Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Knowledge, Attitude, and Behavior of Breastfeeding among Urban Women in Chennai-A Cross-Sectional Study
K Saravanan1, B Krishna Prasanth2*, S Hariharan2, P Deepika3 and Aishwarya PM22Department of Community Medicine, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India
3Department of Paediatrics, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India
B Krishna Prasanth, Department of Community Medicine, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email: mail2kristain@gmail.com
Received: 16-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021
Abstract
Background: Appropriate breastfeeding practices play a prominent role in reducing morbidity and mortality among children below 5 years of age. Exclusive breastfeeding is important for a child’s health and growth. However, there seems to be a disdain for breastfeeding practices among emergent countries. This study intends to assess the knowledge, attitude, and behavior towards breastfeeding among nursing mothers from Chennai. Methods: This was a cross-sectional study conducted among 200 mothers of children aged 0-1 year. The participants were selected through purposive sampling from postnatal OPD of government hospitals in Chennai. Breastfeeding practices were assessed using a self-administered questionnaire after getting informed consent. Results: Almost 52% of the mothers had fair knowledge and only a minimal (3%), had poor knowledge regarding breastfeeding practices. Most of the participants 173 (86.5%) believed that adequate feeding with breast milk played an important role in the long-term health of their children. Most of the mothers (77.5%) viewed breastfeeding as more convenient than formula feeding and around 73% of them felt that breastfeeding promoted bonding between the mother and their infants. Almost 72.5% of the study participants initiated breastfeeding as soon as they delivered. Only a minimal group of babies (7%) had received prelacteal feeds, the commonest being sugar water and honey. Almost 90.5% of newborns received colostrum as their first feed. Conclusion: This study inferred that there was only a fair knowledge about breastfeeding among the nursing mothers living in urban regions and also their attitude and behavior about breastfeeding were sub-optimal. This study also gives an insight into factors hindering optimal breastfeeding practices among young mothers. We must provide proper information, education, and communication to nursing mothers regarding proper breastfeeding. Henceforth this study identifies the need for public health education campaigns towards breastfeeding practices among nursing mothers living in emergent countries.
Keywords
Breastfeeding, Women, Knowledge
Introduction
Breastfeeding is indispensable in not only providing the young infant with the necessary nutrients they need for optimal growth and development but also promotes a direct bond between the mother and her infant [1]. Breastfeeding has numerous advantages for both the mother and the neonate. Exclusive breastfeeding is related to decreased morbidity and mortality among under 5 children. Exclusive Breastfeeding (EBF) is the choice of nutrition till 6 months, beyond which complementary foods are introduced along with breastfeeding. Ideally, breastfeeding is to be initiated within an hour after birth. WHO recommends feeding colostrum, the first milk which is rich in antibodies as an initial food for the neonate. Breast milk is easily digestible by the developing gastrointestinal system, in neonates than with formula feeds. Breast milk meets all the required nutrients necessary during the newborn period, especially in the initial six months.
National health family survey data reveals that Tamil Nadu is the state with the least compliance with exclusive breastfeeding compared to all other South Indian states. The survey also finds that only 41% of children in Tamil Nadu are breastfed in the first 30 minutes of life, which implies a lost opportunity to give colostrum for the newborn [2]. Children who were breastfed showed higher developmental scores as opposed to their peer groups who were formulafed. During episodes of diarrhoea, dehydration could be prevented if the child is breastfed. Malnutrition, a more prevalent condition could be eradicated among children if they are breastfed adequately. The secretory antibodies present in breast milk reduced the incidence of childhood illnesses such as diarrhoea and pneumonia, the most important causes of infant mortality [3]. Maternal benefits from breastfeeding are natural (though not fail-safe) methods of birth control. It reduced the incidence of breast and ovarian cancer. Beyond the immediate benefits, mothers who breastfed were less probably to be obese. With the promotion of timely breastfeeding, neonatal death accounting for 16% among the child can be reduced. Sustainable development goals 2 and 3 could be achieved if all children were breastfed since the first day and if breastfeeding commenced within the initial 60 minutes [4]. Hence this study was undertaken to assess the Knowledge, attitude, and behavior of breastfeeding among urban mothers from Chennai.
