observed in our study. The mean BMI of those with OSA present was 30.78 ± 5.9 kg/m2 while the mean BMI of those with absent OSA was 29 ± 6.7 kg/m2 (Table 2).
| BMI (kg/m2) | N | Mean | Std. Deviation | Minimum | Maximum | F | p-value |
|---|---|---|---|---|---|---|---|
| OSA Present | 63 | 30.07848 | 5.910502 | 23.12 | 47.1 | 0.034 | 0.853 |
| OSA Absent | 37 | 29.8387 | 6.785326 | 23 | 47.1338 | ||
| Total | 100 | 29.98976 | 6.215583 | 23 | 47.1338 |
Table 2: Association of BMI with obstructive sleep apnea
Fasting Blood Glucose Level Association
The study found a significant statistical association between fasting blood glucose level (mg%) and obstructive sleep apnea. Mean fasting blood glucose of those with OSA was 142.4 ± 17.3 mg% while mean fasting blood glucose of those without OSA was 133.3 ± 7.7 mg% (Table 3).
| Fasting blood glucose (mg%) | N | Mean | Std. Deviation | Minimum | Maximum | F | p-value |
|---|---|---|---|---|---|---|---|
| OSA Present | 63 | 142.43 | 17.316 | 126 | 198 | 9.171 | 0.003 |
| OSA Absent | 37 | 133.3 | 7.781 | 126 | 165 | ||
| Total | 100 | 139.05 | 15.147 | 126 | 198 |
Table 3: Association of fasting blood glucose (mg%) with OSA
Fasting Serum Insulin Level Association
A significant association was noted between fasting serum insulin level and obstructive sleep apnea. The mean fasting insulin of those with OSA was 16.11 ± 10.47 uIU/mL while the mean fasting insulin of those without OSA was 18.3 ± 22.06 uIU/mL (Table 4).
| Fasting S Insulin Level uIU/mL | N | Mean | Std. Deviation | Minimum | Maximum | F | p-value |
|---|---|---|---|---|---|---|---|
| OSA Present | 63 | 16.11 | 10.47 | 0.01 | 48.07 | 1.48 | 0.04 |
| OSA Absent | 37 | 18.39 | 22.06 | 0.93 | 138.4 | ||
| Total | 100 | 16.95 | 15.711 | 0.01 | 138.4 |
Table 4: Association of fasting serum insulin level with OSA
C-peptide Level Association
A significant association was observed between C-peptide and obstructive sleep apnea. The mean C-peptide of those with OSA was 1774.1 ± 918.48 pmol/mL while the mean C-peptide of those without OSA was 1906.4 ± 885.2 pmol/ mL (Table 5).
| C-peptide (pmol/mL) | N | Mean | Std. Deviation | Minimum | Maximum | F | p-value |
|---|---|---|---|---|---|---|---|
| OSA Present | 63 | 1774.163 | 918.4873 | 0.34 | 3419 | 0.496 | 0.483 |
| OSA Absent | 37 | 1906.43 | 885.2669 | 35.6 | 3973 | ||
| Total | 100 | 1823.101 | 904.1167 | 0.34 | 3973 |
Table 5: Association of C-peptide with obstructive sleep apnea
HOMA-IR Value Association
No significant association was noted between HOMA-IR and obstructive sleep apnea. The mean HOMA-IR of those with OSA was 5.6 ± 3.9 mmol/I while the mean HOMA-IR of those without OSA was 6.08 ± 7.09 m (Table 6).
| HOMA-IR Fasting Insulin x Fasting Glucose (nmol/l)/22.5 | N | Mean | Std. Deviation | Minimum | Maximum | F | p-value |
|---|---|---|---|---|---|---|---|
| OSA Present | 63 | 5.67 | 3.98 | 0.0033 | 22.0766 | 0.13 | 0.71 |
| OSA Absent | 37 | 6.08 | 7.09 | 0.3169 | 43.7412 | ||
| Total | 100 | 5.82 | 5.31 | 0.0033 | 43.7412 |
Table 6: Association of HOMA-IR with Obstructive Sleep Apnea
Discussion
The hospital-based cross-sectional analytical study was conducted with 100 patients to determine the prevalence of sleep apnea among the overweight or obese population and to compare the indices of glycemia and insulin (secretion and resistance) in subjects with or without sleep apnea.
In the present study, 92% of patients were males while 8% of patients were females. No Obstructive Sleep Apnea (OSA) was found in 37% of patients while 63% of patients had OSA. Similar prevalence data was found in the studies by Aronsohn RS, et al. and Soin D, et al. [20,21].
