Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 5
Inoperable Advanced Head and Neck Cancers: Is COVID-19 Pandemic the Culprit? Our Analysis at a Tertiary Care Hospital
Shahid Rasool*, Shifa Qureshi, Subashree Velmurgun, Mahwish Fatima, Ayushi Manghani and Khaja NaseeruddinShahid Rasool, Department of ENT-HNS, Hamdard Institute of Medical Sciences, New Delhi, India, Email: drshahidgmc@gmail.com
Received: 07-Mar-2022, Manuscript No. ijmrhs-22-56451; Editor assigned: 11-Mar-2022, Pre QC No. ijmrhs-22-56451 (PQ); Reviewed: 21-Mar-2022, QC No. ijmrhs-22-56451 (Q); Revised: 04-May-2022, Manuscript No. ijmrhs-22-56451 (R); Published: 11-May-2022
Abstract
Objectives: To study the effect of the COVID-19 pandemic on Head and neck cancers and its impact on upgrading the stage and in-operability due to delay in seeking health care provision. Study design: This is a retrospective crosssectional study. Settings: Institutional medical record database. Methods: The number of HNC cases that visited our health care facility for a period of 14 months during the pandemic from March 2020 to May 2021 were studied, these cases were compared with HNC cases who attended the facility before the pandemic for an equal number of 14 months, until 1st lockdown was announced in March 2020 by the Government of India. Information about patients was extracted and gathered from the medical records of the hospital and supplemented by telephone interviews. Results: Most of the cases were males above 40 years of age with a male: female ratio of 4.25:1. The most common site of origin was the oral tongue (40%). The total number of new head and neck cancer cases visiting our facility in pandemic and pre-pandemic times were similar with no major difference (63 vs. 65). However, during the lockdown, these numbers dropped to less than half (6 per 3 months). Most of the patients presented with advanced stages (III/IV) of disease during both pandemics as well as pre-pandemic times with no significant difference observed (68.25% vs. 60%). However, a higher incidence of unresectable/inoperable (IVb) advanced cases was seen during pandemic months (30%) compared to pre-pandemic months (7.6%) and these findings were statistically significant (p-value of 0.011). Two third (n=8/12) among these advanced inoperable (IVb) cases had a delay of more than 3 months and one third (4/12) had a delay of more than 6 months in seeking medical advice. Moreover, there was no delay in diagnosing the cases after their contact with our health care facility as almost all cases were diagnosed histopathologically within the first 2 weeks. Conclusion: The author concludes that the COVID-19 pandemic has had a drastic effect on the comprehensive management of Head and Neck cancers. Delay in seeking medical advice and thus diagnosis and initiation of treatment render a huge number of cases inoperable.
Keywords
COVID-19, Corona, Head and Neck cancers, Inoperable tumors
Introduction
COVID-19 disease was declared a pandemic by the world health organization (WHO) on 11th March 2020 [1]. As of 21st June 2021, more than 3,864,180 lives have been claimed, and more than 178,118,597 people have been infected by this deadly virus [2]. Several control measures have been put in place to halt the spread of the disease worldwide which include strict lockdowns in many countries. These COVID lockdowns have been effective in reducing the spread of COVID-19 across the globe [3]. In India, most hospitals have stopped elective operative interventions. Routine outpatient departments have been restricted or stopped; wards have been emptied to make space for the rising number of cases claimed by the highly infectious virus [4]. The heightened restrictions for non-COVID patients have invariably caused them to seek healthcare in a delayed way, and poorly affected its quality when they do receive it [5]. Of these patients, Head and Neck Cancer (HNC) patients are one of the worst-hit [6]. HNCS are considered semi-emergency conditions, given that their doubling time is between 15 to 99 days, and it has been found that almost 79% of patients have had underactive treatment because of delays in seeking treatment [7]. Delaying treatment decreases survival in these patients substantially [8]. Overall, it is predicted that there will be a 20% increase in cancer-related mortality due to the COVID-19 pandemic [9]. While efforts have been made to mitigate the adverse outcomes of non-COVID-19 patients at this time, for example with the creation of ‘cancer hubs’ in the UK where cancer patients were fast-tracked on a priority basis, there is still a great unfulfilled need for providing efficient healthcare of this subset of patients across the world [10].
The current study aims to study the effect of COVID-19 on head and neck tumors and its impact on upgrading the stage and in-operability due to delays in seeking health care provision.
