Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 4
Necrotizing Gingivitis as an Oral Manifestation of Hematopoietic Malignancies: A Case Report
Haslina Taib1*, Zurairah Berahim1, Mior Azrizal M Ibrahim2 and Nurul Wahida Mohd Hasan12Unit Pakar Periodontik, Klinik Pergigian Kangar, Kangar, Perlis, Malaysia
Haslina Taib, Unit of Periodontics, School of Dental Sciences, Universiti Sains Malaysia, Health Campus, Kubang Kerian, Kelantan, Malaysia, Tel: +60 9-767 3000, Email: haslinakk@usm.my
Received: 25-Mar-2021 Accepted Date: Apr 20, 2021 ; Published: 27-Apr-2021
Abstract
Pathological lesions in the oral cavity could be the initial signs of underlying systemic disorders such as hematopoietic diseases. The presence of dental plaque and calculus could be as local predisposing factors that may exacerbate the oral lesion. This current report presents a case of a 16-year-old boy with acute necrotizing gingivitis as a manifestation of myelodysplastic syndrome/myeloproliferative neoplasms. The lesion was painful, tends to reappear at different periodontal regions when the patient in the immune-compromised state which resulted in difficulty in eating and tooth brushing. The lesion was under-controlled after non-surgical periodontal therapy was advocated followed by close monitoring of oral hygiene care. The physician and dentist must be aware of the changes in the oral health status of patients suffering from these hematological disorders as optimum oral hygiene maintenance is deemed important to avoid the debilitating condition.
Keywords
Necrotizing periodontal disease, Myelodysplastic syndrome, Myeloproliferative neoplasms, Necrotizing gingivitis
Introduction
Hematopoietic malignancies are among the most common malignant disorder and the cause of death of cancer patients [1]. The oral manifestations of these malignant hematologic diseases such as Chronic Myeloid Leukemia (CML), and Acute Myeloid Leukemia (AML) have been reported to affect the soft and hard tissues of the oral cavity. The conditions usually result in impaired oral hygiene procedures thereby predispose to oral diseases such as periodontitis [2]. The manifestations include mucosal pallor, ulcerations, spontaneous bleeding, gingival hyperplasia, periodontal and alveolar bone destruction, as well as bony masses in the maxilla or mandible. Myelodysplastic Syndrome/ Myeloproliferative Neoplasms (MDS/MPN) overlap syndromes are among hematologic malignancies that were rarely reported in our hospital setting. We report here the unusual oral presentation of a patient diagnosed with MDS/MPN that consistently affects the gingival tissues in the form of a necrotizing gingivitis-like lesion.
Case Report
A 16-year-old boy was referred to the dental clinic by a medical officer for the management of an oral lesion. He was admitted to the medical ward for a few days due to prolong anemia and low-grade fever and was under investigation to rule out his medical problem. During the ward admission, he complains of acute, sharp pain arising from the gum of the upper anterior teeth region.
The patient claimed the pain and ulcer-like lesion was sudden in onset, but it was immediately relieved by taking a pain killer. He was also having difficulty biting using his front teeth due to mobility. He denied having a history of dental trauma and it was not associated with toothache. The swelling at the upper labial gingiva was also increasing in size gradually.
A few months back, he was diagnosed with symptomatic anemia hence was treated and under follow-up at the district clinic nearby. The patient does not have any history of allergy to any medications or food. He is a non-smoker and has no para-functional habits. On further questioning to his mother, all his siblings are fit and healthy. He received regular dental check-ups and treatment under the school dental service program. Informed written consent was obtained from the patient’s mother before treatment initiated and management was conducted following the standard of care complied with the ethical principle.