In our study, no significant association was reported between age and obstructive sleep apnea. This is comparable to the studies of Soin D, et al. and Kent BD, et al. [21,22].
Our study did not find any significant association between BMI and OSA. But the studies by Aronsohn RS, et al., Kurosawa H, et al., and Abu Youssef HA, et al. found BMI to be significantly associated with OSA [20,23,24]. This variation may be because this study included all subjects with BMI above 23 kg/m2, subjects with lower BMI were excluded.
A significant association was observed between fasting glucose (mg%) and obstructive sleep apnea. Kent BD, et al. and Abu Youssef HA, et al. also noted similar significant associations in their works [22,24].
Our study found that a significant association existed between fasting serum insulin level and OSA. This finding is strongly supported by the studies done by Aronsohn RS, et al., Kent BD, et al., Kurosawa H, et al., Abu Youssef HA, et al., Baburao A, et al. and Priou P, et al. [20,22-26].
In the present study, no significant association was observed between obstructive sleep apnea with that of C-peptide or HOMA IR. Results in a study by Baburao A, et al. had similar findings [25]. However, studies of Aronsohn RS, et al., Kurosawa H, et al., Abu Youssef HA, et al., Barcelo, et al., and Ip M, et al. showed a significant relationship between HOMA IR and OSA [20,23,24,27,28]. Probably, further detailed studies with higher sample size and diverse group of subjects are required to study the relationship between OSA and insulin resistance keeping in view the associated factors like HbA1c levels.
Conclusion
Obesity, Type 2 DM, and cardio-metabolic events are all correlated. This study provides clear evidence that Obstructive Sleep Apnea is associated with insulin resistance and has practical implications in the prevention as well as management of diabetes and other metabolic diseases in the obese population. Evaluation of insulin resistance in obese individuals with OSA should be highlighted and evaluated for early detection of metabolic diseases. Further studies are needed to define the mechanism through which OSA promotes insulin resistance. We would also recommend further study to determine whether sustained treatment of OSA reverses the associated metabolic disturbance.
Strengths
This study highlights the vicious relationship between OSA and metabolic syndrome. There is a high prevalence of OSA in patients with metabolic syndrome and the increasing severity of OSA is associated with poor control of diabetes, hypertension, and dyslipidemia which are all components of metabolic syndrome.
This study reinforces the urgent need for early evaluation of OSA in patients with metabolic syndrome and utilizes the relationship in improving the prognoses.
Limitations
This study has a small sample size with a two-year time frame, which is relatively not a good representation of subjects with or without OSA by potentially reducing statistical power. To determine a better correlation study, it will be appropriate to employ a larger number of subjects with a matching case-control design with BMI and matching demographic backgrounds.
In the evaluation of insulin resistance, the gold standard is the euglycemic clamp method. However, it is expensive, invasive, and labor-intensive. Instead, we used HOMA IR which is a useful guide to insulin resistance in normoglycemic individuals. It is a simple and inexpensive alternative, used in large clinical and epidemiological studies. Moreover, there was a lesser representation of female subjects in this study due to the predominantly male population catered by the hospital, which influenced our ability to detect or find any relationship between insulin resistance and gender.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Pollack, Andrew. "AMA recognizes obesity as a disease."The New York Times,Vol. 18, 2013.
- World Health Organization. "World Health Organization obesity and overweight fact sheet." 2018.
- American Academy of Sleep Medicine. "International classification of sleep disorders."Diagnostic and Coding Manual,2005, pp. 51-55.
- Bixler, Edward O., et al. "Prevalence of sleep-disordered breathing in women: Effects of gender."American Journal of Respiratory and Critical Care Medicine,Vol. 163, No. 3, 2001, pp. 608-13.
- Young, Terry, Paul E. Peppard, and Shahrad Taheri. "Excess weight and sleep-disordered breathing."Journal of Applied Physiology,Vol. 99, No. 4, 2005, pp. 1592-99.
- Peppard, Paul E., et al. "Longitudinal study of moderate weight change and sleep-disordered breathing."JAMA,Vol. 284, No. 23, 2000, pp. 3015-21.
- McNicholas, W. T., M. R. Bonsignore, and Management Committee of EU Cost Action B26. "Sleep apnoea as an independent risk factor for cardiovascular disease: Current evidence, basic mechanisms and research priorities."European Respiratory Journal,Vol. 29, No. 1, 2007, pp. 156-78.
- Young, Terry, et al. "The occurrence of sleep-disordered breathing among middle-aged adults."New England Journal of Medicine,Vol. 328, No. 17, 1993, pp. 1230-35.
