Case Report - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 7
Low Grade Serous Ovarian Carcinoma in an 18-Year-Old Girl: A Case Report
Derartu Fikre1, Wubshet Girma1, Fanta Assefa1, Abdo Kedir2, Tewodros Wubshet3* and Abel Tefera2Department of Pathology, Jimma University Medical Center, Ethiopia
3Assistant Professor of Pathology, Department of Pathology, Dire Dawa University, Dire Dawa, Ethiopia
Tewodros Wubshet, Assistant Professor of Pathology, Department of Pathology, Dire Dawa University, Dire Dawa, Ethiopia, Email: theddo04@gmail.com
Received: 22-Jun-2023, Manuscript No. ijmrhs-23-100709; Editor assigned: 24-Jun-2023, Pre QC No. ijmrhs-23-100709(PQ); Reviewed: 11-Jul-2023, QC No. ijmrhs-23-100709(Q); Revised: 16-Jul-2023, Manuscript No. ijmrhs-23-100709(R); Published: 28-Jul-2023
Abstract
Background: The rare epithelial ovarian cancer subtype known as Low-Grade Serous Carcinoma (LGSC) of the ovary has different clinical characteristics and a unique molecular profile. Compared to high-grade serous carcinoma, this tumor develops early, advances more slowly, and is associated with a longer survival period. Primary surgical cytoreduction to no discernible residual disease is a key prognostic factor. It is characterized by a very high level of chemotherapeutic resistance. Case Presentation: An 18-year-old nulligravida lady, presented with right flank pain of 4 days duration that worsened a day before her presentation. On examination, she had stable vital signs, mild tenderness in the right lower quadrant of the abdomen, but no guarding or rigidity. With an initial assessment of bilateral ovarian tumor + query perforated appendicitis assisted by imaging study; emergency laparotomy was done and biopsy was taken from both ovarian masses, and omentum and diagnosed as Low-grade serous carcinoma of both ovaries with secondary omental deposit. After she took four cycles of neoadjuvant chemotherapy, a relaparotomy was done to do surgical staging/ cytoreductive surgery, and she is currently on follow up. Conclusion: A rare histological subtype of epithelial ovarian cancer, Low-Grade Serous Carcinoma (LGSC) of the ovary, accounts for just 2%-5% of serous carcinomas. Even though the median age upon diagnosis is 46.9 years old, adolescents are still rarely affected. The mainstay of treatment is surgery, and as this cancer is not particularly sensitive to chemotherapy, it is strongly advised to perform a primary maximal cytoreduction.
Keywords
Ovarian cancer, Low-Grade serous carcinoma, Histopathology, Neoadjuvant chemotherapy
Introduction
In general, ovarian cancer is the most lethal gynaecologic malignancy [1]. The most typical histological subtype is Epithelial Ovarian Cancer (EOC), which accounts for the majority of cases. Based on histology, immunohistochemistry, and molecular profiling, EOCs can be divided into five main subgroups: High-Grade Serous Carcinomas (HGSC), endometrioid carcinomas, clear-cell carcinomas, mucinous carcinomas, and Low-Grade Serous Carcinomas (LGSC) [2]. The most frequent type of ovarian epithelial cancer is HGSC, but LGSC is uncommon. 5% to 10% of serous ovarian carcinomas and 2% to 5% of ovarian carcinomas, respectively, are LGSC [3].
It is now evident that high-grade and low-grade serous tumors are two distinct entities, notwithstanding the earlier belief that they were on a spectrum. They experience a variety of developmental stages, display a range of behaviors while obtaining therapeutic care, and eventually encounter a variety of outcomes [4].
Low-Grade Serous Ovarian Cancer (LGSOC) is a separate pathologic and clinical entity that presents at a younger age than High-Grade Serous Ovarian Cancer (HGSOC), with a median age at diagnosis of 46.9 years as opposed to 63 years for the latter [5]. Women as young as 19 and as old as 79 may be affected by the condition [6]. About 70% of LGSOC are detected at an advanced stage, similar to HGSOC (FIGO III–IV) [7].
