Research Article - International Journal of Medical Research & Health Sciences ( 2025) Volume 14, Issue 1
Prevalence of Different Morphological Types of Anemia and Its Significance in Haemodialysis Patients: A Unicentric Study in a Tertiary Care Hospital
Arif Hoda*Arif Hoda, Department of Nephrology, Medical College and Hospital, Maharashtra, India, Email: hodaarif@gmail.com
Received: 19-Dec-2023, Manuscript No. IJMRHS-23-123101; Editor assigned: 22-Dec-2023, Pre QC No. IJMRHS-23-123101(PQ); Reviewed: 06-Jan-2024, QC No. IJMRHS-23-123101; Revised: 10-Feb-2025, Manuscript No. IJMRHS-23-123101(R); Published: 17-Feb-2025
Abstract
Background: Anaemia occurs in the early stages of kidney disease and worsens as kidney function deteriorates. Typical consequences of pneumonia are impaired erythropoietin production, iron and vitamin deficiency, blood loss, shortened erythrocyte life, chronic inflammation, and a uremic environment.
Aim: To identify morphological classification of different types of anemia present in hemodialysis patients with chronic kidney diseases.
Patients and methods: After obtaining informed consent, 4 mL of blood was collected from the vein of each participant for a Complete Blood Count (CBC) and peripheral film report. The CBC was performed using a haematology analyser. All these patients were previously diagnosed with chronic kidney failure and were on haemodialysis with an average duration of 4 years. They developed anaemia during their illness, so the patients were evaluated to find out the cause of the anaemia. Depending on haematological laboratory data, peripheral blood smear examinations of these 22 patients showed different morphological types of anemia. All patients were on baseline erythropoietin at 10,000 IU per week.
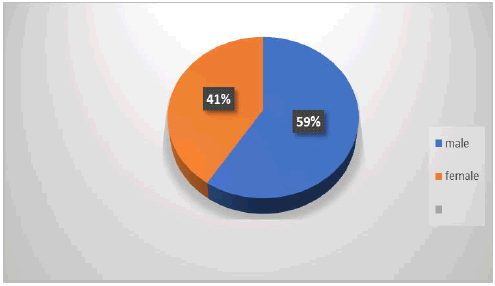
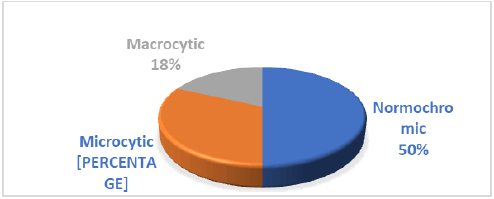
Results: In this study, 30 patients were included, of whom 22 were anaemic: 14 males (59%) and 9 females (41%). The age range was 35–75 for males and 27–62 for females. The most common types of anemia were normochromic anaemia (50%), which developed in 11 patients, followed by hypochromic microcytic anaemia (31.81%), which developed in 7 patients, and macrocytic anemia (18.18%), which developed in 4 patients. Iron deficiency was notable found in microcytic anemia and also was seen in few cases of normocytic and macrocytic anemia also.
Conclusion: Anemia from chronic diseases was the most frequent in hemodialysis patients. There are higher levels of inflammatory parameters in hemodialysis patients than in healthy controls. Normochromic anaemia was the most prevalent type, followed by microcytic hypochromic and then macrocytic hypochromic. Inflammatory markers were higher in most of the patients with normocytic normochromic relationships, with inflammation being the cause of EPO resistance.
Keywords
Anemia, Microcytic, Normocytic, Hypochromic, Iron deficiency
Introduction
Anemia is defined as the concentration of Haemoglobin (Hb) in the blood being below 2 times the standard deviation of the mean Hg of the general population, corrected for age and sex. The following threshold values for Hb<13 g/dl in men and Hb<12 g/dl in women make the diagnosis of anemia according to WHO classification (1) Anemia is a common complication of Chronic Kidney Disease (CKD) and causes increased morbidity and mortality. There are various causes of renal anemia, such as decreased production of Erythropoietin (EPO), r esistance to EPO, shortened survival of Red Blood Cells (RBCs), etc. This decrease in EPO matches the decline in kidney function and is the main determinant of anemia in CKD. Iron deficiency is common in India because of low socio-economic status. The activation of the complement pathway stimulates the degranulation of mast cells and the release of inflammatory cytokines. Inflammation is a rapid and acute protective response to infection or trauma [1].
