Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 1
Scimitar Syndrome: A Rare Case Report
Gomathi Thirugnanam*Gomathi Thirugnanam, Department of Cardiology, Thanjavur Medical College Tamil Nadu, India, Tel: +91 661 246 2292, Email: gomathimd@gmail.com
Received: 02-Dec-2020 Accepted Date: Jan 22, 2021 ; Published: 29-Jan-2021
Abstract
Scimitar syndrome is a rare congenital anomaly. It is also known as hypogenetic lung syndrome. It is essentially a combination of pulmonary hypoplasia and Partial Anomalous Pulmonary Venous Return (PAPVR). There are manifestations of heart failure due to associated congenital heart disease in infants. Most of the adults are asymptomatic but may have exertional dyspnoea or recurrent respiratory infection. It almost exclusively occurs on the right side. It is diagnosed by transthoracic/transesophageal echocardiography or angiography. CT or MRI angiography also helps in the diagnosis. Surgical correction is indicated in the presence of significant left to right shunting and pulmonary hypertension. Creation of an intra-atrial baffle to redirect the pulmonary venous return into the left atrium. Otherwise, the anomalous vein can be re-implanted directly into the left atrium. Thrombosis, stenosis, and occlusion of the scimitar vein and its deviation are the complications of the surgery. This case report emphasizes the importance of a thorough clinical and echocardiographic examination to avoid the diagnosis of this rare congenital anomaly.
Keywords
Scimitar syndrome, Atrial septal defect, Echocardiogram
Introduction
Scimitar is a rare congenital cardiovascular abnormality. It is also known as pulmonary venolobar syndrome. It includes a hypoplastic right pulmonary artery and right lung, anomalous systemic arterial supply to the right lung, and anomalous right pulmonary vein. There is a displacement of cardiac structures into the right hemithorax due to hypoplastic right lung. It has characteristic features of curved anomalous venous drainage of the right pulmonary vein into the inferior vena cava. The syndrome is called Scimitar syndrome hence it resembles the curved Middle Eastern sword “Scimitar” [1,2]. The anomalous pulmonary vein descending below the diaphragm creating a half-crescent sign at the right side of the heart is the anatomic basis of this sign. It may be associated with a variety of congenital thoracic abnormalities [3]. Patients may present with a history of recurrent pneumonia, features of pulmonary hypertension, and/or chronic right ventricle volume overload.
Case Presentation
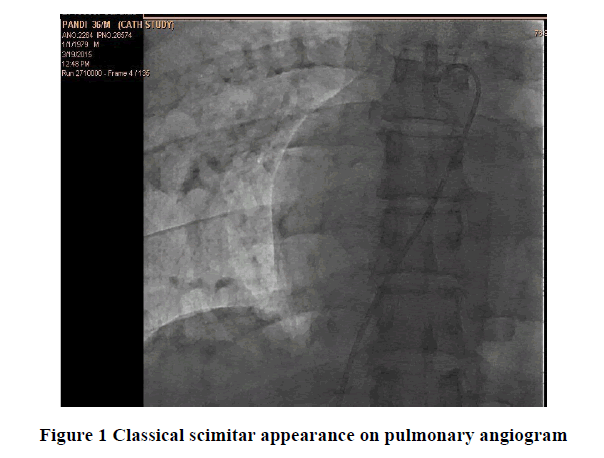
A 36-year-old man presented with chronic dyspnoea on exertion for 6 months duration. There was no significant co-morbid illness. General examination was normal. Cardiovascular examination showed systolic murmur in the pulmonary area and features of right ventricular volume overload. Electrocardiogram showed sinus rhythm with features of right ventricular strain pattern. Chest X-ray showed cardiomegaly. There is right atrial enlargement with classical scimitar appearance of right pulmonary venous drainage into the inferior vena cava. A provisional diagnosis of Scimitar syndrome was made.