LGSOC shares similarities with HGSOC in terms of clinical presentation, which also includes dyspnoea, urine urgency, abdominal and pelvic pain, bloating, and early satiety. In more severe situations, pleural effusion and/or intestinal obstruction may accompany it. CA-125 serum levels are helpful in the diagnosis and follow-up of LGSC, as they are with any other serous epithelial malignant ovarian tumor, despite the fact that HGSC tends to have greater CA-125 serum levels than LGSC [8].
Typically, the initial modality to characterize ovarian lesions is ultrasound. On ultrasonography, LGSC typically presents as a multilocular cystic lesion with more solid components than a Serous Borderline Tumor (SBT) and less solid components than an HGSC. In LGSCs, calcifications resembling psammoma bodies are frequent and can be seen on ultrasonography. The preferred imaging technique today for ovarian cancer staging and treatment monitoring is contrast-enhanced CT [8].
Histologically, LGSOC exhibits destructive invasion, a mitotic index of up to 12 mitoses per 10 High Power Fields (HPF), mild to moderate atypia without nuclear pleomorphism, and proliferation of cuboidal to low columnar cells [9]. LGSOC seems to have a better prognosis, with a mean 5-year survival for FIGO III–IV disease of 32.1% for HGSOC vs. 54.2% for LGSOC [10].
Even in advanced stage LGSOC, surgery is the mainstay of care, with the goal of total resection during initial cytoreductive surgery. After histological confirmation of the malignancy, neoadjuvant chemotherapy followed by interval debulking surgery may be considered if the tumor is inoperable or the patient has poor general health (including comorbidities, age, and nutritional status) [11,12].
Case Presentation
An 18-year-old nulligravida lady, who had a regular menses presented with right flank pain of 4 days that exacerbated a day back. She has a low-grade intermittent fever of one day’s duration.
On physical Examination, she is well looking with vital sign of BP-120/70 mmHg, PR-100/min, RR-20/min, Temp.- 36.8°C, weight: 70 kg, height: 150 cm, BMI: 31.1 kg/m2 , clear chest, full abdomen that moves with respiration with no sign of fluid collection. There is mild tenderness in the right lower quadrant on deep palpation but no guarding or rigidity. PR: A formed stool with no mass or blood. PV was deferred as her hymen is intact.
The Complete Blood Count (CBC) and organ function tests were within the normal range, as shown in a laboratory investigation. LDH 179 U/L, Beta HCG is 0.100 ml U/ml and CA125 U/ml to 1085 u/ml. Abdominopelvic U/S - there was an echo complex septated adnexal mass measuring 4 cm × 3 cm on the right side and another 6 cm × 5cm left sided adnexal mass with associated echo debris, free fluid collection in peri-appendiceal fossa in the right lower quadrant of the abdomen. Appendix not seen. With conclusion: bilateral ovarian mass.
Abdominopelvic CT reveals a bilateral ovarian mass (right measuring 6 cm × 5 cm and left 7 cm × 5 cm); predominantly solid with cystic components. Free fluid in the peritoneal cavity, mesenteric stranding in the left paraumbilical region, and an omental deposit. There were small perigastric lymph nodes, and the conclusion was a bilateral ovarian mass with malignant features, with ascites and an omental deposit.
Laparotomy was done with a finding of 600 ml of serous ascitic fluid, adhesion between omentum, descending colon, uterus, tubes and ovaries; right ovarian mass measuring 6 cm × 7 cm and left 5 cm × 4 cm ovarian mass, appendix looks normal; biopsy taken from both ovarian masses and omentum, and ascites sucked out.