Methods
This is a retrospective cross-sectional study done at Hamdard Institute of Medical Science and Research Centre, a tertiary care hospital of Jamia Hamdard University, New Delhi. The current study aims to study the effect of the COVID-19 pandemic on comprehensive management of head and neck cancers by upgrading the stage and thus in-operability due to delay in seeking health care provision. The effect of pandemic restrictions and lockdowns, fear of catching COVID-19 infections, redistribution of healthcare resources, and change in priorities with more focus on COVID-19 cases were some of the potential variables affecting the delay in seeking health care by patients harboring head and neck cancers. The number of HNC cases that visited our health care facility for a period of 14 months during this pandemic from March 2020 to May 2021 were studied and compared with the data of pre-pandemic patient records from January 2019 to Feb 2020 for an equal number of 14 months, until 1st lockdown was announced in march 2020 by the government of India. Information about patients was extracted and gathered from the medical records of the hospital and supplemented by telephone interviews. As the government of India announced two strict lockdowns of 3 months duration each, between March to May 2020 and 2021 respectively, the total number of cases attending our facility was divided into 3 monthly intervals as lockdown and post-lockdown cases. Clinicopathological parameters such as the following were studied and compared between two cohorts of patients.
• Duration of symptoms ( Appearance of the First symptom until first medical advice was sought)
• Time interval at diagnosis (Appearance of the First symptom until Histopathological diagnosis was arrived at)
• Stage of tumor
• In-operability/unresectability
The study was approved by the local institutional ethical committee. The data was analyzed by using a z-test of proportions.
Ethical Committee
Local institutional ethical committee clearance (HIMSR) was sought and exempted from the ethical clearance as it was an observational study only.
Results
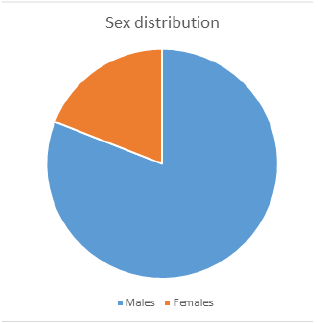
Most of the cases were males above 40 years of age with a male: female ratio of 4.25:1 (Figure 1). The most common site of origin was the oral tongue (40%), followed by buccal mucosa (19.04%), and the least common was laryngeal carcinomas (4.76%) (Table 1). The total number of new head and neck cancer cases visiting our facility during a pandemic and pre-pandemic times were similar with no major difference (63 vs. 65). Moreover, the average number of HNC patients presenting to our facility per 3 months period during a pandemic and pre-pandemic times was also equal (13.5 vs. 13.92). However, during the lockdown, these numbers dropped to less than half (6 per 3 months). There was quite an expected increased influx of HNC cases post lockdown relaxation which rose to three times more (18 per 3 months) than lockdown period (Table 2). Most of the patients presented with advanced stages (III/IV) of disease during both pandemics as well as pre-pandemic times with no significant difference observed (68.25% vs. 60%). However higher incidence of unresectable/inoperable( IVb) advanced cases was seen during pandemic months (30%) compared to pre-pandemic months (7.6%) and these findings were statistically significant (p-value of 0.011) as shown in Table 3 and Figure 2. Two third (n=8/12) among these advanced inoperable (IVb) cases during pandemic times had a delay of more than 3 months and one-third (4/12) had a delay of more than 6 months in seeking medical advice. Moreover, there was no delay in diagnosing the cases after their first contact with our health care facility as all cases were diagnosed histopathologically within the first 2 weeks times.
