Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Metoclopramide Induced Akathisia Treated with Propranolol: Case Report and Literature Review
Rami G Ahmad1,2*, Amirah S Algethami2,3, Faisal F AlArabi1,2 and Tamim A Alghamdi42King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
3College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
4Psychiatry Section, Eradah Complex and Mental Health, Ministry of Health, General Directorate of Health Affairs in Al-Baha, Saudi Arabia
Rami G Ahmad, Psychiatry Section, Medicine Department, Ministry of National Guard-Health Affairs, Jeddah, Saudi Arabia, Email: Ramihafiz@gmail.com
Received: 18-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021
Abstract
Metoclopramide is a common medication used to treat nausea, vomiting, and other conditions. Akathisia is a condition in which a person loses the ability to sit still and is considered part of extrapyramidal side effects. In this case report, we present a case admitted for an elective procedure, which then developed akathisia successfully treated with propranolol after the failure with a benzodiazepine. We share clinical thinking from the patient developing this sudden side effect until the patient was treated successfully. A literature review found 49 cases described before for the side effect, and no cases were found that were treated with propranolol.
Keywords
Metoclopramide, Akathesia, Propranolol, Benzodiazepine, Extrapyramidal symptoms
Introduction
Metoclopramide is a dopamine 2 receptor antagonist commonly used to manage nausea, vomiting, and vascular headaches. It treats gastroesophageal reflux disease and is considered prophylaxis for nausea and vomiting associated with surgical procedures or chemotherapy. It works by blocking dopamine at the D2 and serotonin (5-HT3 receptors) in the chemoreceptor trigger zone of the central nervous system. Its inhibitory actions have prokinetic effects on presynaptic and postsynaptic D2 receptors, agonism of serotonin 5-HT4 receptors, and antagonism of muscarinic receptor inhibition. All of this results in acetylcholine release, which increases lower esophageal sphincter and gastric tone, accelerates gastric emptying and transit through the gut, and relaxes the gastrointestinal tract. Possible side effects include drowsiness, dizziness, diarrhea, tiredness, and other mild side effects. Severe side effects include depression and suicidality, difficulty in breathing, and swallowing [1].
Akathisia (Greek a=without, Kathisia=setting) is a neuropsychiatric diagnostic illness identified by an incapacity to sit still. With this disorder, patients feel uncomfortable and distressed, with the legs mainly affected. The act will extremely urge patients to move. Akathisia is primarily an adverse effect of psychotropic medications such as antipsychotics, particularly first-generation SSRIs (Selective Serotonin Reuptake Inhibitors), but also associated with calcium channel blockers and antiemetics of the phenothiazine class. Although the pathophysiology of akathisia is poorly understood; however, some theories have been proposed. Among these, the most common one is an imbalance between several neurotransmitter systems, including noradrenergic, serotonergic, and dopaminergic pathways. Another theory suggested that increased stimulation of the locus coeruleus leads to an imbalance between the nucleus core and shell accumbency. A pattern of abdominal D2/D3 receptor use has been linked to the pathogenesis of akathisia [2].
In the literature, multiple cases have been reported since 1970. Most of these cases have only reported the development of tardive dyskinesia in chronic use of metoclopramide. Fewer cases accompanied by the use of acute metoclopramide with akathisia have been presented. It is important to recognize acute akathisia as a potential side effect of metoclopramide, especially in a busy setting like the emergency department. It is readily reversible if promptly treated. This research could not identify a case that developed akathisia from less than 10 mg of metoclopramide from the literature review. We could not find cases that were treated with propranolol. We highlight a case of acute akathisia secondary to administering a single low dose bolus of Intravenous (IV) metoclopramide postoperatively, which was difficult to identify immediately and treated successfully with propranolol after the failure of benzodiazepine. A summary of the literature review is then provided, reflecting the incident.