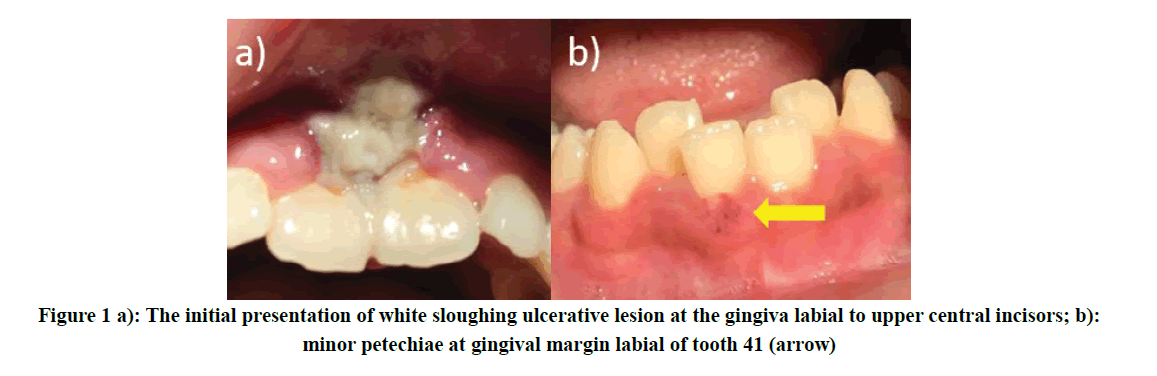
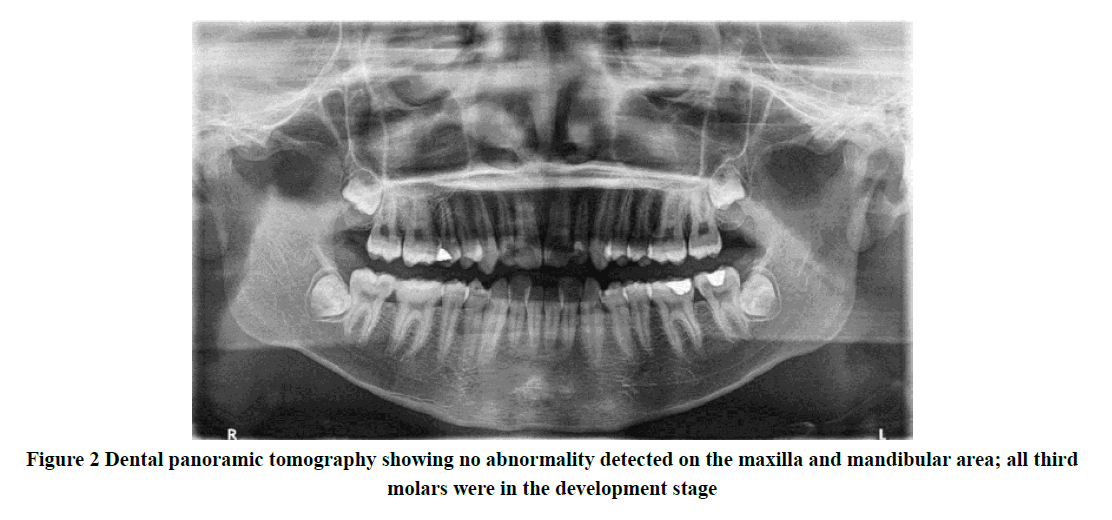
Extra-orally, the patient looks lethargic, pale with inadequate hydrational status. However, he appeared to be cooperative and motivated throughout the dental procedures. Upon intraoral examination, there was swelling and ulcerative lesion which was easily bleed on the labial gingiva of his upper central incisor teeth region associated with grade 1 tooth mobility. The lesion appeared sloughing with an erythematous and rounded border extending from the gingival margin towards the buccal sulcus affecting the maxillary labial frenum. Minor petechiae were also observed at the gingiva, labial to tooth 41 (Figure 1). He has unsatisfactory oral hygiene (plaque score was 57.1%) with localized sub-gingival calculus that is easily spotted. The gingival bleeding score was 81.3%, however, no periodontal pocket was detected which indicated generalized gingivitis [3]. Dental panoramic tomography was taken which revealed no abnormal findings of the maxilla and mandible (Figure 2). The diagnosis made at this stage was an acute necrotizing periodontal disease associated with a hematologic disorder
As the lesion was very painful alongside his unfavorable systemic condition, the full mouth examination and complete oral debridement were deferred. The area of lesion was gently irrigated with 0.2% Chlorhexidine (CHX) mouthwash and he was prescribed paracetamol 1 g 3 times a day for 5 days to relieve pain. Antibiotic therapy with augmentin and metronidazole had been initiated and completed for 1 week. He was advised to rinse with 0.2% CHX twice daily to help in improving his oral hygiene care.