| Site of tumors | Number (n) | Percentage % |
|---|---|---|
| Oral tongue | 25 | 39.68 |
| Buccal mucosa | 12 | 19.04 |
| Gingivobuccal sulcus | 6 | 9.5 |
| Sinonasal | 7 | 11.11 |
| Oropharyngeal | 6 | 9.5 |
| Hypopharyngeal | 4 | 6.35 |
| Laryngeal | 3 | 4.76 |
| Total | 63 | 100% |
| Three monthly period | Number of cases | ||
|---|---|---|---|
| March-May 2020 | 1st lockdown | 6 | 3 times less |
| June-August 2020 | Post lockdown | 18 | |
| Sept-November 2020 | Post lockdown | 18 | |
| Dec 2020-Feb 2021 | Post lockdown | 15 | |
| March-May 2021 | 2nd lockdown | 6 | 3 times less |
| Total | 63 |
| Clinical stage | Pre pandemic period (n=65) | pandemic period(63) | ||||
|---|---|---|---|---|---|---|
| Without lockdown (n=51) | Lockdown (n=12) | |||||
| Early tumors (I,II) | 27 | 18 | 2 | 20 | ||
| Advanced operable (III,IVa) | 36 | 39 | 27 | 4 | 31 | 43 |
| Advanced inoperable (IVb) | 3 | 6 | 6 | 12 | ||
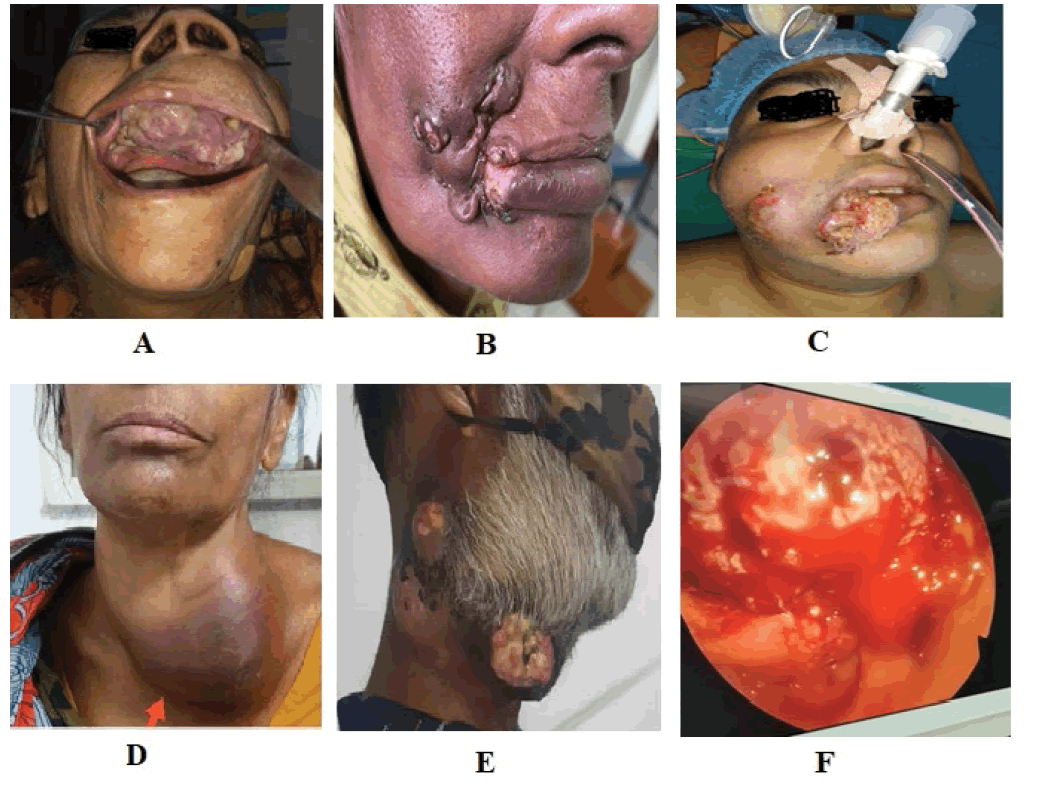
Figure 2. Advanced inoperable cases across many sites of H&N; A): Advanced scc palate involving pteygoids and skull base; B): Advanced buccal mucosa scc with extensive skin involvement; C): Advanced buccal mucosa scc with extensive skin and lip involvement; D): Hypopharyngeal ca with extension into thyroid gland and encasement of carotids; E): Lower GIngivobuccal scc with erosion of mandible and fungation of eternal skin; F): Endoscopic picture of scc tongue involving almost complete oral tongue and base of tongue
Discussion
The current study observed that there was a sharp decline in HNC patient visits to our health care facility during lockdown months of the pandemic as opposed to months without lockdown. The reduction seen was less than half (6 per 3 months) of the average number of new HNC patient visits (13.5 per 3 months). However, there was no significant reduction in the number of new cases (n=63) diagnosed overall during the 14 months of the pandemic, i.e. between March 2020-May 2021 when compared with pre-pandemic numbers (n=65) for the same period. Lockdowns cause a delay in people reaching healthcare facilities, which causes a dip in the number of patients coming to the hospital during lockdown months. When the lockdown restrictions are eased, they come to the hospital with tumors that are now in their advanced stages. This delay of even 2 to 3 weeks is sufficient to make HNCS inoperable, thus increasing both morbidity and mortality. This is in line with existing literature. It is well established that during the COVID-19 pandemic, patients experienced a delay in the diagnosis of their cancer. For example in Germany, as studied by Jacob, et al., national screening programs were suspended for a few types of tumors which inevitably caused a poorer outcome in the patients affected by those cancers [11]. A study using data from the Dutch cancer registry showed a decrease of 26%-60% in the number of new cancer diagnoses in the period between April 6, 2020, and April 12, 2020 [12]. At the University of Texas MD Anderson cancer center, one of the largest cancer centers in the world, an analysis of epidemiological and demographic data observed a 46.7% drop in outpatient visits and 46.8% of surgeries performed from March 1, 2020, to April 9, 2020, compared to the same time interval in 2019 [13]. The implications of these observations are grave in India, where almost 60%-80% of patients present in the later stages of any disease, including HNCS, as compared with developed nations where only about 40% of cases are present in advanced stages [14].