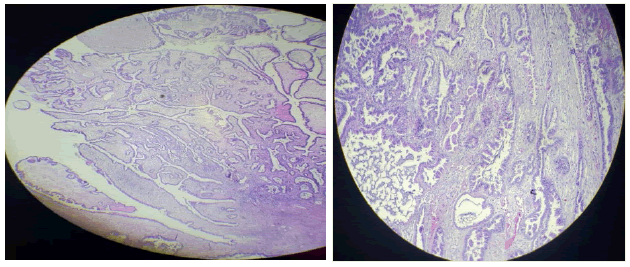
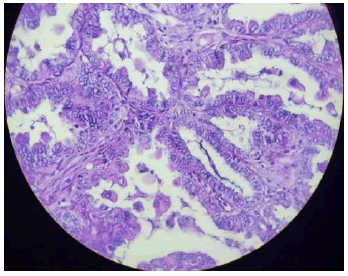
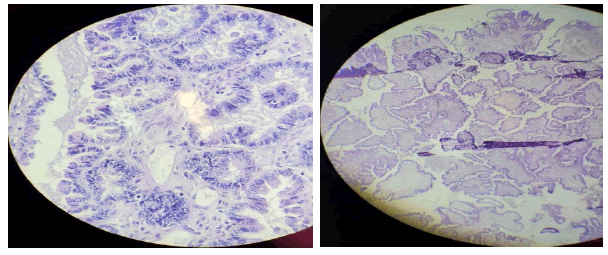
Histopathologic examination of sections from both ovarian masses shows tumoral tissue containing papillary structures with hierarchical branching and glandular structures, which are lined by stratified, mildly pleomorphic cells invading the underlying desmoplastic stroma. A section from the omentum shows similar malignant cell deposits. With this Pathologic diagnosis of Bilateral ovarian Low grade serous carcinoma with secondary omental deposits was made (Figures 1-3).
The patient was linked to the oncology side for Neo-Adjuvant Chemotherapy (NACT) and received carboplatin and paclitaxel. However, on the second cycle, she experienced an allergic reaction to paclitaxel (skin rash, itching, and fainting). The medication was then changed to cisplatin and cyclophosphamide, which she received for three cycles, resulting in a decrease in CA125 U/Ml to 447 U/Ml and after undergoing 4 cycles of chemotherapy, she was referred to a gynecologic oncology unit for interval debulking surgery
Intraoperative findings include a dense adhesion between the abdominal wall, the omentum, the uterus, and the bladder; a bilateral cystic ovarian mass measuring 10 cm × 12 cm; an implant measuring 4 cm × 5 cm on the omentum; 200 ml of ascites; and normal appearing liver and diaphragm. A total abdominal hysterectomy, bilateral salpingo-oophorectomy, and total omentectomy were performed.
Histologic examination of the bilateral salpingo-oophorectomy specimens showed hierarchically branching papillary architecture lined by stratified mild to moderately pleomorphic cuboidal cells having vesicular chromatin, conspicuous nucleoli, scant cytoplasm, and papillary structures with artifactual clefts infiltrating the stroma. The mitosis count was 12/HPF, and there was no necrosis and no histologic evidence of a chemotherapy response. Histologic examination of the omentum also showed similar malignant cells infiltrating the desmoplastic stroma.
With these morphologic features, a diagnosis of bilateral ovarian low-grade serous carcinoma with secondary omental deposits was made.
The patient is currently on follow up after being discharged from the ward with stable vital signs.
Discussion
This is a case of LGSOC in an adolescent who had no response to NACT. Low-Grade Serous Ovarian Cancer (LGSOC), which makes up 4.6% of serous ovarian cancers and 1.02% to 3.64% of all ovarian carcinomas, is a discrete pathologic and clinical entity, and is characterized by a younger age at presentation with a median age at presentation of 46.9 years, less aggressive biological behavior, lower sensitivity to chemotherapy, and longer Overall Survival (OS) compared with High-Grade Serous Ovarian Carcinoma (HGSOC). Histologically, LGSOC is characterized by a uniform/homogenous proliferation of small cells with mild to moderate atypia without nuclear pleomorphism (<3 variation in size), a mitotic index of up to 12 mitoses per 10 High Power Fields (HPF), and destructive invasion [9].
The signs and symptoms of LGSC are similar to those of other forms of ovarian tumors. The patient may not exhibit any symptoms or display severe ones, primarily as a result of the mass effect, such as early satiety, bloating, dyspnea, urinary urgency, and discomfort. A common LGSOC appearance is a solid, mixed solid and solid cystic, or cystic mass with nodularity and frequent calcification. Sometimes, peritoneal lesions which have calcified might be seen [10-12].