Case Presentation
Mrs. A, a 29-year-old, married, unemployed female who has a bachelor’s degree in religion, had been admitted to our hospital, King Abdulaziz Medical City. Her admission was under the Otorhinolaryngology (ENT) team through the Emergency Department, as a case of wound dehiscence postoperative from surgery two weeks before the presentation. The procedure that was executed was tympanoplasty. Seven days into Mrs. A’s admission, the ENT team made an urgent consultation with the psychiatry team regarding the patient’s sudden severe anxiety development in the form of a sudden panic attack. Upon initial assessment, the patient was out of her bed, pacing back and forth, restless and panting heavily. She could not sit down, reporting being unable to sit down. Mrs. A was in severe distress and kept asking for help. Mrs. A reported being excessively worried about the sudden change in her state; she could not calm herself down. Her worries were associated with the sensation of shortness of breath and nausea. All these worries were extremely sudden, starting about 2 hours before the psychiatry assessment, and Mrs. A reported she was doing well before her sudden change.
There was no fear of death, fear of losing control, sweating, numbness, chest pain or discomfort, and tremor. She reported having a similar attack one month ago, but it was associated with shortness of breath, palpitations, numbness, and fear of paralysis. The patient did admit, however, that the current episode was much more severe. Due to her current anxiety, Mrs. A could not give any specific details about these attacks. No anticipatory anxiety nor avoidance behaviors were reported. She performed well on recall, and registration was oriented and denied having any psychotic or manic symptoms. No symptoms were suggestive of delirium either, and she denied any suicidal ideation. Physical examination and laboratory findings were unremarkable. Her mental state examination revealed a young female, fair groom, and hygiene that had significant restlessness, rocking back and forth, unable to sit down. Her speech was coherent and relevant, and her mood was euthymic with an anxious affect. Her thought process was linear, with no abnormal perception, and her cognition was intact. Upon further history, no significant past psychiatric history was elicited, no history of substance use. There was a second-degree family psychiatric history of psychotic and mood disorders. The patient had no family history of anxiety disorder or obsessive-compulsive disorders, or chronic medical illnesses either.
Collateral history from her brother at this time confirmed the above history with no other complaints. Although her anxiety symptoms were not typical of anxiety disorders, our initial impression was a panic attack. She was given an initial immediate dose of benzodiazepine, lorazepam, 1 mg orally. We supplemented this with two additional doses, lorazepam, 1 mg to be given at bedtime, and 0.5 mg in the morning, and we decided to re-evaluate the patient the next day. Upon re-assessment the next day, her picture was more or less the same, with minimal response to the benzodiazepine doses. She was still restless and agitated and was unable to sit down or rest without feeling uneasy. The main benefit of benzodiazepine, according to Mrs. A, was sleeping as it did not affect her restlessness. For this reason, she did not take her morning dose of lorazepam. Upon further investigation and extensively reviewing the patient chart, we noticed that the patient started using antiemetic metoclopramide 5 mg IV for nausea and vomiting. She was given one dose before the consultation of our service. When the patient was asked about drug allergies or severe adverse effects, she recalled similar symptoms after taking medication for her nausea. The patient previously denied having any allergies to the physicians’ team. Mrs. A denied dystonia or muscle tension and no muscle pain.
It was concluded that her current picture was most likely an extrapyramidal symptom (akathisia) induced by metoclopramide. She has been given an oral propranolol 20 mg immediately and is to be reassessed within two hours. Upon returning to reassess the patient, her state had changed dramatically. She was no longer pacing. Her restlessness resolved almost completely. She was able to calm down and sit. Mrs. A reported being in her usual self again and started asking when she would be discharged home as there were no remaining symptoms. She was then deemed fit for discharge by the primary team. We informed the patient that it was likely she suffered an acute reaction to metoclopramide. We started her on propranolol 10 mg orally as needed up to twice daily for a short period, and she was given a follow-up appointment in our outpatient clinics one week after discharge. Mrs. A attended the clinic alone after discharge from the hospital without any significant psychiatric complaints. She reported she was doing extremely well with no anxiety symptoms and no recurrence of restlessness. She denied any anticipatory anxiety or any avoidance behaviors again. She did not take any propranolol after discharge as she did not need it. She was given additional information about metoclopramide and its reaction. She was advised to report to her physician about this incident and avoid taking metoclopramide until her appointment with her primary physician.