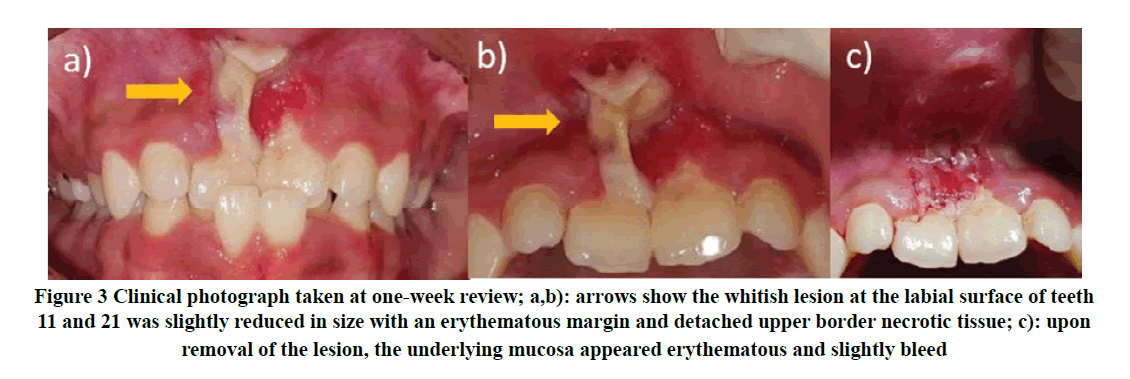
The patient was then scheduled for a 1-week review which showed a reduction of the pain intensity. The ulcerative lesion appeared slightly smaller in size however with persistent whitish necrotic tissue and sloughing (Figure 3). The petechia at the gingiva of tooth 41 had subsided. But he still appeared lethargic and pallor. Under local anesthesia, the necrotic tissue was gently removed with a curette exposing the erythematous mucosa. The area was then debrided with 0.2% CHX solution and hyaluronic acid gel (Gengigel®) was applied.
Figure 3. Clinical photograph taken at one-week review; a,b): arrows show the whitish lesion at the labial surface of teeth 11 and 21 was slightly reduced in size with an erythematous margin and detached upper border necrotic tissue; c): upon removal of the lesion, the underlying mucosa appeared erythematous and slightly bleed
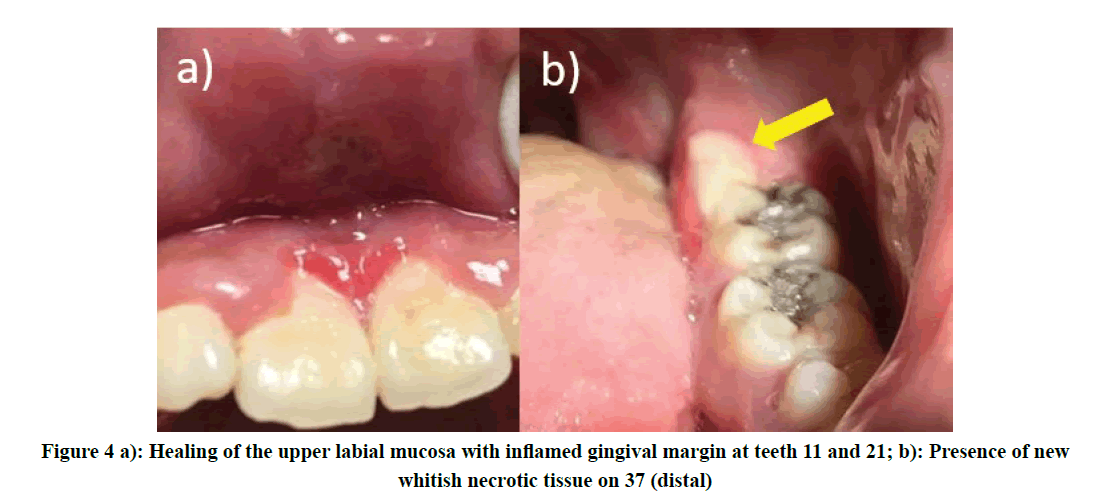
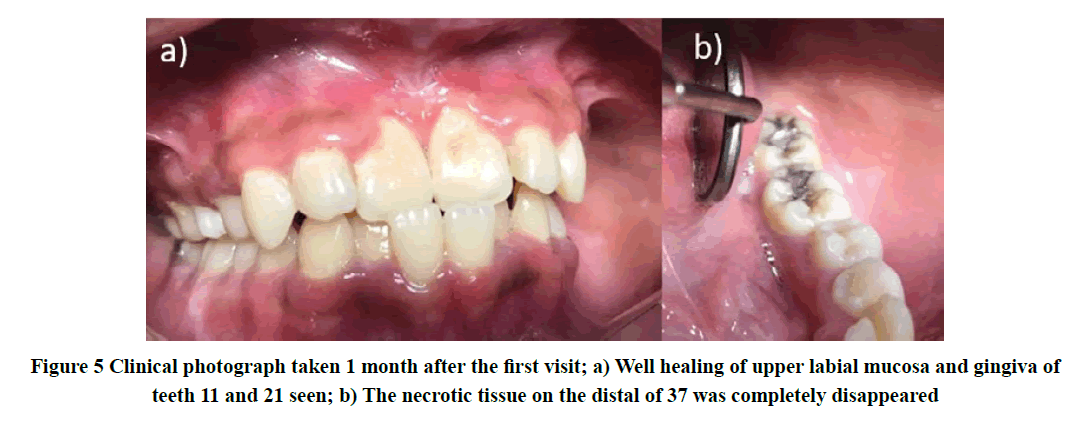
The patient was then reviewed weekly to observe the lesion and full mouth scaling was carried out completely as his medical condition has improved. Within 2-weeks of observation, the upper labial mucosa showed healing in progress but with redness of free gingiva. However, there was the presence of a similar new whitish lesion noted at the mucosa distal to tooth 37 (Figure 4). Gengigel® was applied onto the lesion and the patient was advised to continue practice good oral hygiene care. Fortunately, there was complete healing observed in the week after, although gingival contour appeared steep scalloping at teeth 11 and 21 (Figure 5).