Materials and Methods
A descriptive cross-sectional study was conducted to assess the knowledge, attitude, and behaviour of breastfeeding among mothers attending government hospitals in Chennai. About 200 mothers who complied with the inclusion criteria, criteria included all nursing mothers aged more than 18 years and free from any mental illness, were enrolled in this study. The participants were selected using the purposive sampling technique. A questionnaire for assessing knowledge, attitude, and behavior of mothers on breastfeeding was prepared based on WHO and CDC guidelines. Iowa infant feeding attitude scale was used to assess the attitude variable questionnaire.
The questionnaire consisted of four parts which are as follows. Part I consisted of 20 questions with demographic details, obstetric details, and previous knowledge of breastfeeding. Part II comprised of 13 questions regarding the breastfeeding practices such as early initiation of breastfeeding, exclusive breastfeeding, use of pre and post-lacteal feeds, if colostrum was given, Bottle feeding practices, Rooming-in, and Skin to skin contact practices. Part III consisted of 15 questions, with questions on knowledge of breastfeeding, regarding colostrum, breastfeeding duration, mother’s comfort, bonding between mother and newborn, neonatal and maternal health, maternal hygiene, and beauty. Questions were formulated in true or false format. The score was interpreted as 76%-100% with good knowledge, 51%-75% as fair knowledge, ≤ 50% with poor knowledge.
For assessing the attitude towards breastfeeding, 17 questions were used. The responses were recorded as 0-Disagree,1- Neutral,2-Agree. These were interpreted as scores below 50% with a negative attitude towards breastfeeding and scored between 51%-100% as a positive attitude towards breastfeeding. After obtaining Institutional ethical clearance, this study was conducted in a major government hospital in Chennai, Tamil Nadu. Two hundred mothers of Infants attending pediatrics outpatient and inpatient were randomly selected. Data entry and data analysis were done with SPSS software. All the data were tabulated and analyzed. Demographic and obstetrical variables of mothers were analyzed in terms of frequency and percentage distribution.
Results
Table 1 represents the frequency and percentage distribution of demographic variables of mothers and their infants. Concerning the maternal age, 4 (2%) were below 19 years and 84 (42%) belonged to 20-25years. 84 (42%) were in 26-30 years and 28 (14%) were more than 31 years. Considering the educational status of mothers, 79 (39.5%) have completed up to middle school. 73 (36.5%) have completed their high school. 35 (17.5%) have completed the undergraduate and 10 (5%) were post-graduates. Regarding the occupation of the mothers 5 (2.5%) of them were government employees, 35 (17.5%) were private employees, 4 (2%) were doing business, 139 (69.5%) were housewives and 17(8.5%) were daily wages/coolie. The family income of 100 (50%) mothers was below 5000 INR, 57 (28.5%) was within the income group of 5001INR-10000 INR, 30 (15%) belonged to the income group of 10001 INR- 15000 INR, 10 (5%) was within the income group of 15001 INR-20000 INR, and 3 (1.5%) belonged to the income group of INR above Rs. 20000. Among the participants 141 (70.5%) were Hindus, 41 (20.5%) were Christians and 18 (9.0%) belonged to the Muslim community. In regards to family type, 131 (65.5%) were living in a nuclear family and 69 (34.5%) were living in a joint family. 103 (51.5%) were from the urban area, 97 (48.5%) were from a rural area. Among the 200 mothers, 105 (52.5%) had one child, 76 (38%) had two children, 19 (9.5%) were multiparous.