Research Strategy
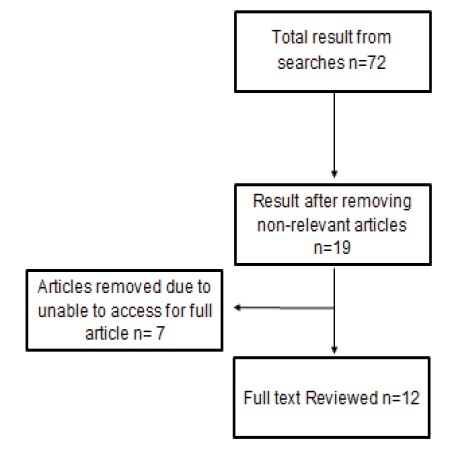
To attain the research resources in PubMed. The derived relevant articles were from March 2020. The terms used were: ((Extrapyramidal Symptoms (MeSH Terms)) OR (Akathisia (MeSH Terms)) AND (hydrochloride, metoclopramide (MeSH Terms)). The search resulted in 72 studies, and all were reviewed. Fifty-three articles were not relevant from the title. Seven articles were excluded due to the inability to access the full article. And only 12 were used (Figure 1). The number of cases that were reported in the literature was 49. The average dosage of metoclopramide was mostly 10 mg with different frequencies that ranged from BID to QID. The route of administration included oral, IV (bolus and infusion), and suppositories. One study concluded no difference if the medication is administered as IV bolus or infusion [3]. Symptoms of akathisia lasted from 36 hours to several months. These symptoms were treated by stopping metoclopramide. Symptoms were markedly improved after administering diphenhydramine hydrochloride and benzodiazepines. Five patients received benzodiazepines only, one patient received diphenhydramine hydrochloride alone, and only one patient received both benzodiazepine and diphenhydramine hydrochloride, as shown in (Table 1).
| Study Title | Authors | Publication Year | Study design | Number of Cases | Dose of Metoclopramide/Route | Duration of Akathisia | Medication Used for Treatment |
|---|---|---|---|---|---|---|---|
| Administration of metoclopramide by infusion or bolus does not affect the incidence of drug-induced akathisia [3] | Egerton-Warburton D, Povey K | 2013 | Clinical trial | 26 of 205 | 20 mg IV | N/A | N/A |
| Case of acute akathisia from intravenous metoclopramide [1] | Qiu LM, Lim BL | 2011 | Case report | 1 | 10 mg IV | 1 day | Diphenhydramine 25 mg IV and Midazolam 2 mg IV |
| Severe akathisia as a side effect of metoclopramide [2] | Van Gool AR, Doorduijn JK, Seynaeve C | 2010 | Case report | 1 | 20 mg Suppositories BID | 4 days | Haloperidol 1 mg and Temazepam |
| Akathisia, panic, agoraphobia, and major depression following brief exposure to metoclopramide [4] | Anfinson TJ | 2002 | Case report | 1 | N/A | Several months | N/A |
| Metoclopramide and akathisia [5] | Shuster J | 1998 | Case report | 1 | 10 mg PO, QID | N/A | N/A |
| Metoclopramide-induced extrapyramidal symptoms in a diabetic patient [6] | Robinson D, Omar SJ, Dangel C, Fenn H, Tinklenberg J. | 1994 | Case report | 1 | 10 mg PO, BID | 6 weeks | N/A |
| Antiemetic-induced akathisia in cancer patients receiving chemotherapy [7] | Fleishman SB, Lavin MR, Sattler M, Szarka H | 1994 | Cross-sectional study | 4 of 24 | N/A | N/A | N/A |
| The prevalence of metoclopramide-induced tardive dyskinesia and acute extrapyramidal movement disorders [8] | Ganzini L, Casey DE, Hoffman WF, McCall AL | 1993 | Cross-sectional study | 31 of 51 | 20 mg OD | N/A | N/A |
| Extrapyramidal side effects of antiemetics presenting as psychiatric illness [9] | Rodgers C | 1992 | Case reports | 3 | 1-10 mg IV | 1- 5 days | 1-Diphenhydramine hydrochloride 50 mg I.M |
| 2-75 mg IV before chemotherapy QID | 3- 6 days | 2-Lorazepam 0.5 mg QID | |||||
| 3-10 mg PO | 3-Two doses of lorazepam 0.5 mg PO and alprazolam 0.25 mg QID | ||||||
| Metoclopramide-induced akathisia [10] | Hamilton FA | 1987 | Case report | 1 | 10 mg TID | 6 weeks | Benzodiazepine |
| Tardive akathisia and agitated depression during metoclopramide therapy [11] | Shearer RM, Bownes IT, Curran P | 1984 | Case report | 2 | 1-10 mg PO, QID | 1-18 months | Oxazepam 15 mg TID and Misnderin 60 mg |
| 2-10 mg PO, TID | 2-2 years | ||||||
| Acute akathisia after oral droperidol and metoclopramide preoperative medication [12] | Barnes TR, Braude WM, Hill DJ | 1982 | Cross-sectional | 3 | 10 mg | N/A | N/A |
| N/A: Not available | |||||||
Literature Review