Eventually, his condition improved with resolving his systemic state during hospitalization, and was discharged. He had been prescribed oral prednisolone taken once daily for 2 weeks. At this stage, the definitive diagnosis of his medical condition was not yet confirmed. Follow-up for dental review was given after two weeks in which he came with no complaint of any pain intra-orally. He also felt that his upper front teeth were no longer mobile. Motivation and oral hygiene instructions were given to the patient. He was informed regarding his current dental status, treatment plan, and potential outcomes after treatment. The patient was called for another two weeks to monitor his gingival condition and oral hygiene.
The medical diagnosis was turned to be a Myelodysplastic Syndrome/Myeloproliferative Neoplasms (MDS/MPN) thus he was planned for bone marrow transplant once the donor among his siblings has been determined from the laboratory result. Meanwhile, he was once again hospitalized for 20 days due to fever and upper respiratory tract infection with left-hand thrombophlebitis. He also complains of pain and having difficulty in swallowing his medications and food. He was treated by a hematologist accordingly until fully recovered from the conditions.
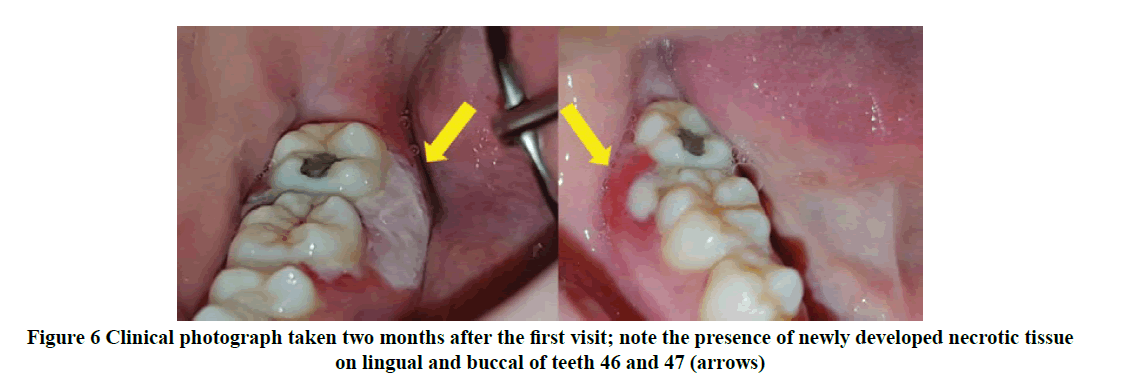
During this hospitalization, he also complains of painful ulceration on the lower right gum which was like his previous experience on his upper labial region. On a further examination, there was a presence of pseudomembranous whitish lesion suggesting necrotic tissue on the lingual of teeth 46 to 47, extending towards the distobuccal surface of tooth 46 (Figure 6). The lesion was firmly attached to the underlying gingiva and tender on palpation.
