Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 5
Post-Percutaneous Coronary Intervention, Giant Left Circumflex Artery Pseudoaneurysm-A Rare Incidental Finding
Sandeep Nagulapally* and Amber S PapalkarSandeep Nagulapally, Department of Radiodiagnosis, Krishna Institute of Medical Sciences Secunderabad, Telangana, India, Tel: 02164241555, Email: sinaawayya@gmail.com
Received: 21-Apr-2021 Accepted Date: May 18, 2021 ; Published: 25-May-2021
Abstract
Percutaneous coronary intervention is a useful non-surgical technique widely used in the treatment of angina. One of the rare complications that can develop after a percutaneous coronary intervention is a coronary pseudoaneurysm. These aneurysms may cause stent thrombosis and coronary rupture leading to life-threatening cardiac tamponade. Therefore, it is important to detect and diagnose high-risk Coronary Pseudoaneurysms (CPSA) early so that prompt treatment can be initiated. Here, we present a case of an asymptomatic cardiac patient who previously underwent Percutaneous Coronary Intervention (PCI) and was being evaluated for an unrelated intraspinal tumor requiring neurosurgical excision and incidentally found to have a large pseudoaneurysm of the Left Circumflex (LCx) artery on CT coronary angiography.
Keywords
CT coronary angiography, Giant pseudoaneurysm, Left circumflex arterys
Abbreviations
PCI: Percutaneous Coronary Intervention; LAD: Left Anterior Descending; OM: Obtuse Marginal; CAA: Coronary Artery Aneurysm; CPSA: Coronary Artery Pseudoaneurysm; CABG: Coronary Artery Bypass Graft; LCx: Left Circumflex artery; CAD: Coronary Artery Disease; CTCA: Computed Tomography Coronary Angiography
Introduction
A coronary artery aneurysm is defined as a focal dilation of a coronary artery segment whose diameter exceeds that of the adjacent normal coronary artery by a maximal luminal diameter of at least 50%. Coronary Artery Aneurysms (CAA) are further classified as true or false [1]. The wall of a true aneurysm contains all three vascular layers (i.e., intima, media, and adventitia). A false aneurysm or Coronary Artery Pseudo-Aneurysm (CPSA) lacks at least one of these layers of the arterial wall and consists of an outwardly bulging monolayer or double layer, which develops from loss of vessel wall integrity, typically with disruption of the external elastic membrane. A giant aneurysm has been defined as when the maximal diameter exceeds 20 mm in adults or 8 mm in children [2].
The incidence is approximately from 0.02% to 0.03% in the normal population and 1.4% to 4.9% in individuals with coronary angiography [3]. Giant CAA is associated with advanced age, the tendency for complications including rupture, and may present as a mediastinal, intracardiac mass or superior vena cava syndrome, cardiac tamponade in addition to ischemic symptoms. CT coronary angiography is a simple, non-invasive method used to diagnose suspected complications and confirm the same, before the use of conventional angiography, especially in asymptomatic patients who are on follow-up [4].
Case Report
We present the case of a 50-year-old male, a known case of coronary artery disease who presented with paraparesis, which on evaluation was explained by a spinal cord space-occupying lesion. He was planned for a neurosurgical excision. He had a history of percutaneous coronary intervention after the diagnosis of diffuse anterior wall STsegment elevation myocardial infarction and underwent stenting to the Left Anterior Descending (LAD) 6 months ago and to the LCx 1 month back.