In 2011, Qiu and Lim reported the case of a 26-year-old woman who was presented with a history of five-day colicky abdominal pain accompanied by diarrhea and vomiting. The patient did not have any significant medical diseases. She was given an IV bolus of metoclopramide 10 mg and tramadol 50 mg to relieve her symptoms. Five minutes later, she became anxious, agitated, and restless. She complained of an uneasy sensation and chest tightness. Acute akathisia was suspected, and she has treated with IV bolus diphenhydramine 25 mg and investigated for all other possible causes. All results were normal. The patient’s symptoms did not improve, and she received a second dose of IV bolus diphenhydramine 25 mg, which led to slight changes in her symptoms. After 30 minutes, similar symptoms were noticeable. She was then administered an IV bolus of midazolam 2 mg leading to a slight improvement of her symptoms. She then received an IV infusion of diphenhydramine 50 mg over 2 hours, and her akathisia significantly improved with a complete resolution of her symptoms [1].
In 2010 Arthur, Jeanette, and Caroline reported a case of severe akathisia induced by metoclopramide. The 58-yearold woman had locally advanced breast cancer, which then spread to the liver and bones. Chemotherapy was initiated with 5-fluorouracil, methotrexate, and cyclophosphamide in combination with trastuzumab. After a diagnosis of the repetitive metastatic condition and before beginning chemotherapy, the patient was directed to a psycho-oncological service for extra psychological support. Her diagnosis was held overwhelming. She had used oxazepam and temazepam for a long time. She had been taken to the mental health facility 15 years ago for undefined issues. Four weeks before her hospitalization, she complained of vague uneasiness, which was attributed to hyperventilation. The weekend before her admission, she contacted G.P. and the oncology department. She complained of uneasiness and insomnia for days. The physical examination and laboratory tests were normal. She was then admitted to the cancer department. During the psychiatric visit, she walked up and down the oncology corridor, unable to sit on a chair, walking from one end of the room to the other. The patient dismissed having a history of anxiety disorders, and nothing was clear to the physicians. After reviewing her medication list, they discovered that she had been given numerous metoclopramide suppositories, 20 mg, to treat vomiting or nausea. The patient had started taking metoclopramide routinely 2 to 4 times a day in the weeks before hospitalization. She was informed that metoclopramide was the reason to develop her symptoms and advised to stop it. She was discharged and re-admitted on the same day due to anxiety and suicidal ideation. She was given temazepam and one dose of haloperidol, one mg. The akathisia subsided in 4 days and did not re-occur [2].
Egerton-Warburton and Povey conducted a prospective, double-blind, block randomized, placebo-controlled trial between 2007 and 2010. The research aimed at determining if a slow IV infusion of metoclopramide reduces the incidence of acute drug-induced akathisia compared to IV bolus. It was a multicenter trial across all three Southern Health emergency departments, including Monash Medical Centre, Dandenong, and Casey Hospitals in eastern metropolitan Melbourne, Australia. The study included patients over 19 years old, receiving metoclopramide 20 mg IV for any indication. Two hundred and six participants were randomized, and only two hundred and five were included in the analysis. The authors used the Prince Henry akathisia Rating Scale (PHARS) to assess drug-induced akathisia. Drug-induced akathisia occurred in 26 of 205 participants (12.7%, 95% CI: 8.1-17.3). It occurred in 11 out of 103 (10.7%, 95% CI: 4.6-16.7%) in those who received bolus, and in 15 out of 102 (14.7%, 95% CI: 7.7-21.7%) in the infusion group (p=0.7). The study concluded that there was no difference in the incidence of drug-induced akathisia between those receiving metoclopramide 20 mg as a bolus or an infusion [3].