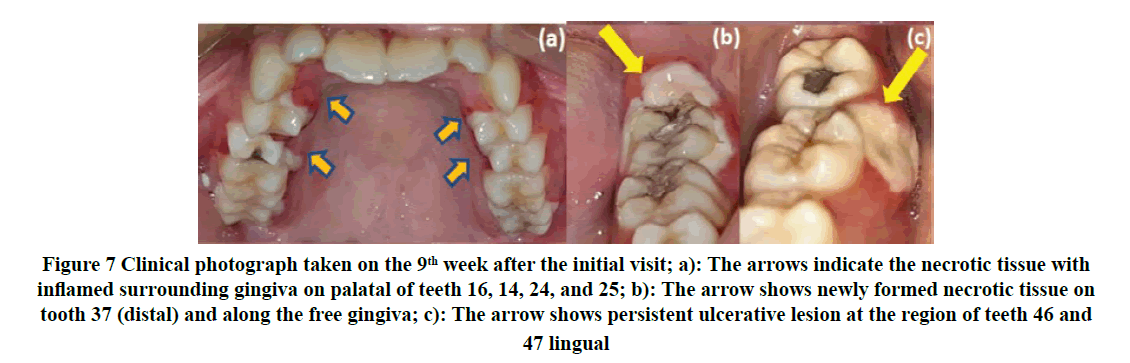
Localized scaling was done under local anesthesia on teeth 46 and 47 (distobuccally and distolingually) to remove plaque and subgingival calculus which could be the local predisposing factors. The area was irrigated with 0.2% CHX solution and he was advised to continue mouth rinsing twice daily while admitted. However, one week later, he still complain of a painful gum ulcer which showed the new pseudomembranous whitish lesion has spread to other regions in all quadrants (Figure 7).
Figure 7. Clinical photograph taken on the 9th week after the initial visit; a): The arrows indicate the necrotic tissue with inflamed surrounding gingiva on palatal of teeth 16, 14, 24, and 25; b): The arrow shows newly formed necrotic tissue on tooth 37 (distal) and along the free gingiva; c): The arrow shows persistent ulcerative lesion at the region of teeth 46 and 47 lingual
Samples of partial pseudomembranous whitish ulcerative lesions at tooth 14 (palatal) and 37 (distal) had been taken and sent for histopathological examination. A smear sample was performed from the dorsum of the tongue and was sent for Periodic Acid Schiff (PAS) staining. The report showed desquamated epithelial cells and non-specific microbial colonies from the tongue smear. No candida hyphae are seen from the sample. PAS stain was also negative indicating there was no active fungal infection. Samples taken from the lesions revealed necrotic tissue debris with the polymorphonuclear leukocytes and apoptotic cells interspersed. Therefore, the whitish lesion of the gingiva was confirmed to be necrotic and no tissue overgrowth. The patient was advised to continue mouth rinsing once daily by using CHX oral rinse and to take a soft diet. He also was encouraged to ensure his oral hygiene was maintained at an optimum level to reduce his gingival problem.