| Demographic variable | Group | Frequency | Percent |
|---|---|---|---|
| Age in years | ≤ 19 | 4 | 2 |
| 20-25 | 84 | 42 | |
| 26-30 | 84 | 42 | |
| ≥ 31 | 28 | 14 | |
| Education | Illiterate | 79 | 39.5 |
| Schooling | 73 | 36.5 | |
| Undergraduates | 35 | 17.5 | |
| Postgraduates | 10 | 5 | |
| Professional degree | 3 | 1.5 | |
| Employment status | Government | 5 | 2.5 |
| Private | 35 | 17.5 | |
| Business | 4 | 2 | |
| Homemaker | 139 | 69.5 | |
| Daily wages/coolie | 17 | 8.5 | |
| Income in rupees | Below 5000 | 100 | 50 |
| 5001-10000 | 57 | 28.5 | |
| 10001-15000 | 30 | 15 | |
| 15001-20000 | 10 | 5 | |
| Above 20000 | 3 | 1.5 | |
| Religion | Hindu | 141 | 70.5 |
| Christian | 41 | 20.5 | |
| Muslim | 18 | 9 | |
| Family type | Nuclear family | 131 | 65.5 |
| Joint family | 69 | 34.5 | |
| Place of living | Urban | 112 | 51.5 |
| Rural | 97 | 48.5 |
From Table 2, we can observe that 138 (69%) of infants were less than 6 months of age, 62 (31%) were more than 6 months of age. Among the children, 143 (71.5%) were males and the remaining were female babies. 105 (52.5%) mothers underwent normal vaginal delivery and 95 (47.5%) had undergone C-section. 171 (85.5%) mothers delivered at full-term, 29 (14.5%) were preterm delivery. 195 (97.5%) were singleton birth, 5 (2.5%) were twins. Around 17 (8.5%) were LBW (Low Birth Weight) with 44 (22%) weighing 2001-2500 grams, 77 (38.5%) weighing 2501-3000 grams and 62 (31%) above 3001 grams.
| Details of last delivery of participated mother | N=200 | % | |
|---|---|---|---|
| Age of the child | <6 month | 138 | 69.0 |
| >6 month | 62 | 31.0 | |
| Gender | Male | 143 | 71.5 |
| Female | 57 | 28.5 | |
| Type of delivery | Natural | 105 | 52.5 |
| Less | 95 | 47.5 | |
| Birth order | Single birth | 195 | 97.5 |
| Twins | 5 | 2.5 | |
| Gestational age at birth | Below 35 weeks | 29 | 14.5 |
| 35 to 38 weeks | 171 | 85.5 | |
| Birth weight | ≤ 2000 g | 17 | 8.5 |
| 2001-2500 g | 44 | 22.0 | |
| 2501-3000 g | 77 | 38.5 | |
| ≥ 3001g | 62 | 31.0 | |
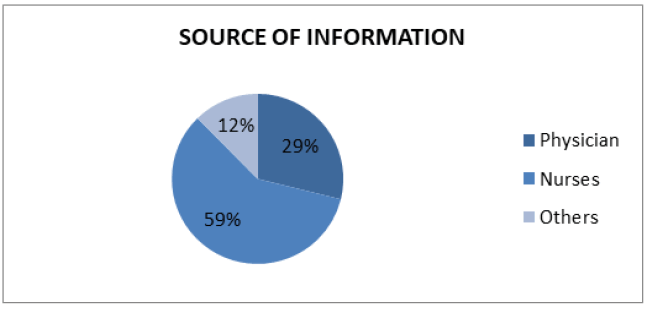
The majority of the participants got breastfeeding advice from the nurses (59%), followed by physicians (29%) and around 12% obtained by other sources (Figure 1).