In 2002, Anfinson reported a case of a patient who developed akathisia, panic, agoraphobia, and major depression after two days of using metoclopramide [4].
In 1998, Shuster reported a case of a 42-year-old male who had diabetes mellitus, gastroparesis. He was prescribed metoclopramide 5 mg QID, and then it was increased to 10 mg QID during the second week of treatment. After using the medication for two weeks, the patient developed motor restlessness and inability to sit still. He then was diagnosed with akathisia [5].
A study published in 1994 titled “Metoclopramide-Induced Extra Pyramidal Symptoms in A Diabetic Patient” reported a case of a 76-year-old male with a history of hypertension, diabetes mellitus type 2, and gastroesophageal reflux disease. He presented cases of restlessness, purposeless activity, abnormal gait, cogwheel rigidity, and bradykinesia. His symptoms developed after he began taking metoclopramide 10 mg BID. His symptoms were severe, and he became dependent on a wheelchair for 30 days before his admission. During his admission, metoclopramide was discontinued, and 36 hours later, he could gradually walk without assistance. Ten days after discharge, the patient had no motor symptoms and reported a feeling of inner calm, and he appeared less restless than before [6].
A cross-sectional study was conducted in 1994 titled “Antiemetic-Induced Akathisia in Cancer Patients Receiving Chemotherapy.” In the research, 24 consecutive cancer patients had a variety of cancer and had their first chemotherapy. These patients received metoclopramide or prochlorperazine to treat chemotherapy-related vomiting. Follow-up by telephone interviews was conducted within three days’ post-chemotherapy. The authors asked patients nine questions to assess akathisia, and patients who responded positively to 6 questions were considered to have akathisia. About 12 (50%) of 24 participants met the mentioned criteria. One patient used metoclopramide alone, eight patients used prochlorperazine alone, and three patients received both medications [7].
In 1993, Ganzini conducted a study to measure the prevalence and severity of Tardive Dyskinesia and Acute Extrapyramidal Movement syndromes. The study concluded that the high incidence and severity of drug-induced parkinsonism and the high severity of tardive dyskinesia and akathisia are associated with metoclopramide [8].
Rodgers documented three more cases in 1992; they developed akathisia and parkinsonism after receiving metoclopramide alone or in combination with prochlorperazine [9]. The first case was for a 34-year-old male with AIDS, admitted to the hospital due to fever. It was associated with blurred vision, weight loss, night sweats, nausea, and vomiting. Prochlorperazine 10 mg every 6 hours orally or intramuscular (IM) was among the list of medications he received. Four days later, a significant change in the patient’s mental status was noted. The patient had a vacuous look, a flattened affect, and tremulous lips and hands. A day later, the patient received 10 mg IV of metoclopramide for continued vomiting. Psychiatric history and examination revealed that the patient had severe parkinsonism, and both the medications were discontinued. He then received 2 doses of diphenhydramine hydrochloride 50 mg IM, and he recovered significantly during the next day. The second case was for a 70-year-old female with recurrent melanoma, admitted to receiving her chemotherapy. Her physician prescribed metoclopramide 75 mg IV before chemotherapy and every 6 hours to avoid nausea and vomiting. After two days, she became very anxious, and the psychiatric team was consulted. During the assessment, the patient had a masked face, bilateral cogwheeling, and involuntary leg movements. She was diagnosed with akathisia, and metoclopramide was stopped. The patient then received lorazepam 0.5 mg every 6 hours to manage her symptoms and was discharged after receiving chemotherapy without other side effects. Finally, the third case was for a 19-year-old female admitted for resection of a benign hepatic mass and lobectomy. Fifth day postoperative, the patient had vomiting and was given metoclopramide 10 mg orally. Despite giving her metoclopramide, she continued to have nausea and vomiting on the sixth day. Therefore, she was given prochlorperazine 10 mg IM. During the same day, the patient was anxious, shifting restlessly back and forth, and unable to stay in bed. The next day, though the patient did not report any nausea, she was surprisingly given another prochlorperazine dose. The patient had received two doses of lorazepam 0.5 mg orally but reported no relief of anxiety. She was diagnosed with severe akathisia. It was recommended to discontinue metoclopramide and prochlorperazine and placed the patient on alprazolam 0.25 mg four times a day. A day later, significant improvement was noted [9].