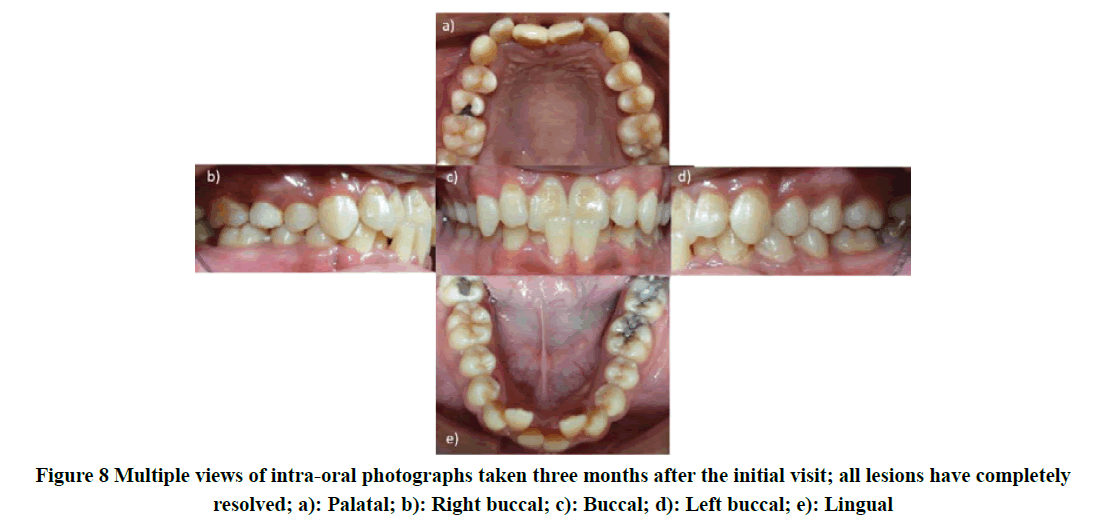
The patient was still under follow-up for his hematological condition and was scheduled for a bone marrow transplant. One month later, upon dental review, the patient still appeared lethargic, but his condition was slightly improved. Oral examination revealed that the entire whitish ulcer lesion had completely disappeared (Figure 8) and he able to perform the daily oral hygiene measures adequately as reflected by the very minimal plaque accumulation. However, the patient’s medical condition was getting worse, and then admitted again. He was not able to survive and had died 6 months later.
Discussion
This current report presents a case of a patient with necrotizing gingivitis as a manifestation of MDS/MPN with plaque-induced generalized chronic gingivitis. The main objective of periodontal therapy for this patient was to halt the progression of his gingival condition and to provide a stable periodontal environment while he is under active treatment for the hematological disease.
The MDS/MPN is a group of chronic clonal myeloid neoplasms characterized by a paradoxical phenotypic presentation of both MDS and MPN [4,5]. It is a heterogeneous stem cell disorder of blood and marrow with the presence of persistent cytopenia(s), dysplasia of various cell lines cells, and genetic markers [6]. The MPN-like features include constitutional symptoms such as night sweats and/or weight loss, elevated blood counts as well as extra-medullary infiltration. The low blood counts may lead to MDS symptoms e.g. tiredness, pale skin, mouth sores, skin infections, petechia, and bleeding gums.
In the revised 4th edition of the World Health Organization (WHO) classification, there are five distinct entities under MDS/MPN overlap syndromes namely Chronic Myelomonocytic Leukemia (CMML), Juvenile Myelomonocytic Leukemia (JMML), atypical Chronic Myeloid Leukemia (aCML), MDS/MPN unclassifiable (MDS/MPN-U), and MDS/MPN with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T) [5]. The latter was initially grouped under a provisional entity known as refractory anemia with ring sideroblasts and thrombocytosis [7,8]. In general, the respective disorders are identified by the presence of predominant myeloid subset such as the expansion of peripheral blood monocytes in CMML and JMML, and dysplastic granulocytes in aCML. In MDS/MPN-U, there is an occurrence of overlapping myeloproliferative and myelodysplastic features at presentation and not meeting criteria for other subtypes [7]. For this young boy’s medical condition of MDS/MPNs, currently, it has not been allocated to any subgroup.
It has been reported that the incidence rate of MDS/MPNs is about 4.3 cases per one million person-years which is commonly seen in elderly males (CMML the most frequent subtype) with the age group of 60-69 years [9,10]. These disorders rarely occurred among younger age groups, thus detection of our patient with MDS/MPNs at the age of 16 years old requires further understanding. The treatment options for this group of disorders were limited and the affected patients usually showed poor prognostication [7]. The recommended treatment was mostly deduced from clinical trials that focused on MDS/MPN patients, hence very few overlap syndrome patients were included. Several pharmacologic agents have been established, nevertheless, none have shown an effect on the natural history of the diseases [11]. Therapeutic approaches are mainly targeted at alleviating the predominant myelodysplastic or myeloproliferative features presented in specific cases.