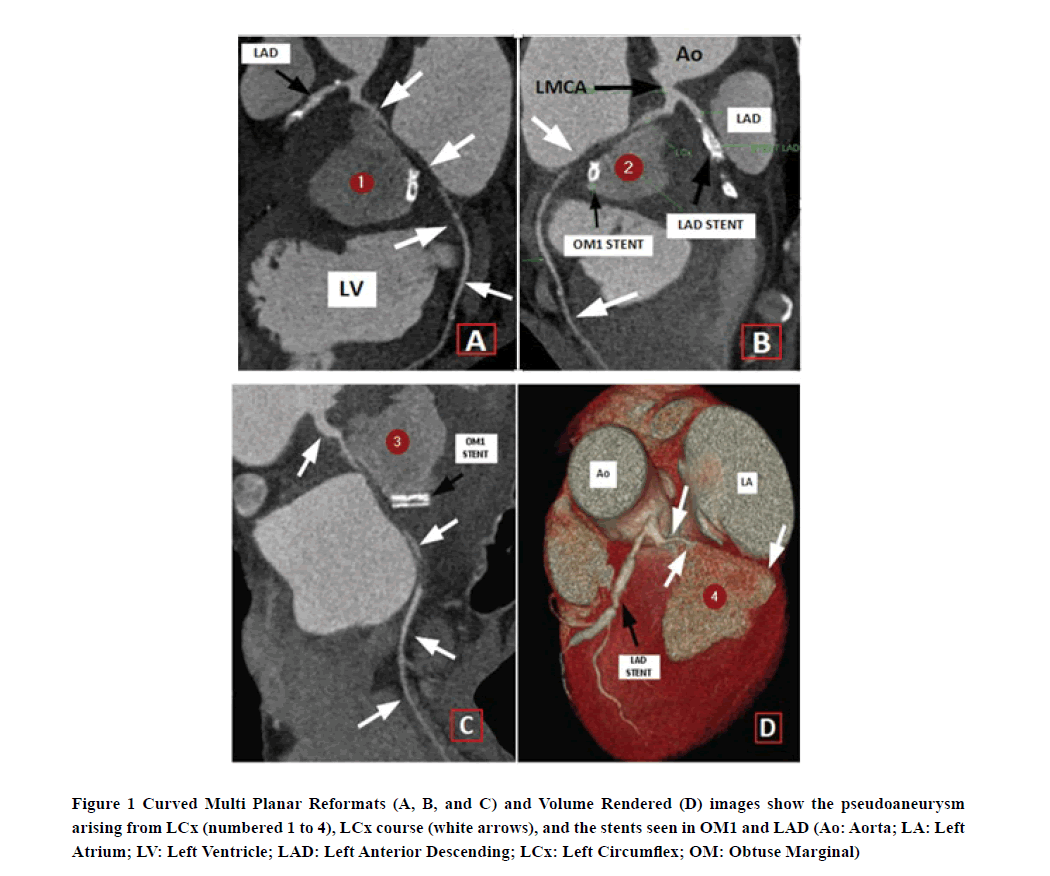
As part of the neurosurgical preoperative profile and with a background history of CAD and recent PCI, a CT coronary angiography was performed despite having no active chest-related complaints. CTCA showed a large contrast opacified collection seen involving the basal anterolateral wall of the left ventricle measuring (4.5 × 4.1 × 3.5) cm, which was communicating with the proximal portion of LCx suggesting pseudoaneurysm formation. A segment of proximaldistal LCx was non-opacified.
Distal LCx showed reformation by collaterals. In the first obtuse marginal branch of LCx (OM1), a stent was seen along the inferior aspect of the pseudoaneurysm. OM1 branch was not opacified. The LAD stent was patent and showed no in-stent stenosis or pseudoaneurysm formation.
After the CTCA which helped diagnose the giant pseudoaneurysm, coronary artery bypass grafting and pseudoaneurysm resection were planned to prevent adverse cardiac outcomes. The imaging also helped in counseling the patient adequately about the necessity of treating the coronary pseudoaneurysm first before proceeding for the spinal mass neuro-surgery. Written informed consent was obtained from the patient.
The patient had refused further intervention and hence was treated with aggressive medical management. The patient has been stable without any cardiac complaints (Figure 1).
Figure 1. Curved Multi Planar Reformats (A, B, and C) and Volume Rendered (D) images show the pseudoaneurysm arising from LCx (numbered 1 to 4), LCx course (white arrows), and the stents seen in OM1 and LAD (Ao: Aorta; LA: Left Atrium; LV: Left Ventricle; LAD: Left Anterior Descending; LCx: Left Circumflex; OM: Obtuse Marginal)
Discussion
The peculiarity, in this case, was that the patient was having a large pseudoaneurysm, yet was asymptomatic. A CT coronary angiography was performed to know the stent patency and also for the preoperative neurosurgical profile. This showed a surprisingly large pseudoaneurysm which was also possibly causing extrinsic compression on the stent. The stent which was placed in the OM1 branch of LCx showed no opacification.
A universally accepted definition of a giant Coronary Artery Aneurysm (CAA) does not exist: diameters of greater than 20 mm, 40 mm, 50 mm, and quadruple the reference vessel diameter have all been proposed as definitive in the medical literature [5,6]. The pathogenesis of aneurysm formation after catheter-based interventions has been attributed to the use of an oversized balloon, high inflation pressures, coronary dissection, interventions in the setting of acute myocardial infarction, and inadequate healing due to anti-proliferative treatment with cortisone, colchicine, and antiinflammatory drugs.