Anemia represents a significant problem to deal with in patients with Chronic Kidney Disease (CKD) on Hemodialysis (HD). Renal anaemia is typically an isolated normochromic, normocytic anaemia with no leukopenia or thrombocytopenia. This is a frequent complication and contributes considerably to the reduced Quality of Life (QoL) of patients with CKD. It has also been associated with a number of adverse clinical outcomes, including increased morbidity and mortality. In general, there is a progressive increase in the incidence and severity of anaemia with declining renal function. The reported prevalence of anaemia by CKD stage varies significantly and depends, to a large extent, on the definition of anaemia and whether study participants selected from the general population are at a high risk for CKD. Hence, we study in our hospital the probable cause and different morphologies associated with anemia [2].
Materials and Methods
This was a cross-sectional observational study conducted at a tertiary care hospital. Patients included in this study were >18 years of age with CKD stage 5D on haemodialysis. Anemia was defined according to WHO guidelines, with male Hb>13 and female Hb>12. A sample size was selected for all patients undergoing haemodialysis in our centre. Depending on clinical signs, symptoms, and laboratory diagnostic tests, all those patients were previously diagnosed with chronic renal failure and was on heamodialysis. Therefore, all laboratory tests were performed, including a complete blood count, peripheral smear, CRP done by Latex enhanced immuno turbidimetry, serum iron done by ferene triazine method, total iron-binding capacity by chromazurol B test, serum ferritin by Chemiluminescence Immunoassay (CLIA), and serum vitamin B12 by CLIA method for identification of the type of anemia in CKD. Transferrin Saturation (TSAT) is calculated as (Serum iron/Serum TIBC) × 100. Written consent was obtained from all patients for this study [3].
After a good cleaning of the patient's venepuncture site, 8 ml of venous blood was collected using standard collecting techniques and the collected blood sample was processed as follows:
• 4 ml of venous blood is added to a disposable tube containing an anticoagulant (EDTA K2, purple cap), after which the tube is repeatedly inverted several times so that the blood mixes well with the anticoagulants and used to collect the whole blood count, blood film, ESR, CRP, and reticulocyte count using the Mindray Automated Hematology Auto Analyzer (Cell Counter) and Sysmex.
• Another 4 ml of venous blood was added to the gel tube and, after 5 minutes, centrifuged at 4000 rpm for 10 minutes to obtain serum, which was used for the determination of serum iron, serum total iron binding capacity enzyme essay, serum ferritin, and serum vitamin B12 using the Cobas e41 and Cobas Integra 400 methods.
Results
The results of this study were based on an analysis of 30 patients who are on maintenance heamodialysis. All patients are on injection EPO 10 thousand units of therapy (Table 1 and Figure 1). Out of 30 patients, 22 were found to be anemic. There were 13 males (59.09%) and 9 females (41%); the age group was 35–75 for males and 27–62 for females (Figure 2) [4].
| Sex | Numbers (%) | Age range ( years) |
|---|---|---|
| Male | 13 (59.09) | 35-75 |
| Female | 9 (41) | 27-62 |
Table 1 Classification of patients
Depending on the CBC analysis of laboratory data, peripheral blood smear examinations from these 22 patients, which showed different types of anemia, are shown below in the table. The most common types of anemia were normocytic normochromic anemia, which develops in 11 patients, followed by microcytic hypochromic anemia, which develops in seven patients, and macrocytic hypochromic anemia, which develops in four patients. Microcytic hypochromic morphology combined with a high red cell distribution width was used to estimate the prevalence of iron deficiency [5].