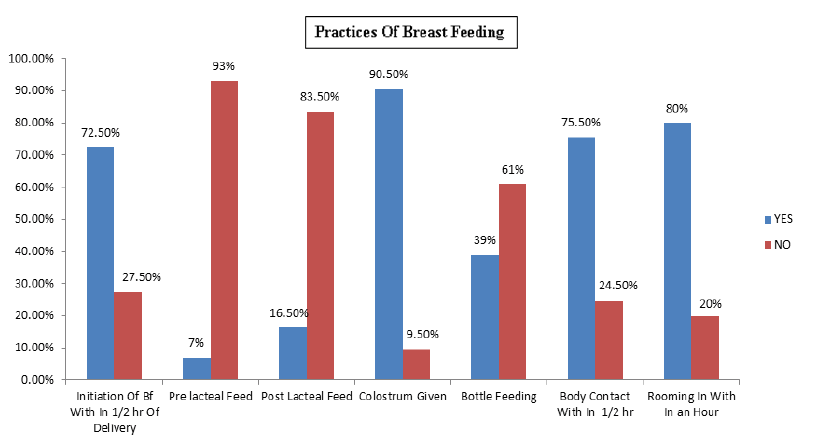
Figure 2 showed that around 145 (72.5%) mothers have initiated breastfeeding within half an hour of delivery. Among the newborns 14 (7%) of babies required postnatal admission. 7% of the neonates have received pre-lacteal feeds in the form of sugar water and honey. Only 181 (90.5%) of the babies have received the colostrum as their first feed. Around 19 (9.5%) were not fed with colostrum due to maternal hospitalization in other hospitals, the baby was kept nil per oral due to some medical conditions. The use of pre-lacteal feeds along with colostrum was found from this study. Bottle-feeding practices accounted for 78 (39.0%). 151 (75.5%) babies were roomed in with the mothers within 30 minutes of delivery, others 49 (24.5%) didn’t have skin-to-skin contact with the mother due to delayed post-op recovery, and the baby got admitted to NICU. Rooming-in was practiced in 160 (80%) of the babies within an hour of birth while in 40 (20%) rooming-in was not practiced as mother and child were separated due to admission of the neonate in NICU with some medical conditions like preterm birth, low birth weight, asphyxia, hyperbilirubinemia and maternal complications such as delayed post-op recovery, maternal admission.
Knowledge of Mothers Regarding Breastfeeding
In this study, 96.5% of mothers knew Colostrum being the initial milk and 194 (97%) mothers said colostrum is necessary for the baby’s immunity. Regarding breastfeeding practices 185 (92.5%) mothers consented to burp after each feed is necessary. Among the participants, 144 (72%) reported breastfeeding to be practiced till two years and 142 (71%) reported EBF for the initial six months. Around 168 (84%) of mothers replied that lactating mothers should take healthy food to improve milk secretion and 146 (73%) of mothers replied that during breastfeeding the mother should sit comfortably. 117 (58.5%) of the participants stated that eye contact to be maintained during breastfeeding. Most consented that breastfeeding helps in maternal and child bonding. Almost 64.5% of mothers were against the statement of stopping breastfeeding when they start weaning. 91 (45.5%) mothers knew as to breastfeeding reducing the risk of genital cancer. Among the participants, 70.5% of mothers had said to wash each breast with warm water before breastfeeding (Table 3).
| Knowledge Variable | True (n=200) | False (n=200) | Mean | SD | ||
|---|---|---|---|---|---|---|
| F | % | F | % | |||
| Colostrum is the first breast milk | 193 | 96.5 | 7 | 3.5 | 1.04 | 0.184241 |
| Colostrum is important for the baby to maintain immunity | 194 | 97 | 6 | 3 | 1.03 | 0.171015 |
| Burping should be done after each feed | 185 | 92.5 | 15 | 7.5 | 1.075 | 0.264052 |
| Breastfeeding should be continued up to two years | 144 | 72 | 56 | 28 | 1.28 | 0.450126 |
| Exclusive breast milk can be given during the first six months | 146 | 71 | 58 | 29 | 1.29 | 0.454901 |
| Lactating mother should take healthy food to improve secretion of milk | 168 | 84 | 32 | 16 | 1.16 | 0.367526 |
| During breastfeeding, the mother should sit comfortably | 146 | 73 | 54 | 27 | 1.27 | 0.445074 |
| During breastfeeding, the mother should maintain eye to eye contact and talk with the baby | 117 | 58.5 | 83 | 41.5 | 1.415 | 0.493958 |
| Wash each breast with warm water before breastfeeding | 141 | 70.5 | 59 | 29.5 | 1.415 | 0.493958 |
| Awakening the baby while breastfeeding | 121 | 60.5 | 79 | 39.5 | 1.295 | 0.457187 |
| Breastfeeding helps in mother and child bonding | 150 | 75 | 50 | 25 | 1.395 | 0.490077 |
| Breastfeeding prevents diseases affecting breast | 91 | 45.5 | 109 | 54.5 | 1.25 | 0.434099 |