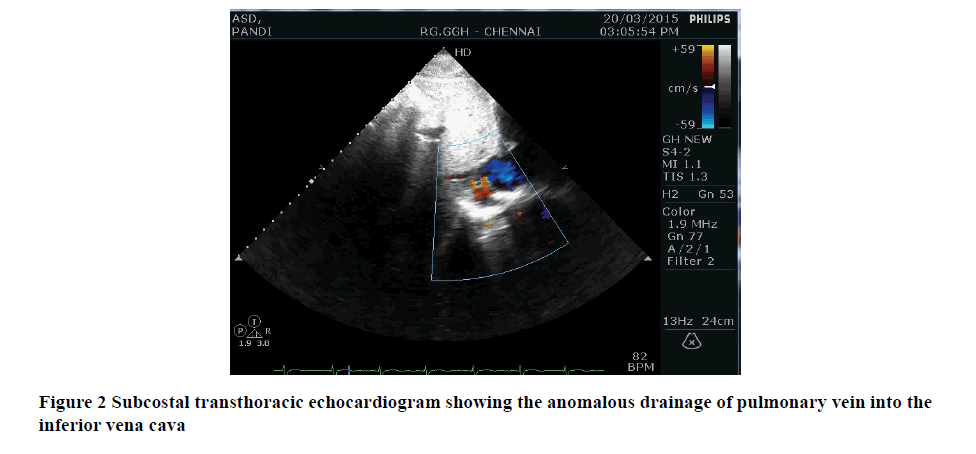
The patient was subjected to an echocardiogram. It revealed a large ostium secundum atrial septal defect with left to right shunt. There is a gross dilatation of right heart chambers with moderate pulmonary artery hypertension. There is abnormal drainage of the right pulmonary vein into the suprahepatic segment of the inferior vena cava. The right pulmonary artery was hypoplastic. There was preserved biventricular contractile function.
Cardiac catheterization was done. It showed dilated right-sided chambers with large ostium secundum atrial septal defect with QP:QS>2:1. The pulmonary angiogram showed a hypoplastic right pulmonary artery with the classic scimitar appearance of right upper pulmonary venous drainage into the inferior vena cava. The diagnosis of scimitar syndrome was confirmed. Surgical correction was planned due to the presence of symptoms with a large shunt and moderate pulmonary hypertension.
Discussion
The scimitar syndrome was first described by Chassinat in1836 [4]. The term “Scimitar” was coined by CA Neill et al., in 1960. It is associated with multiple cardiopulmonary anomalies [5,6]. It is a complex malformation of the lungs, heart, and blood vessels. The most common congenital heart disease associated with this syndrome is an atrial septal defect (70%) [7]. Other associated cardiac anomalies are ventricular septal defect, tetralogy of Fallot, patent ductus arteriosus, coarctation of the aorta, hypoplastic left heart syndrome, total anomalous pulmonary venous connection, cor triatriatum, bicuspid aortic valve, and subaortic stenosis [8-10]. Non-cardiac problems include ipsilateral diaphragmatic anomalies, localized bronchiectasis, horseshoe lung, vertebral anomalies, and genitourinary tract abnormalities. The patient may present with a repeated history of respiratory tract infections or features of pulmonary hypertension.
The diagnosis is made by transthoracic/transesophageal echocardiography or angiography. Chest X-ray findings are ipsilateral mediastinal shift with a small lung. In one-third of cases, a typical scimitar appearance due to the anomalous draining vein may be seen as a tubular structure paralleling the right heart border. The right heart border may be blurred. The presence of a left to right shunt may lead to the development of pulmonary hypertension and Eisenmenger physiology. The exact anatomy of the anomalous drainage is delineated by Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). They also give added information about the associated congenital defects of the lung, bronchovascular tree, or thoracic spine. Cine MRI and 3D contrast-enhanced MR angiography is the non-invasive tool in the evaluation of anomalous pulmonary venous drainage. Quantification of the left-to-right shunt is done either by dynamic MRI or cardiac catheterization.
Prenatal diagnosis is made by fetal echocardiogram. Color flow and spectral doppler will provide clues to an obstructed pulmonary venous drainage. Visualization of the confluence behind the right atrium and a vertical vein is the characteristic findings in echocardiography [11]. But the detection rate of these anomalies remains suboptimal [12,13].
Surgical correction is always required for the infantile form. Generally, the prognosis is poor for infantile form even with or without surgery. In adults, the indications for surgical corrections are recurrent respiratory tract infections, significant left-to-right shunting, or pulmonary hypertension. The main aim of the surgery is to avoid the sequelae of chronic volume overload [14-17]. Pneumonectomy of the hypoplastic lung or correction of the anomalous drainage by rerouting into the left atrium is the surgical option. Alternatively, the creation of a tunnel by an intra-atrial patch is used to redirect the anomalous pulmonary venous flow into the left atrium through an ASD. The free wall of the right atrium is also used to create a tunnel from the anomalous pulmonary vein to the left atrium across an ASD. This is described by Puig-Massana and Revuelta et al. [18]. Similar results are observed by Huddleston et al., in right lung lobectomy or pneumonectomy compared to repair of the anomalous venous return and ligation of collaterals [19]. Post repair stenosis is the most important immediate postoperative complication which may lead to death in certain cases. The risk of thrombosis is also there.