The determination of types of anemia in those patients depends on the results of the haematological test, which was done for all the patients (Table 2 and Figure 3) [6].
| Types of anemia | Total numbers | Percentage (%) |
|---|---|---|
| Normocytic normochromic | 11 | 50 |
| Microcytic hypochromic | 7 | 31.81 |
| Macrocytic hyopocromic | 4 | 18.18 |
Table 2 Percentage of different types of anemia
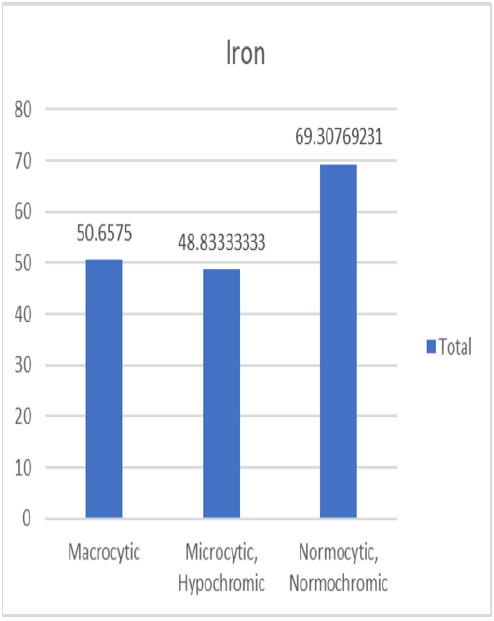
Mean haemoglobin with standard deviation noted was 9.1 ± 2.1 g/dl, 9.2 ± 2.4 g/dl, and 8.9 ± 2.6 g/dl and mean pack cell volume noted was 29.1 ± 5.8%, 27.9 ± 4.9%, and 29.4 ± 7.5% in normocytic, microcytic and macrocytic anemia, respectively. The mean with standard deviation of Mean Corpuscular Volume (MCV) was noted as 86 ± 4.1 fl, 71 ± 4.7 fl, and 104 ± 3.9 fl; Mean Hemoglobin Concentration (MCH) was noted at 27 ± 0.7 pg, 23 ± 1.5 pg, and 33 ± 2.0 pg; Mean Corpuscular Hemoglobin Concentration (MCHC) was noted at 32 ± 1.15 g/dL, 31.9 ± 1.19 g/dL, and 32.4 ± 1.27 g/dL; and Red Cell Distribution (RDW) was noted at 16 ± 2.5%, 18.6 ± 3.0%, and 16.5 ± 1.3% in normocytic, microcytic, and macrocytic anemia, respectively. Serum iron was low (60 mcg/dL) in 8 cases, 7 in microcytic anaemia and 1 in normocytic anemia, and TIBC (total iron binding capacity) was high in 9 (more than 450 mcg/dL) cases, and transferrin saturation, which was calculated using the formula TSAT=(serum iron/total iron binding capacity) ðÂÃÃÂ??ÂÃÂ?ÂÂ??100, showed 12 below the range of normal, which is 20 for males and 15 for females, which included 7 in microcytic anemia, 4 in normocytic anemia, and 1 in macrocytic anemia (Figures 4-6) [7].
Of the 11 normocytic anemia 7 showed raised CRP levels, 3 in microcytic anemia and 2 in macrocytic anemia. Vitamin B12 was noted low in 3 in macrocytic anemia and 2 in normocytic anemia. Ferritin was raised (>300 ng/mL) in 14 cases of 22 that is 64 % of cases.
Discussion
The cause of anemia can be varied in CKD and includes nutritional deficiency, increased pro-inflammatory cytokines, chronic blood loss and relative Erythropoietin (EPO) deficiency. Assessing anemia in chronic illnesses is a complex process, and this is particularly true for patients with CKD, particularly those from India, where IDA is a common condition [8].
The relative deficiency in Erythropoietin (EPO) production by the peritubular cells of the kidneys is responsible for defective erythropoiesis in CKD patients. Due to Erythropoietin deficiency there is disturbances in the differentiation and maturation of red blood cell precursors, and uremic toxins contribute to it.