Primary debulking surgery is still the cornerstone of treatment for LGSC, as it is for all ovarian cancer subtypes, and retrospective studies that have just looked at LGSC have demonstrated that good debulking surgery is linked to better results. Although it is known that LGSC is more resistant to platinum-based chemotherapy, there is still insufficient data from prospective clinical trials to support a change in the standard of care. Staging affects the recommendation for primary chemotherapy that follows. All types of epithelial ovarian cancer, including serous carcinoma, are recommended to consider chemotherapy after surgery in stage 1C disease, while platinum-based chemotherapy is advised for stages II-IV disease after cytoreductive surgery. Although neoadjuvant chemotherapy is increasingly used in advanced ovarian cancer, it should be highlighted that LGSC has a considerable chemoresistance that works against its use in this subtype [13].
Conclusion
Low-Grade Serous Carcinoma (LGSC) of the ovary is uncommon histological subtype of epithelial ovarian carcinoma, which can be diagnosed as early as adolescence. Compared to high-grade serous ovarian cancer, LowGrade Serous Ovarian Carcinoma (LGSOC) is less aggressive and has a better clinical prognosis than HGSOC. Surgery is the mainstay of therapy, and since this cancer is not particularly sensitive to chemotherapy, it is strongly recommended to perform a primary maximal cytoreduction
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Ethics Approval
The patient provided written informed consent, which we obtained before publishing this study anonymously. This required no further review by the Institutional Review Board (IRB) of Jimma University.
References
- Siegel, Rebecca L., et al. "Cancer statistics, 2021." CA: A Cancer Journal for Clinicians, Vol. 71, No. 1, 2021, pp. 7-33.
Google Scholar Crossref - WHO Classification of Tumors Editorial Board. "Female Genital Tumors: WHO Classification of Tumors." IARC, Vol. 4, 2020.
- Matsuo, Koji, et al. "Trends of low-grade serous ovarian carcinoma in the United States." Journal of gynecologic oncology, Vol. 29, No. 1, 2018.
Google Scholar Crossref - Babaier, Abdulaziz, et al. "Low-grade serous carcinoma of the ovary: The current status." Diagnostics, Vol. 12, No. 2, 2022, p. 458.
Google Scholar Crossref - Gershenson, David M., Charlotte C. Sun, and Kwong-Kwok Wong. "Impact of mutational status on survival in low-grade serous carcinoma of the ovary or peritoneum." British journal of cancer, Vol. 113, No. 9, 2015, pp. 1254-8.
Google Scholar Crossref - Okoye, Ekene, Elizabeth D. Euscher, and Anais Malpica. "Ovarian low-grade serous carcinoma." The American journal of surgical pathology, Vol. 40, No. 5, 2016, pp. 627-35.
Google Scholar Crossref - Gershenson, David M., et al. "Impact of age and primary disease site on outcome in women with low-grade serous carcinoma of the ovary or peritoneum: results of a large single-institution registry of a rare tumor." Journal of Clinical Oncology, Vol. 33, No. 24, 2015, p. 2675.
Google Scholar Crossref - Amante, Sofia, Filipa Santos, and Teresa Margarida Cunha. "Low-grade serous epithelial ovarian cancer: a comprehensive review and update for radiologists." Insights into Imaging, Vol. 12, No. 1, 2021, pp. 1-12.
Google Scholar Crossref - Gadducci, Angiolo, and Stefania Cosio. "Therapeutic approach to low-grade serous ovarian carcinoma: state of art and perspectives of clinical research." Cancers, Vol. 12, No. 5, 2020, p. 1336.
Google Scholar Crossref - Peres, Lauren C., et al. "Invasive epithelial ovarian cancer survival by histotype and disease stage." JNCI: Journal of the National Cancer Institute, Vol. 111, No. 1, 2019, pp. 60-8.
Google Scholar Crossref - Widschwendter, Peter, et al. "CT scan in the prediction of lymph node involvement in ovarian cancer–a retrospective analysis of a tertiary gyneco-oncological unit." Geburtshilfe und Frauenheilkunde, Vol. 80, No. 5, 2020, pp. 518-25.
Google Scholar Crossref - Minig, Lucas, et al. "Patterns of lymph node metastases in apparent stage I low-grade epithelial ovarian cancer: a multicenter study." Annals of surgical oncology, Vol. 24, 2017, pp. 2720-26.
Google Scholar Crossref - Moujaber, Tania, et al. "New therapeutic opportunities for women with low-grade serous ovarian cancer." Endocrine-Related Cancer, Vol. 29, No. 1, 2022, pp. 1-16.
Google Scholar