Conclusion
In conclusion, we describe a rare congenital anomaly, the scimitar syndrome, which is complicated by an atrial septal defect. This case report emphasizes the importance of a thorough clinical evaluation. Through CT and MRI the exact anatomy of the anomalous drainage and course of adjacent vessels should be delineated.
References
- Neill, Catherine A., et al. "The familial occurrence of hypoplastic right lung with systemic arterial supply and venous drainage" scimitar syndrome"." Bulletin of the Johns Hopkins Hospital, Vol. 107, 1960, pp. 1-21.
- Woodring, John H., Teresa A. Howard, and Jamshed F. Kanga. "Congenital pulmonary venolobar syndrome revisited." Radiographics, Vol. 14, No. 2, 1994, pp. 349-69.
- Frydrychowicz, A., et al. "Images in cardiovascular medicine. Scimitar syndrome: added value by isotropic flow-sensitive four-dimensional magnetic resonance imaging with PC-VIPR (phase-contrast vastly undersampled isotropic projection reconstruction)." Circulation, Vol. 121, No. 23, 2010, pp. e434-6.
- Cahssinat, R. "Observation of remarkable anatomical abnormalities of the circulatory system with hepatocele renital discharge which gave rise during life to no particular symptoms." Archives of General Medicine Paris, Vol. 11, 1836, pp. 80.
- Canter, Charles E., et al. "Scimitar syndrome in childhood." The American Journal of Cardiology, Vol. 58, No. 7, 1986, pp. 652-4.
- Oakley, D., et al. "Scimitar vein syndrome: report of nine new cases." American Heart Journal, Vol. 107, No. 3, 1984, pp. 596-8.
- Shibuya, Kazuhiko, Jeffrey E. Smallhorn, and Brian W. McCrindle. "Echocardiographic clues and accuracy in the diagnosis of scimitar syndrome." Journal of the American Society of Echocardiography, Vol. 9, No. 2, 1996, pp. 174-81.
- Schramel, F. M., et al. "The scimitar syndrome: clinical spectrum and surgical treatment." European Respiratory Journal, Vol. 8, No. 2, 1995, pp. 196-201.
- Dupuis, Claude, et al. "The “adult” form of the scimitar syndrome." The American Journal of Cardiology, Vol. 70, No. 4, 1992, pp. 502-7.
- Gao, Yong-An, et al. "Scimitar syndrome in infancy." Journal of the American College of Cardiology, Vol. 22, No. 3, 1993, pp. 873-82.
- Valsangiacomo, E. R., et al. "Partial and total anomalous pulmonary venous connection in the fetus: two-dimensional and Doppler echocardiographic findings." Ultrasound in Obstetrics and Gynecology, Vol. 22, No. 3, 2003, pp. 257-63.
- Carvalho, J. S., et al. "ISUOG practice guidelines (updated): sonographic screening examination of the fetal heart." Ultrasound in Obstetrics and Gynecology, Vol. 41, 2013, pp. 348-59.
- SIEOG (Italian Society of OStetric-Gynecological Ultrasound). `SIEOG Guidelines (2015 Edition). Editeam, Cento (FE): Rome, 2015.
- Kamler, Markus, et al. "Scimitar syndrome in an adult: diagnosis and surgical treatment." Interactive Cardiovascular and Thoracic Surgery, Vol. 2, No. 3, 2003, pp. 350-1.
- Pelletier, Glenn J., and Thomas L. Spray. "Repair of Scimitar syndrome." Operative Techniques in Thoracic and Cardiovascular Surgery, Vol. 6, No. 1, 2001, pp. 32-49.
- Gudjonsson, Ulf, and John W. Brown. "Scimitar syndrome." Seminars in Thoracic and Cardiovascular Surgery: Pediatric Cardiac Surgery Annual, Vol. 9, No. 1, WB Saunders, 2006.
- Casha, AR, M. Sulaiman, and A. J. R. Cale. "Repair of adult Scimitar syndrome with an intra-atrial conduit." Interactive Cardiovascular and Thoracic Surgery, Vol. 2, No. 2, 2003, pp. 128-30.
- Puig-Massana, M., M. Murtra, and J. M. Revuelta. "A new technique in the correction of partial anomalous pulmonary venous drainage." The Journal of Thoracic and Cardiovascular Surgery, Vol. 64, No. 1, 1972, pp. 108-13.
- Huddleston, Charles B., et al. "Scimitar syndrome presenting in infancy." The Annals of Thoracic Surgery, Vol. 67, No. 1, 1999, pp. 154-9.