In our study, the prevalence of anaemia was 73% in all dialysis-dependent patients. 59% were male and 41% were female, with a mean age of 55 and 46 years, respectively. Data from the National Health and Nutrition Examination
Survey (NHANES) showed that Hb levels starts to fall at an estimated glomerular filtration rate (eGFR) of less than 75 ml/min per 1.73 m2 in men and 45 ml/min per 1.73 m2 in women.
A review of National Health and Nutrition Examination Survey (NHANES) data determined that the prevalence of anaemia increased with stage of CKD, as follows:
• Stage 1: 8.4%
• Stage 2: 12.2%
• Stage 3: 17.4%
• Stage 4: 50.3%
• Stage 5: 53.4%
In the above study, we had 11 patients with normocytic normochromic anemia, which is seen in the anemia of chronic disease in CKD. However, iron deficiency was noted in 8 cases, 7 in microcytic anemia and 1 in normocytic anemia, and the transferrin saturation calculated showed 12 cases below the range of normal, which included 7 microcytic anemia, 4 normocytic anemia and 1 macrocytic anemia. Chronic inflammation plays an important role in the progression of CKD, and high levels of inflammatory markers appear to accompany reduced renal function. Inflammatory states also affect erythropoiesis via the inhibition of hypoxia-induced EPO production in Hep3B cells [9].
Elevated ferritin levels, low levels of serum iron, and iron-binding capacity, as well as a higher abundance of iron in the bone marrow, are the characteristic features of inflammatory associated anemia. Due to iron sequestration in reticuloendothelial cells there is inadequate plasma iron levels to perform erythropoiesis. In our patients, we had raised CRP levels in 63% of anemia cases, which denotes an inflammatory cause of anemia in CKD. In few studies hemodialysis patients with high CRP levels (>8 mg/L) have been shown to have lower iron absorption than patients with lower CRP levels [10].
We found that iron deficiency was noted in 8 cases and TSAT was low in 12 cases. Also, Serum ferritin was high in 64% of our cases. The TSAT corresponds to circulating iron, which is calculated using the formula: Serum iron divided by TIBC. Serum ferritin indirectly measures iron storage. As a surrogate marker for iron stores, serum ferritin is the most commonly used laboratory test to diagnose iron deficiency. However, as it a marker for acute-phase reactant, it is the mostly at higher levels in CKD which becomes an important drawback of measuring serum ferritin. Due to this, a wide range of reference limits for serum ferritin have been suggested to diagnose iron deficiency in patients with chronic inflammation especially in CKD. Clinical nephrology guidelines recommend the use of serum ferritin and the TSAT measure for the guidance of initiation of iron therapy. Serum ferritin less than 100 μg/L and TSAT less than 20% are taken as signs of iron deficiency in CKD and initiation of iron therapy. In a study by Chuang, et al., only 17% of iron-deficient haemodialysis patients who had low serum iron, had serum ferritin <300 μg/L [11].
In parallel with this study, the United States Renal Data System (USRDS) annual data report showed that mean serum ferritin levels remained stable at approximately 600 ng/mL from 2001 to 2006, but rose significantly to 800 ng/mL in 2011 in maintenance Haemodialysis (HD) patients. Also, Dialysis Outcomes and Practice Patterns Study (DOPPS) data showed that median serum ferritin levels rose from 561 ng/mL in 2010 to 794 ng/mL in 2012 in maintenance HD patients [12].
According to Besarab, et al. the losses of iron in haemodialysis patients reach 1–3 g per year and they are associated with chronic bleeding related to platelet dysfunction and also frequent phlebotomy, hemolysis, and blood retained in the extracorporeal circulation during heamodialysis. Additionally, patients undergoing dialysis show impaired dietary iron absorption [13].
We also noted macrocytic anemia in CKD in maintenance HD patients. This could be nutritional or may be due to inflammation caused in CKD leading to less absorption from the intestine leading to folate and vitamin B12 malabsorption and its deficiency [14]. The exact mechanism of the influence of the inflammatory state on the development of anemia may be related to hepcidin which affects iron homeostasis through the binding of the cell surface iron transporter ferroportin.