Hamilton presented another case in 1987 that involved a 42-year-old male who presented to an outpatient clinic due to his long-standing persistent chest discomfort and heartburn unresponsive to antacids. The doctor recommended keeping him on ranitidine and adding metoclopramide 10 mg TID. During the next four weeks, the patient noted a marked improvement. He noticed muscle twitches and restlessness of the lower extremities during exercise. The patient ignored these symptoms. The patient experienced agitation, restlessness, pacing, and concentration difficulties during the fifth and sixth weeks. He then sought emergency treatment for his symptoms and was admitted. He was treated with a benzodiazepine for agitation and tremulousness. Metoclopramide was discontinued. His symptoms quickly diminished after discontinuation of the metoclopramide. They were completely absent by the third day of admission [10].
Shearer, Bownes, and Curran, in 1984, reported two cases that developed tardive akathisia after using metoclopramide for four months [11]. The first case was a 47-year-old female who used oral metoclopramide 10 mg QID. This patient experienced a sudden panic attack and motor restlessness. Over the following two months, she complained of insomnia, becoming restless, and being very anxious about going out. After symptoms became more severe, metoclopramide was stopped. The symptoms did not improve. The patient was then prescribed oxazepam 15 mg TID, then switched to mianserin 30 mg. After that dose was increased to 60 mg, she improved slightly. Her improvement was short-term, and her symptoms returned in an episodic fashion. It was not until a further 18 months had elapsed that the symptoms eventually settled. The other reported case for a 50-year-old male patient, he used metoclopramide 10 mg TID. After using it for four months, he suddenly developed motor restlessness and reported an inability to sit still. He complained of rocking movements, panic attacks, insomnia, fear of the future, and loss of confidence in his ability to cope with his affairs. There was no improvement with intervention as psychotherapy, anxiolytics, or antidepressants. After ceasing metoclopramide for almost two years, symptoms fully subsided [11].
Barnes, in 1982 did a cross-sectional study in fourteen patients receiving oral droperidol 12 mg and metoclopramide 10 mg as preoperative medication for elective eye surgery [12]. Three out of the fourteen patients complained of a sudden restlessness feeling of inability to keep their legs still. These patients had no psychiatric history and had not used any psychiatric medications. The study concluded that using both droperidol and metoclopramide could develop akathisia in non-psychiatric patients within ninety minutes. It was hypothesized that akathisia is a dose-dependent side effect [12].
Discussion
In Mrs. A’s case, the sudden and acute presentation caused a shock for the patient, family, surgical team, and the psychiatry assessing team. During the patient’s initial presentation, many data were difficult to obtain due to the severity of the symptoms. The first decision was to decrease the anxiety symptoms in the patient, then to be reassessed again. Our first differential diagnosis of the patient did not include akathisia at all due to multiple reasons. First, this phenomenon’s rarity, as this diagnosis and the clinical picture was the first time seen in all team members assessing the patient. Second, physicians usually look for common causes and diagnoses to explain the patient’s presentation during practice. Hence we thought about the panic attack or delirium. Third, as the patient and family were in shock, many data were missing, making this diagnosis challenging to reach.
There was a remarkable similarity in the presentation of the case between akathisia and a panic attack. They both involve the patient having fear, being in an anxious state, and pacing. What helped us differentiate between akathisia and the panic attack was: 1) negative past psychiatry history in the patient, 2) negative family history of anxiety disorders, 3) lack of anticipatory worries, 4) lack of any provoking factors or emotional stressors before the episode, 5) history of a similar episode occurred during admission in other hospitals in the past after vomiting with no recurrence till the presentation mentioned above, and 6) the marked improvement after propranolol and the minimal response after lorazepam. Although the patient received a good dose of lorazepam when she was assessed the next morning, her akathisia symptoms remained despite no other metoclopramide doses being given. After 2 hours of propranolol 20 mg orally was given, the patient had improved dramatically to the point she asked for discharge.