The treatment options consist of supportive care, such as red blood cell and platelet transfusions, antibiotics, growth factors, and iron chelators. The Food and Drug Administration (FDA) has approved some medications to treat MDS such as azacitidine, decitabine, and lenalidomide; immunosuppressive therapy, chemotherapy, and stem cell transplantation [12]. There is no standard treatment in MDS/MPN, and allo-SCT (allogeneic hematopoietic stem cell transplantation) appears to be the only strategy that offers a potential long-term remission [7]. This was taken quite sometimes as the investigation has to be conducted for the identification of the compatible donor of hematopoietic stem cell among his siblings before the allo-SCT to be carried out.
The oral cavity is the frequent site of MDS/MPNs manifestations as a result of quantitative and qualitative blood abnormalities, as well as chemotherapy [13]. The incidence of oral complications in MDS ranges between 15% and 85% [14]. The common oral complications include gingivitis, periodontitis, spontaneous bleeding from the gingiva, soft tissue ulcerations, exacerbation of chronic periodontal and other oral tissue infections by bacterial, fungal, and viruses [1,12].
Epstein, et al. reported a case of an MDS/MPN patient who presented with gingival enlargement, which was firm, hemorrhagic but not inflamed [14]. During the further assessment, they reported the gingival enlargement continued to progress with ulceration and pseudo-membrane formation. The almost similar clinical findings were found in this case as the patient developed a pseudomembranous whitish lesion which was painful upon palpation and showed necrotic features. The lesion also was not generalized and presented at different locations during each time after recurrence. Histopathological examination was performed on the sample of the pseudomembranous whitish lesion which was detached from the free gingiva. Samples taken from the lesions revealed necrotic tissue debris with the poly-morphonuclear leukocytes and apoptotic cells interspersed. Therefore, the whitish lesion of the gingival was interpreted to be necrotic and no tissue overgrowth was found.
According to the location of the tissue affected by the acute disease process, necrotizing periodontal diseases can be classified as necrotizing gingivitis affecting only the gingival tissues, necrotizing periodontitis when involves the periodontal ligament and the alveolar bone, leading to attachment loss, and necrotizing stomatitis by which the necrosis progresses to deeper tissues beyond the mucogingival line, including the lip, cheek mucosa, or the tongue [15,16]. In this patient, only the gingival tissues were affected which therefore a diagnosis of Necrotizing Gingivitis (NG) was established. Patients with NG are frequently susceptible to future disease recurrence, mostly because of the difficulties in controlling predisposing factors as well as the difficulty in achieving proper supragingival biofilm control, in part because of the sequelae of these diseases, including the presence of gingival craters [17].
The diagnosis is based on the presence of necrosis and ulcers of the free gingiva. These lesions usually start at the interdental papilla and have a typical ‘punched-out’ appearance. In this case, there was the presence of pseudomembrane over the necrotic area which consists of a whitish-yellow colored meshwork, composed of necrotic tissue, fibrin, erythrocytes, leukocytes, and bacterial cells. When this ‘membrane’ is removed, the underlying connective tissue became exposed and bleeds as seen in this patient.
Based on the clinical findings, it has been identified that the necrotizing gingival condition recurred during his admission to the hospital due to lethargies and infections such as upper respiratory tract infection and left-hand thrombophlebitis. Therefore, this coincidental finding might indicate the gingival lesion tends to appear when the patient in the immunecompromised state [16]. Oral evaluation and treatment of pre-existing dental disease are recommended in immunecompromised patients to reduce the risk of septicemia arising from the oral cavity [18].
Conclusion
The purpose of this case report was to emphasize that acute necrotizing gingivitis can be an oral manifestation of MDS. The physician and dentist must be aware of the changes in the oral cavity of patients suffering from these hematological disorders. This may avoid missed diagnosed by the dentist for a long period and repeated visits during management Thus, patients with an MDS/MPNs should be given periodic oral examinations as a routine part of their management. Non-surgical periodontal therapy could be advocated for affected patients to help improve and stabilize the overall periodontal health besides close monitoring of oral health status. This may prevent the occurrence of an acute gingival condition despite the debilitating medical condition. Nevertheless, this patient had suffered from his poor medical status and could not survive longer.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Prasad, S. R., and Jayaram R. Anitha. "Oral manifestations of myeloid neoplasms and acute leukemia-A diagnostic perspective." Hematology and Transfusion International Journal, Vol. 6, No. 5, 2018, pp. 177-80.