We observed that the most common site of involvement was the oral tongue seen in 40% of cases. Oral cancer is the most common HNC seen in India, preferably found in men who consume smoked and smokeless tobacco and alcohol [15].
The current study noted an unfortunate higher trend of new cases with advanced inoperable/unresectable disease during pandemic months (30%, 12/43) compared to pre-pandemic months (7.6%, 3/39) with a p-value of 0.011. These findings were statistically significant although overall the total number of new HNC visits and diagnoses remained the same in both pre-pandemic and pandemic months (65 vs. 63). These results were corroborative with the findings published in the British medical journal in April 2020 done by Jacqui wise who predicted a 20% increase in cancer mortality could be seen due to the COVID-19 pandemic in the due course of time [9]. Their study estimated that at least 6270 additional deaths could occur in England over the next 12 months in patients with new cancer diagnoses which could rise to an estimated 17,915 additional deaths if all people who currently have cancer are considered. It has been seen that a reasonable outcome can be expected at a stage where resection is feasible, unlike advanced tumors where the prognosis is dismal even after surgery and appropriate adjuvant treatment [16]. With a doubling time of HNC being between 15-99 days, this consequently causes greater morbidity and mortality in these patients even in short lockdowns [8].
The current study observed that Two-third (8/12) of these advanced inoperable cases of pandemic times had a delay of more than 3 months and one-third (4/12) had more than 6 months delay in seeking medical advice. However, there was no delay in diagnosis as all cases were staged and diagnosed histopathologically within the first 2 weeks after first contact with our health care facility. This clearly shows that delay was mostly due to a delay in seeking medical help than arriving at the histopathological diagnosis after getting access to a health care facility. This has been validated by various authors who observed that 70% of cancer patients of any type in India could not access healthcare facilities during lockdown (Table 4) [17].
| Duration of symptoms | Number | Percentage |
|---|---|---|
| 3- 6 months | 8 | 66.6% |
| >6 months | 4 | 33.3% |
| Total | 12 | 100% |
However, these findings were not supported by the American cancer society, which conducted a survey of 1200 cancer patients and found that almost 79% of patients have had underactive treatment because of delay in initiation of chemotherapy, radiotherapy, and/or hormone therapy [8]. These differences can be justified by the fact that in developing countries like India Factors like financial burdens, ignorance towards allopathy, poverty and lack of knowledge, and poor access to health facilities dominate the scenario and further complicate delay in seeking medical help more than in diagnosis and subsequent treatment. All of these factors, when put together with a lockdown of most healthcare facilities for non-COVID patients, cause a dangerous shift in the trends of diagnosis and comprehensive management of HNC. Moreover, most patients with HNC are older adults who present with underlying comorbidities associated with higher morbidity and mortality [18].
This problem does not go unrecognized in various developed countries; different solutions have been proposed and implemented with success. In the United Kingdom, the NHS has created “cancer hubs,” where patients with cancer from multiple tumor groups are fast-tracked on a priority basis [10]. The American College of Surgeons has given guidelines for the triage of cancer surgeries during this pandemic and recommended the decision to be taken by the MDT team based on the available resources and situation in their region [19]. We propose that this problem is more severe in India, and with fewer implemented policies to cope with the delayed treatment for HNC patients. This measure aside, developed nations are leaps and bounds ahead in the overall management of HNC patients. There is undoubtedly massive scope for improvement in the timeline of treatment for the management of HNCS in developing nations. The guidelines proposed by the foundation of the HNC Organization of India are some of the steps taken in the right direction [20].