Medical management with spontaneous resolution or vigilant observation and clinical follow-up, covered stents, drugeluting stents, bare-metal stents, coil embolization, or surgery involving CABG followed by resection or ligation of the PSA are possible treatment options [7].
CT coronary angiography is a non-invasive method that can be used not only for assessing anatomy, anatomic variants, patency in post stenting viability of graft in post grafting patients, but also in unusual circumstances like these where a major catastrophe could be prevented because of prompt diagnosis that helped in time management.
We performed coronary CT angiography as an electrocardiographically gated contrast medium-enhanced CT scan of the heart. The CT examination is performed after achieving adequate vasodilation with intravenous administration of metoprolol on the table after ruling out asthma, also given tablet Ivabradine 2 hours before the procedure to control the heart rate to less than 70 beats per minute. Scanning was performed between the tracheal bifurcation and the diaphragm; the start delay is defined by using a bolus-tracking technique with the following parameters: collimation, 2 × 32 × 0.6; rotation time, 330 m/sec; tube voltage, 100 kV-120 kV; effective tube current, 800 mA; and pitch, 0.25.
Chen, et al. reported a case of a 49-year-old man with unstable angina for which paclitaxel-eluting stent implantation was done into proximal LAD. One month after the procedure cardiac computed tomography revealed pseudoaneurysm at mid-portion of the stent, which resolved spontaneously [8].
Another case by Kapoor, et al. reported a case of a 50-year-old man who presented with unstable angina initially had PCI done. After 8 weeks of intervention, he developed recurrent angina. On evaluation, a coronary PSA of the LAD was found and was subsequently treated with CABG [9].
In the present setting, as in our case, percutaneous intervention was necessary and would have been associated with an adverse outcome if undiagnosed or neglected. Treatment should be considered for coronary revascularization and management of the coronary artery pseudoaneurysm on a case-by-case basis. In addition, enhancement of the entire pseudoaneurysm on CT coronary angiography implied the risk of aneurysm rupture.
The prognosis of an atherosclerotic coronary aneurysm is usually favorable compared to a pseudoaneurysm developing after PCI. The risk is due to thrombosis with distal embolization or rapid enlargement and rupture leading to cardiac tamponade [1].
Conclusion
A diagnosis of giant pseudoaneurysm with the help of CT coronary angiography has helped in decision making with regards to patient management and counseling and hence preventing catastrophic events like cardiac tamponade from pseudoaneurysm rupture.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Aqel, Raed A., Gilbert J. Zoghbi, and Ami Iskandrian. "Spontaneous coronary artery dissection, aneurysms, and pseudoaneurysms: A review." Echocardiography, Vol. 21, No. 2, 2004, pp. 175-82.
- Díaz-Zamudio, Mariana, et al. "Coronary artery aneurysms and ectasia: Role of coronary CT angiography." Radiographics, Vol. 29, No. 7, 2009, pp. 1939-54.
- Yuan, Xinchun, Jia Hu, and Chunxiao Zhao. "Case Report Echocardiographic diagnosis of giant coronary aneurysm: A case report." International Journal of Clinical and Experimental Medicine, Vol. 11, No. 11, 2018, pp. 12729-33.
- Pugliese, Francesca, et al. "Multidetector CT for visualization of coronary stents." Radiographics, Vol. 26, No. 3, 2006, pp. 887-904.
- Crawley, Patricia D., et al. "Giant coronary artery aneurysms: Review and update." Texas Heart Institute Journal, Vol. 41, No. 6, 2014, pp. 603-08.
- Eshtehardi, Parham, et al. "Giant coronary artery aneurysm: imaging findings before and after treatment with a polytetrafluoroethylene-covered stent." Circulation: Cardiovascular Interventions, Vol. 1, No. 1, 2008, pp. 85-86.
- Pande, Abhay K., Ravi R. Kasliwal, and Naresh Trehan. "Spontaneous primary coronary artery dissection leading to pseudoaneurysm." International Journal of Cardiology, Vol. 42, No. 1, 1993, pp. 97-99.
- Chen, David, et al. "Spontaneous resolution of coronary artery pseudoaneurysm consequent to percutaneous intervention with paclitaxel-eluting stent." Texas Heart Institute Journal, Vol. 35, No. 2, 2008, pp. 189-91.
- Kapoor, Aditya, et al. "Coronary pseudoaneurysm in a non-polymer drug-eluting stent: A rare entity." Asian Cardiovascular and Thoracic Annals, Vol. 19, No. 6, 2011, pp. 407-10.