| Breastfeeding affects the beauty of feeding mothers | 28 | 14 | 172 | 86 | 1.545 | 0.49922 |
| The mother would not feed the child when she has diarrhea | 90 | 45 | 110 | 55 | 1.86 | 0.347858 |
| Stop breastfeeding when you started weaning | 71 | 35.5 | 129 | 64.5 | 1.645 | 0.479714 |
Among the women 173 (86.5%) disagreed that the benefits of breastfeeding lasted only as long as the infant is breastfed. Nearly three-fourths of the mothers consented that breastfeeding is convenient rather than formula feeding. While 104 (52%) disagreed, 80 (40%) of them agreed to the statement “breast milk is lacking in iron”. Around 113 (56.5%) of the participants stated that “formula feeding is the better choice if the mother plans to go back to work”. Among the participants, 159 (79.5%) agreed that women who formula-fed miss the greatest joys of motherhood, and 109 (54.5%) of them agreed that fathers feel left out if a mother breastfeeds. 60.5% agreed women can breastfeed in public places such as restaurants. Almost all of them stated that breast milk is ideal for babies 166 (83%), easily digested 158 (79%), and healthy for an infant than formula 163 (81.5%). 147 (73.5%) agreed that breast milk is affordable than formula and 104 (52%) agreed that formula is as healthy as breast milk. Almost 96 (48%) felt that the mother who occasionally drinks alcohol should not breastfeed the baby. Overall the average score of the IIFAS (21.32 ± 4.57168, M ± SD) lay in the range of ‘Negative breastfeeding attitudes’ (Table 4).
| Attitude Score | Disagree | Neutral | Agree | Mean | SD | |||
|---|---|---|---|---|---|---|---|---|
| F | % | F | % | F | % | |||
| The benefits of breast milk last only as long as the baby is breastfed | 173 | 86.5 | 3 | 1.5 | 24 | 12.0 | 1.7450 | 0.65737 |
| Formula feeding is more convenient than breastfeeding | 168 | 84.0 | 2 | 1.0 | 30 | 15.0 | 0.3100 | 0.71867 |
| Breastfeeding increases mother infant bonding | 44 | 22.0 | 10 | 5.0 | 146 | 73.0 | 1.5100 | 0.83269 |
| Breast milk is lacking in iron | 104 | 52.0 | 16 | 8.0 | 80 | 40.0 | 1.1200 | 0.95402 |
| Formula-fed babies are more likely to be overfed than breastfed babies | 78 | 39.0 | 13 | 6.5 | 109 | 54.5 | 1.1550 | 0.95685 |
| Formula feeding is the better choice for the mother who plans to go back to work | 76 | 38.0 | 11 | 5.5 | 113 | 56.5 | 0.8150 | 0.95674 |
| Mother who formula feed miss one of the great joys of motherhood | 37 | 18.5 | 4 | 2.0 | 159 | 79.5 | 1.6100 | 0.78164 |
| Women should not breastfed in public places such as restaurants | 73 | 36.5 | 6 | 3.0 | 121 | 60.5 | 1.2400 | 0.95759 |
| Breastfed babies are healthier than formula fed babies | 31 | 15.5 | 6 | 3.0 | 163 | 81.5 | 1.6600 | 0.73286 |
| Breastfed babies are more likely to be overfed than formula-fed babies | 95 | 47.5 | 12 | 6.0 | 93 | 46.5 | 0.9900 | 0.97192 |
| Father feels left out if a mother breast feeds | 72 | 36.0 | 19 | 9.5 | 109 | 54.5 | 0.8150 | 0.93549 |
| Breast milk is the ideal food for babies | 26 | 13.0 | 8 | 4.0 | 166 | 83.0 | 1.7000 | 0.68729 |
| Breast milk is more easily digested than formula | 33 | 16.5 | 9 | 4.5 | 158 | 79.0 | 1.6250 | 0.75313 |
| Formula is as healthy as breast milk | 87 | 43.5 | 9 | 4.5 | 104 | 52. | 0.9150 | 0.97598 |
| Breast feeding is more convenient than formula | 36 | 18.0 | 9 | 4.5 | 155 | 77.5 | 1.5950 | 0.77717 |
| Breast milk is cheaper than formula | 45 | 22.5 | 8 | 4.0 | 147 | 73.5 | 1.5100 | 0.83870 |
| Mothers who drink occasionally should not breast feed | 96 | 48.0 | 8 | 4.0 | 96 | 48.0 | 1.0000 | 0.98225 |
| Mean Attitude Score | 21.32 | 4.57168 | ||||||
Most of the participants (52%) had fair knowledge, 45% of them had good knowledge, and very minimal (3%) had poor knowledge (Table 5).