According to National Institute for Health and Care Excellence (NICE) the treatment of anemia in CKD patients requires the use of either iron or erythropoiesis-stimulating agents, their combination in order to address both absolute and functional iron deficiency, According to the KDIGO guideline 2012, the correction of iron deficiency with oral or intravenous iron supplementation can reduce the severity of anemia in patients with CKD [15].
The Correction of Hemoglobin and Outcomes in Renal Insufficiency (CHOIR) trial and The Trial to Reduce Cardiovascular Events with Aranesp Therapy (TREAT) demonstrated that higher haemoglobin targets may be harmful to patients which can lead to adverse events like myocardial infarction or stroke [16].
International guidelines recommend an upper limit of serum ferritin at 500 μg/L to avoid potential complications that are associated with iron therapy.
Within the dialysis CKD population, the prevalence of inflammation is in large numbers and is an important indicator of patient health and outcome, but the actual effect of chronic inflammation on renal function is unclear and the relationship between the level of inflammation and GFR has not been found to correlate as may be expected [17].
While epidemiological studies have shown better outcomes associated with the attainment of haemoglobin levels on mortality and hospitalisation in hemodialysis patients, the results of four key randomised clinical trials have not supported the hypothesis that full anaemia correction with ESAs is beneficial to all patients. Attempts to explain the apparent paradox between epidemiological and clinical data on Hb levels are grounded in the hypothesis that higher doses required in a subgroup of ESA hyporesponsive patients, precipitated by inflammation, may be the culprit rather than other causes of anemia [18,19].
Treatment of anemia of CKD has become a highly contentious topic, with growing concerns regarding the precise targets, safety, clinical evidence, questionable benefits and costs of present anemia management practices. There are increased calls for a re-evaluation of anemia management strategies in HD and for alternative approaches to help correct the disorder. While exogenous supplementation of EPO and iron remains the mainstay of anemia therapy in CKD, the potential for improving the condition by curbing underlying conditions that contribute to the pathogenesis of anemia, or by dialysis-specific approaches, have yet to be fully recognized. Newer therapy like Activins which includes sotatercept and luspatercept, sultuximab, hypoxia-inducible factor prolyl hydroxylase inhibitor (Hif1_inhibitors) which includes Vadustat, Daprodustat etc, Pentoxifylline are still under trials and show promising results [20].
Conclusion
It is obvious that renal anemia in hemodialysis patients remains a serious problem. This was greater before the EPO era, when blood transfusion was the only therapeutic approach. Insufficiencies of iron and EPO with inflammation are the most important causes of this anemia. Nowadays, with the availability of new IV iron supplements, ESAs and other upcoming drugs this problem has become more manageable. The high cost of the EPO treatment makes iron therapy essential in order to maximise the EPO administration result with a lower dose. The ideal haemoglobin target has to be established despite the numerous trials worldwide, and the treatment has to be individualized.
References
- Locatelli F, et al. Kidney Disease: Improving Global Outcomes guidelines on anaemia management in chronic kidney disease: a European Renal Best Practice position statement. Nephrology Dialysis Transplantation. Vol. 28, No. 6, 2013, pp. 1346-1359.
[Crossref] [Google Scholar] [PubMed]
- Babitt JL and Lin HY. Mechanisms of anemia in CKD. Journal of the American Society of Nephrology. Vol. 23, No. 10, 2012, pp. 1631-1634.
[Crossref] [Google Scholar] [PubMed]
- Brancaccio D, et al. Hyperparathyroidism and anemia in uremic subjects: a combined therapeutic approach. Journal of the American Society of Nephrology. Vol. 15, No. 1_suppl, 2004, pp. S21-24.
[Crossref] [Google Scholar] [PubMed]
- Mercadal L, et al. Timing and determinants of erythropoietin deficiency in chronic kidney disease. Clinical Journal of the American Society of Nephrology. Vol. 7, No. 1, 2012, pp. 35-42.