Mrs. A reported poor response on lorazepam and a great response on propranolol. Apart from administering the doses and medication, this gave us a question: Is propranolol more superior in treating metoclopramide-induced akathisia than lorazepam? Or it was due to the chance that this observation was noticed. This question is an interesting area for research in the future. From the literature review, most cases did not receive propranolol and showed improvement in other treatments. The dose of metoclopramide administered to Mrs. A was 5 mg IV, which is lower than all case reports found in our review. This finding could generate a research question if metoclopramide-induced movement disorder side effects are not dose-dependent phenomena. We may estimate that metoclopramide-induced akathisia could be under-reported. We need more understanding of why some patients complain from dystonia more than akathisia, which increases the risk factors of such incidents and when to expect it, and our best treatment options for our patients.
Conclusion
In conclusion, this is a case of akathisia induced by using metoclopramide. It is crucial for physicians who prescribe metoclopramide to be aware of this side effect as it is usually used in an emergency or acute setting. We recommend asking the patient before giving any dopamine antagonist if the patient has a history of poor reaction, akathisia, dystonia, or any other drug-induced movement disorder. More studies help provide all physicians with insight into this phenomenon and fully understand the pathophysiology and the most effective medication to treat metoclopramideinduced akathisia.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Qiu, L. M., and B. L. Lim. "Case of acute akathisia from intravenous metoclopramide." Singapore Medical Journal, Vol. 52, No. 1, 2011, pp. 12-14.
- Van Gool, Arthur R., Jeanette K. Doorduijn, and Caroline Seynaeve. "Severe akathisia as a side effect of metoclopramide." Pharmacy World & Science, Vol. 32, No. 6, 2010, pp. 704-06.
- Egerton‐Warburton, Diana, and Kirsty Povey. "Administration of metoclopramide by infusion or bolus does not affect the incidence of drug‐induced akathisia." Emergency Medicine Australasia, Vol. 25, No. 3, 2013, pp. 207-12.
- Anfinson, Theodore J. "Akathisia, panic, agoraphobia, and major depression following brief exposure to metoclopramide." Psychopharmacology Bulletin, Vol. 36, No. 1, 2002, pp. 82-93.
- Shuster, J. "Metoclopramide and akathisia." Nursing, Vol. 28, No. 12, 1998, p. 74.
- Robinson, Dave, et al. "Metoclopramide-induced extra pyramidal symptoms in a diabetic patient." Journal of the American Geriatrics Society, Vol. 42, No. 12, 1994, pp. 1307-08.
- Fleishman, Stewart B., et al. "Antiemetic-induced akathisia in cancer patients receiving chemotherapy." The American Journal of Psychiatry, Vol. 151, No. 5, 1994, pp. 763-65.
- Ganzini, Linda, et al. "The prevalence of metoclopramide-induced tardive dyskinesia and acute extrapyramidal movement disorders." Archives of Internal Medicine, Vol. 153, No. 12, 1993, pp. 1469-75.
- Rodgers, Carla. "Extrapyramidal side effects of antiemetics presenting as psychiatric illness." General Hospital Psychiatry, Vol. 14, No. 3, 1992, pp. 192-95.
- Hamilton, Frank A. "Metoclopramide-induced akathisia." Military Medicine, Vol. 152, No. 11, 1987, pp. 585-86.
- Shearer, R. M., I. T. Bownes, and P. Curran. "Tardive akathisia and agitated depression during metoclopramide therapy." Acta Psychiatrica Scandinavica, Vol. 70, No. 5, 1984, pp. 428-31.
- Barnes, T. R. E., W. M. Braude, and D. J. Hill. "Acute akathisia after oral droperidol and metoclopramide preoperative medication." The Lancet, Vol. 320, No. 8288, 1982, pp. 48-49.