| Knowledge score | Frequency | % |
|---|---|---|
| Poor (below 50%) | 7 | 3.5 |
| Fair (51%-75%) | 104 | 52 |
| Good (76%-100%) | 89 | 44.5 |
| Total | 200 | 100 |
From this study, it was found that 51% of the mothers had a neutral attitude and 47% were having a positive attitude (Table 6).
| Attitude score | Frequency (n=200) | Percentage |
|---|---|---|
| Negative attitude (17-27) | 3 | 1.5 |
| A neutral attitude (28-39) | 103 | 51.5 |
| Positive attitude (40 ≤ ) | 94 | 47.0 |
Nearly three fourth of the participants (74%) had desirable behavior scores (Table 7).
| Behaviour score | Frequency (n=200) | Percentage |
|---|---|---|
| Non-desirable (below 50%) | 52 | 26.0 |
| Desirable (above 50%) | 148 | 74.0 |
| Total | 200 | 100.0 |
Discussion
The first important step in breastfeeding is awareness and practice involved in breastfeeding. This study provides an insight into knowledge, attitude, and practices of breastfeeding in mothers hailing from an urban area, which could assist in intervention design and as a basis for more broad-based research in the other regions of the country. The Baby-Friendly Hospital Initiative (BFHI) was developed to encourage early initiation (i.e. within 30 minutes of delivery) of breastfeeding. Almost 72.5% of mothers initiated breastfed soon following birth in this study. This is comparatively greater than the study conducted by Vijayalakshmi, et al., in Karnataka, India [5]. The differences could be attributed to breastfeeding neonates kept nil per oral, preterm birth, cleft lip and cleft palate, birth asphyxia, maternal exhaustion, delayed post-op recovery after LSCS, mothers hospitalized are some of the reasons for delayed breastfeeding initiation. Approximately 27 percent of them initiated breastfeeding after 30 minutes and the explanation for late initiation was due to LSCS and neonatal morbidity such as birth asphyxia. To ensure optimal growth and development, proper nutrition is deemed necessary during infancy. Breastfeeding contributes to short-term and longterm benefits, including protecting children from various acute and chronic disorders. The specific nutritional and antibody properties and benefits of colostrum are now established [6]. From the study, 90.5% of mothers fed colostrum, which is higher in comparison with other studies conducted in India [7]. EBF particularly in countries like India is a healthy, simple, economical, and emotionally satisfying means of feeding babies. Current research reported that approximately 93% have followed exclusive breastfeeding while the remaining 7% have historically given are-lacteal feed as sugar water, honey, donkey milk, etc. EBF in this study was 93%, which is greater than available national data (72%), while pre-lacteal feed was 7%, comparatively lower than the national data (28%) [8]. From this study, 39% of mothers practiced bottle feeding. Similarly, Adil Ali Nassir Ayed said that because of work, 56.7% of mothers adopted bottle feeding [9]. The justification of bottle-feeding practices was due to inadequate breast milk, working nature, alternative feeding. 44.5% of mothers had strong awareness regarding breastfeeding. Around 97% of the participants knew about colostrum and its importance. In comparison, many studies found that 63.3% were informed of colostrum, and a study by Abroo Bashir, et al. showed almost identical results that 80% were informed of colostrum [10].