[Crossref] [Google Scholar] [PubMed]
- Valderrabano F, et al. Quality of life in end-stage renal disease patients. American Journal of Kidney Diseases. 2001 Vol. 38, No. 3, 2001, pp. 443-464.
[Crossref] [Google Scholar] [PubMed]
- Obrador GT, and Pereira BJ. Anaemia of chronic kidney disease: An underâ?recognized and underâ?treated problem. Nephrology Dialysis Transplantation. Vol. 17, No. suppl_11, 2002, pp. 44-46.
[Crossref] [Google Scholar] [PubMed]
- Merkus MP, et al. Quality of life in patients on chronic dialysis: self-assessment 3 months after the start of treatment. American Journal of Kidney Diseases. Vol. 29, No. 4, 1997, pp. 584-592.
[Crossref] [Google Scholar] [PubMed]
- Locatelli F, et al. Anaemia in haemodialysis patients of five European countries: association with morbidity and mortality in the Dialysis Outcomes and Practice Patterns Study (DOPPS). Nephrology Dialysis Transplantation. Vol. 19, No. 1, 2004, pp. 121-132.
[Crossref] [Google Scholar] [PubMed]
- Astor BC, et al. Kidney function and anemia as risk factors for coronary heart disease and mortality: the Atherosclerosis Risk in Communities (ARIC) Study. American Heart Journal. Vol. 151, No. 2, 2006, pp. 492-500.
[Crossref] [Google Scholar] [PubMed]
- Dhingra R, et al. Chronic kidney disease and the risk of heart failure in men. Circulation: Heart Failure. Vol. 4, No. 2, 2011, pp. 138-144.
[Crossref] [Google Scholar] [PubMed]
- Taddei S, et al. Hypertension, left ventricular hypertrophy and chronic kidney disease. Heart Failure Reviews. Vol. 16, 2011, pp. 615-620.
[Crossref] [Google Scholar] [PubMed]
- Vlagopoulos PT, et al. Anemia as a risk factor for cardiovascular disease and all-cause mortality in diabetes: the impact of chronic kidney disease. Journal of the American Society of Nephrology. Vol. 16, No. 11, 2005, pp. 3403-3410.
[Crossref] [Google Scholar] [PubMed]
- Parfrey P. Anaemia in chronic renal disease: lessons learned since Seville 1994. Nephrology Dialysis Transplantation. Vol. 16, No. suppl_7, 2001, pp. 41-45.
[Crossref] [Google Scholar] [PubMed]
- Madore F, et al. Anemia in hemodialysis patients: variables affecting this outcome predictor. Journal of the American Society of Nephrology. Vol. 8, No. 12, 1997, pp. 1921-1929.
[Crossref] [Google Scholar] [PubMed]
- Gaweda AE. Markers of iron status in chronic kidney disease. Hemodialysis International. Vol. 21, 2017, pp. S21-27.
[Crossref] [Google Scholar] [PubMed]
- Bataille S, et al. Indole 3-acetic acid, indoxyl sulfate and paracresyl-sulfate do not influence anemia parameters in hemodialysis patients. BMC Nephrology. Vol. 18, 2017, pp. 1-9.
[Crossref] [Google Scholar] [PubMed]
- Gluba-Brzozka A, et al. The influence of inflammation on anemia in CKD patients. International Journal of Molecular Sciences. Vol. 21, No. 3, 2020, pp. 725.
[Crossref] [Google Scholar] [PubMed]
- Stauffer ME, and Fan T. Prevalence of anemia in chronic kidney disease in the United States. PLoS One. Vol. 9, No. 1, 2014, pp. e84943.
[Crossref] [Google Scholar] [PubMed]
- Ganz T. Iron in innate immunity: starve the invaders. Current Opinion in Immunology. vol. 21, No.1, 2009, pp. 63-67.
[Crossref] [Google Scholar] [PubMed]
- Kooistra MP, et al. Iron absorption in erythropoietin-treated haemodialysis patients: effects of iron availability, inflammation and aluminium. Nephrology Dialysis Transplantation. Vol. 13, No. 1, 1998, pp. 82-88.
[Crossref] [Google Scholar] [PubMed]