- Young, Terry, James Skatrud, and Paul E. Peppard. "Risk factors for obstructive sleep apnea in adults."JAMA,Vol. 291, No. 16, 2004, pp. 2013-16.
- Bixler, Edward O., et al. "Effects of age on sleep apnea in men: I. Prevalence and severity."American Journal of Respiratory and Critical Care Medicine,Vol. 157, No. 1, 1998, pp. 144-48.
- Punjabi, Naresh M., and Vsevolod Y. Polotsky. "Disorders of glucose metabolism in sleep apnea."Journal of Applied Physiology,Vol. 99, No. 5, 2005, pp. 1998-2007.
- Somers, Virend K., et al. "Sleep apnea and cardiovascular disease: An American heart association/American college of cardiology foundation scientific statement from the American heart association council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing in collaboration with the national heart, lung, and blood institute national center on sleep disorders research (national institutes of health)."Journal of the American College of Cardiology,Vol. 52, No. 8, 2008, pp. 686-717.
- Tasali, Esra, and Mary SM Ip. "Obstructive sleep apnea and metabolic syndrome: Alterations in glucose metabolism and inflammation."Proceedings of the American Thoracic Society,Vol. 5, No. 2, 2008, pp. 207-17.
- Yaggi, H. Klar, et al. "Obstructive sleep apnea as a risk factor for stroke and death."New England Journal of Medicine,Vol. 353, No. 19, 2005, pp. 2034-41.
- Young, Terry, et al. "Sleep disordered breathing and mortality: Eighteen-year follow-up of the Wisconsin sleep cohort."Sleep,Vol. 31, No. 8, 2008, pp. 1071-78.
- Redline, Susan, et al. "Obstructive sleep apnea-hypopnea and incident stroke: The sleep heart health study."American Journal of Respiratory and Critical Care Medicine,Vol. 182, No. 2, 2010, pp. 269-77.
- American Diabetes Association. "Standards of medical care in diabetes-2009."Diabetes Care,Vol. 32, No. Suppl 1, 2009, pp. S13-S61.
- Lam, J. C. M., et al. "A randomised controlled trial of nasal continuous positive airway pressure on insulin sensitivity in obstructive sleep apnoea."European Respiratory Journal,Vol. 35, No. 1, 2010, pp. 138-45.
- Sharma, Surendra K., et al. "CPAP for the metabolic syndrome in patients with obstructive sleep apnea."New England Journal of Medicine,Vol. 365, No. 24, 2011, pp. 2277-86.
- Aronsohn, Renee S., et al. "Impact of untreated obstructive sleep apnea on glucose control in type 2 diabetes."American Journal of Respiratory and Critical Care Medicine,Vol. 181, No. 5, 2010, pp. 507-13.
- Soin, Divya, et al. "Evaluation of obstructive sleep apnea in metabolic syndrome."Journal of Family Medicine and Primary Care,Vol. 8, No. 5, 2019, pp. 1580-86.
- Kent, Brian D., et al. "Sleep apnoea severity independently predicts glycaemic health in nondiabetic subjects: The ESADA study."European Respiratory Journal,Vol. 44, No. 1, 2014, pp. 130-39.
- Kurosawa, Hideaki, et al. "Association between severity of obstructive sleep apnea and glycated hemoglobin level in Japanese individuals with and without diabetes."Endocrine Journal,Vol. 65, No. 1, 2017.
- Youssef, Hoda A. Abu, et al. "Insulin resistance in obstructive sleep apnea."Egyptian Journal of Chest Diseases and Tuberculosis,Vol. 63, No. 1, 2014, pp. 133-39.
- Baburao, Archana, and George D. Souza. "Insulin resistance in moderate to severe obstructive sleep apnea in nondiabetics and its response to continuous positive airway pressure treatment."North American Journal of Medical Sciences,Vol. 6, No. 10, 2014, pp. 500-04.
- Priou, Pascaline, et al. "Independent association between obstructive sleep apnea severity and glycated hemoglobin in adults without diabetes."Diabetes Care,Vol. 35, No. 9, 2012, pp. 1902-06.
- Barceló, Antonia, et al. "Insulin resistance and daytime sleepiness in patients with sleep apnoea."Thorax,Vol. 63, No. 11, 2008, pp. 946-50.
- Ip, Mary SM, et al. "Obstructive sleep apnea is independently associated with insulin resistance."American Journal of Respiratory and Critical Care Medicine,Vol. 165, No. 5, 2002, pp. 670-76.