Among the mothers, 92.5% practiced infant burping, which is greater than the other studies which reported 70% being aware of infant burping. About 72% thought they could continue breastfeeding till the second year. This finding is almost similar to a study by Vijayalakshmi, et al., which found that 68% knew they should continue breastfeeding till two years of age [5]. Currently, the guidelines by WHO and UNICEF’s Global Policy for Infant and Young Child Feeding states that children should be breastfed exclusively during the initial six months. Compared to Vijayalakshmi, et al. study, in the present survey, 85.2% knew EBF, which is comparatively poor. This result suggests raising awareness towards exclusive breastfeeding [5]. Among the study participants, 45.5% of mothers understood that breastfeeding can prevent breast-affecting disease, which is more than the previous survey by Abroo Bashir, et al., which suggested that 17.6% of mothers recognized breastfeeding as preventing breast-affecting disease [10]. Abroo Bashir, et al. also suggested 75% were aware that breastfeeding improves mother-child bonding, which is low compared to 87.9% [10]. Most of the mothers were aware of breastfeeding practices. The mean attitude score in this study is 21.32 SD ± 4.57, which points towards a negative attitude towards breastfeeding. The subjects of this study had better knowledge about breastfeeding but the attitude was sub-optimal. This indicates that health educators should insist on breastfeeding and allow them to regularly apply their expertise to breastfeeding. Maternal variables and the medical condition of mothers causing a delayed initiation of feeding were post-op, maternal exhaustion, delayed post-op recovery after LSCS, admitted to other hospitals, delay in suturing episiotomy, and poor maternal feeding. Newborn variables such as warmer infants, phototherapy, incubated, sustained under intensive care/observation unit and medical conditions such as neonates sustained in NPO due to preterm birth, heart issue, cleft lip and cleft palate, birth asphyxia were confirmed by previous studies [9].
Conclusion
This study highlights the knowledge towards breastfeeding being fair among the urban population, but breastfeeding practices and attitudes were still sub-optimal. Few factors which were found from this study that could predict EBF includes the feeding experience and the employment of mothers. Insufficient breast milk was a major concern. Therefore, during their prenatal follow-up visits, healthcare providers should provide breastfeeding education to all women, especially women with low educational qualifications and no prior breastfeeding experience. Working towards resolving the barriers about breastfeeding, particularly for working mothers, alternatives must be provided including longer maternity leave and paid breaks for continued breastfeeding.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Organisation mondiale de la santé, et al. "Global strategy for infant and young child feeding." World Health Organization, 2003.
- Arnold, Fred, et al. "Nutrition in India. National Family Health Survey (NFHS-3), India, 2005-06." International Institute for Population Sciences, Vol. 43, 2009.
- Martin, Camilia R., Pei-Ra Ling, and George L. Blackburn. "Review of infant feeding: Key features of breast milk and infant formula." Nutrients, Vol. 8, No. 5, 2016, p. 279.
- Turin, Christie G., and Theresa J. Ochoa. "The role of maternal breast milk in preventing infantile diarrhea in the developing world." Current Tropical Medicine Reports, Vol. 1, No. 2, 2014, pp. 97-105.
- Vijayalakshmi, Poreddi, T. Susheela, and D. Mythili. "Knowledge, attitudes, and breast feeding practices of postnatal mothers: A cross sectional survey." International Journal of Health Sciences, Vol. 9, No. 4, 2015, pp. 364-75.
- Newburg, David S. "Innate immunity and human milk." The Journal of Nutrition, Vol. 135, No. 5, 2005, pp. 1308-12.
- Pandey, Deeksha, et al. "Awareness and attitude towards breastfeeding among two generations of Indian women: A comparative study." PloS One, Vol. 10, No. 5, 2015, p. e0126575.
- Victora, Cesar G., et al. "Infant feeding and deaths due to diarrhea: A case-control study." American Journal of Epidemiology, Vol. 129, No. 5, 1989, pp. 1032-41.
- Ayed, A. "Knowledge, attitude and practice regarding exclusive breastfeeding among mothers attending primary health care centers in Abha city." International Journal of Medical Science and Public Health, Vol. 3, No. 11, 2014, pp. 1355-63.
- Bashir, Abroo, Suhail Mansoor, and Mohammad Yousuf Naikoo. "Knowledge, attitude, and practices of postnatal mothers regarding breastfeeding: A cross-sectional study." International Journal of Medical Science and Public Health, Vol. 7, No. 9, 2018, pp. 725-30.