Conclusion
The author concludes that the COVID-19 pandemic has a drastic effect on the comprehensive management of head and neck cancers. Delay in seeking medical advice and thus diagnosis and initiation of treatment render a huge number of cases inoperable/unresectable. There is high scope for improvement besides imparting the knowledge of COVID transmission and Standard operating procedures to be followed, considering the cancers as semi emergent at the administration level with the provision of separate cancer hubs, provision of COVID sterile ambulances/means of transportation to and from the health facilities to gain the confidence of patients and reduce unnecessary scare, prompt imaging, and histopathological diagnosis can facilitate timely intervention and thus help in decreasing morbidity and mortality of HNC.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgment
Mr. Varun is a statistician from the department of community medicine.
References
- World Health Organization. "WHO Director-General’s opening remarks at the media briefing on COVID-19-11 March 2020." 2020.
Google Scholar - World Health Organization. "WHO Coronavirus (COVID-19) Dashboard."
- Guzzetta, Giorgio, et al. "Impact of a nationwide lockdown on SARS-CoV-2 transmissibility, Italy." Emerging Infectious Diseases, Vol. 27, No. 1, 2021, pp. 267-70.
Google Scholar Crossref - The Economics Times. "AIIMS to shut down OPD from March 24 till further notice." 2020.
- Mahl, Claudiane, et al. "Delay in head and neck cancer care during the COVID-19 pandemic and its impact on health outcomes." Brazilian Oral Research, Vol. 34, 2020.
Google Scholar Crossref - American Cancer Society. "COVID-19 Pandemic ongoing impact on cancer patients and survivors: Survey findings summary." 2020.
Google Scholar Crossref - Graboyes, Evan M., et al. "Association of treatment delays with survival for patients with head and neck cancer: A systematic review." JAMA Otolaryngology-Head & Neck Surgery, Vol. 145, No. 2, 2019, pp. 166-77.
Google Scholar Crossref - Lai, Alvina G., et al. "Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency." MedRxiv, 2020.
Google Scholar Crossref - Wise, Jacqui. "COVID-19: Cancer mortality could rise at least 20% because of pandemic, study finds." BMJ, 2020.
Google Scholar Crossref - England, N. H. S. "Cancer services in London during the COVID-19 pandemic." London, England: NHS, 2020.
Google Scholar Crossref - Jacob, Louis, et al. "Impact of the COVID-19 pandemic on cancer diagnoses in general and specialized practices in Germany." Cancers, Vol. 13, No. 3, 2021, p. 408.
Google Scholar Crossref - Dinmohamed, Avinash G., et al. "Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands." The Lancet Oncology, Vol. 21, No. 6, 2020, pp. 750-51.
Google Scholar Crossref - Kiong, Kimberley L., et al. "Changing practice patterns in head and neck oncologic surgery in the early COVID‐19 era." Head & Neck, Vol. 42, No. 6, 2020, pp. 1179-86.
Google Scholar Crossref - Kulkarni, Manik Rao. "Head and neck cancer burden in India." International Journal of Head & Neck Surgery, Vol. 4, No.1, 2013, pp. 29-35.
Google Scholar Crossref - Niaz, Kamal, et al. "Smokeless tobacco (paan and gutkha) consumption, prevalence, and contribution to oral cancer." Epidemiology and Health, Vol. 39, 2017.
Google Scholar Crossref - Hamoir, Marc, et al. "Salvage surgery in recurrent head and neck squamous cell carcinoma: Oncologic outcome and predictors of disease free survival." Oral Oncology, Vol. 67, 2017, pp. 1-9.
Google Scholar Crossref - Ghosh, A. "70% of India’s cancer patients couldn’t access care during lockdown, experts say." The Print, 2020.
- Martins-Filho, Paulo Ricardo, Carolina Santos Souza Tavares, and Victor Santana Santos. "Factors associated with mortality in patients with COVID-19. A quantitative evidence synthesis of clinical and laboratory data." European Journal of Internal Medicine, Vol. 76, 2020, pp. 97-99.
Google Scholar Crossref - COVID, ACS. "Guidelines for triage of cancer surgery patients." ACS, 2020.
Google Scholar Crossref - Foundation for Head and Neck Oncology. "Advisory for management of head and neck cancers during COVID-19 epidemic period." 2020.
Google Scholar