- Tsuda, Kenji, et al. "Oral mucosal manifestations of chronic eosinophilic leukaemia with FIP1L1-PDGFRα." Case Reports, Vol. 2016, 2016.
- Ainamo, J., and I1 Bay. "Problems and proposals for recording gingivitis and plaque." International Dental Journal, Vol. 25, No. 4, 1975, pp. 229-35.
- Campo, Elias, et al. "The 2008 WHO classification of lymphoid neoplasms and beyond: Evolving concepts and practical applications." Blood, The Journal of the American Society of Hematology, Vol. 117, No. 19, 2011, pp. 5019-32.
- Pati, Haraprasad, and Karthika Kundil Veetil. "Myelodysplastic Syndrome/Myeloproliferative Neoplasm (MDS/MPN) overlap syndromes: Molecular pathogenetic mechanisms and their implications." Indian Journal of Hematology and Blood Transfusion, Vol. 35, No. 1, 2019, pp. 3-11.
- Dao, Kim-Hien T. "Myelodysplastic syndromes: Updates and nuances." Medical Clinics, Vol. 101, No. 2, 2017, pp. 333-50.
- Clara, Joseph A., David A. Sallman, and Eric Padron. "Clinical management of myelodysplastic syndrome/myeloproliferative neoplasm overlap syndromes." Cancer Biology and Medicine, Vol. 13, No. 3, 2016, pp. 360-72.
- Arber, Daniel A., et al. "The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia." Blood, Vol. 127, No. 20, 2016, pp. 2391-405.
- Srour, Samer A., et al. "Incidence and patient survival of myeloproliferative neoplasms and myelodysplastic/myeloproliferative neoplasms in the United States, 2001-12." British Journal of Haematology, Vol. 174, No. 3, 2016, pp. 382-96.
- Lim, Yoojoo, Jeong-Ok Lee, and Soo-Mee Bang. "Incidence, survival and prevalence statistics of classical myeloproliferative neoplasm in Korea." Journal of Korean Medical Science, Vol. 31, No. 10, 2016, pp. 1579-85.
- Padron, Eric. "Surveying the landscape of MDS/MPN research: Overlap among the overlap syndromes?" Hematology 2014, the American Society of Hematology Education Program Book, Vol. 2015, No. 1, 2015, pp. 349-54.
- Carl, William, and Maria Baer. "Prophylaxis and treatment of the oral complications of the myelodysplastic syndromes." Quintessence International, Vol. 22, No. 10, 1991, pp. 801-06.
- Pereira, Claudio M., et al. "Severe gingival bleeding in a myelodysplastic patient: Management and outcome." Journal of Periodontology, Vol. 75, No. 3, 2004, pp. 483-86.
- Epstein, J. B., et al. "Oral manifestations in myelodysplastic syndrome: Review of the literature and report of a case." Oral surgery, Oral Medicine, Oral Pathology, Vol. 61, No. 5, 1986, pp. 466-70.
- Horning, Gregory M., and Mark E. Cohen. "Necrotizing ulcerative gingivitis, periodontitis, and stomatitis: Clinical staging and predisposing factors." Journal of Periodontology, Vol. 66, No. 11, 1995, pp. 990-98.
- Herrera, David, et al. "Acute periodontal lesions (periodontal abscesses and necrotizing periodontal diseases) and endoâ?periodontal lesions." Journal of Clinical Periodontology, Vol. 45, 2018, pp. S78-94.
- MacCarthy, Denise, and Noel Claffey. "Acute necrotizing ulcerative gingivitis is associated with attachment loss." Journal of Clinical Periodontology, Vol. 18, No. 10, 1991, pp. 776-79.
- Mufti, Ghulam J., et al. "Diagnosis and classification of myelodysplastic syndrome: International Working Group on Morphology of Myelodysplastic Syndrome (IWGM-MDS) consensus proposals for the definition and enumeration of myeloblasts and ring sideroblasts." Haematologica, Vol. 93, No. 11, 2008, pp. 1712-17.