Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 3
Study of Heart Rate Variability among Normal and Overweight Individuals during Pre-and Post-Exercise Period
Athira Surendran1* and Shreesh Ajaykumar22Department of Civil Engineering, Government College of Engineering, Kannur, India
Athira Surendran, Department of Physiology, Mysore Medical College and Research Institute Mysore, Karnataka, India, Email: athiram1171@gmail.com
Received: 02-Feb-2022, Manuscript No. ijmrhs-22-53212 (M); Editor assigned: 04-Feb-2022, Pre QC No. ijmrhs-22-53212 (P); Reviewed: 22-Feb-2022, QC No. ijmrhs-22-53212 (Q); Revised: 07-Mar-2022, Manuscript No. ijmrhs-22-53212 (R); Published: 15-Mar-2022
Abstract
Background: Sympathetic activity in obesity-related cardiovascular diseases indicates the association between cardiac autonomic functions and BMI (Body Mass Index). The Heart Rate Variability (HRV) is considered as an appropriate measure of cardiac autonomic function. A stressor, like an exercise, requires changes in the neural, cardiovascular and autonomic control that are unique to the person. So the study was conducted to assess the heart rate variability of normal and overweight individuals during the pre-and post-exercise period. Methods: A case-control study with 42 subjects of 17-25 years old was done. Subject with their BMI ≥ 25 kg/m2 (overweight) was taken as cases and their BMI within normal limits (18.5 kg/m2-24.9 kg/m2) was taken as controls. Resting HRV was recorded. Then, the subjects were asked to perform Harvard Step Test and the post-exercise HRV was recorded immediately. Results: At rest, the values of HRV domains like High Frequency (HF) and RMSSD and pNN50 (Indicators of parasympathetic activity) were less and the Low Frequency (LF) and LF/HF (Indicators of sympathetic activity) were high in an overweight group compared to control. After exercise, the difference in the HRV variables became more prominent and LF/HF became significant for the overweight group compared to the control group. Correlation between HRV variables and BMI remained almost the same both in pre-and post-exercise. Conclusion: Overweight individuals have their HRV indices indicative of dominant cardiac sympathetic activity and reduced parasympathetic activity in response to simple aerobic exercise compared to individuals with normal BMI. Hence, it is likely that overweight individuals are prone to develop various cardiovascular diseases in their future life.
Keywords
Exercise, HRV, Overweight
Introduction
Modern lifestyle imposes various challenges to the homeostasis of the body, the major challenges being less physical activity and a stressful work environment. These factors lead to disturbed metabolic activity leading to overweight and obesity. The incidence of obesity in young adults in India now has been identified as one of the biggest precursors of many non-communicable diseases adversely affecting the cardiovascular health of the individual. It also increases the risk of diabetes mellitus and metabolic syndrome. WHO now accepts a Body Mass Index (BMI) of 25.0 kg/ m2 or higher as abnormal and the overweight category is classified as obese when the BMI is 30.0 kg/m2 or more [1,2].
Autonomic function has been largely focused on obesity, fuelled by either the putative involvement of enhanced sympathetic activity in obesity-related cardiovascular disease or the possible role of reduced sympathetic activity in the genesis of obesity [3].
The association between the overweight/obese condition and changes in the activity of the Autonomic Nervous System (ANS) is widely accepted [4-6]. In particular, it is known that the ANS influences physiological time variation between heartbeats. Hence, the Heart Rate Variability (HRV) is considered an appropriate measure of the cardiac autonomic function although its interpretation is to date controversial [7-9].
Physical exercise requires rapid and complex physiological adaptation, particularly by the ANS. Exercise programs require changes in the neural cardiovascular and ANS control that are unique to the person and his/her surroundings [10]. So there may be changes in the post-exercise cardiac autonomic response of individuals with normal and high BMI.
The purpose of this study is to assess the heart rate variability of normal and overweight individuals during pre and post-exercise periods. The study also analyses the degree and nature of the relationship between BMI and HRV indices.
Aim
To compare the cardiac autonomic functions of normal and overweight individuals.
Objectives of the Study
• To record the HRV during pre and post-exercise period on subjects with normal BMI and who are under the overweight category
• To compare the pre-exercise HRV on normal and overweight individuals
• To compare the post-exercise HRV on normal and overweight individuals
• To assess the effect of BMI on HRV in normal and overweight individuals during pre and post-exercise period
Materials and Methods
Study Subjects
42 subjects of age 17 to 25 years were included in the study with 20 males and 22 females.
Sample Size Calculation
2 sided confidence interval=95%
Power=80%, Ratio of sample size (group 2/group 1) =1
Group 1 mean=67.64, SD=30.61, Variance=936.9
Group 2 mean=43.85, SD=23.93, Variance=576.6
Sample size of group 1=21, Sample size of group 2=21
Study Design
Case-control study.
Inclusion Criteria
Study group: Subjects with their BMI more than or equal to 25 kg/m2 (overweight category)
Control group: Subjects with their BMI within normal limits (18.5 kg/m2-24.9 kg/m2)
Exclusion Criteria for Study Group and Control Group
- Any subject with hypertension/diabetes mellitus/respiratory diseases/cardiovascular disease any other disease history which may affect their autonomic function
- History of Asthma, COPD, Anemia
- Subjects who cannot perform exercise due to physical disabilities
- History of any neurological or psychological disorder
- Habits of smoking, alcohol consumption
Study Period
3 months.
Method
Informed consent was obtained from each subject before the study. The subjects were divided into two groups based on their BMI: Group-1 or control group (BMI between 18.5-24.99; n=21) and Group-2 or Overweight group/High BMI group (BMI ≥ 25; n=21). A detailed medical history of all the subjects was also taken to meet the inclusion and exclusion criteria. Approval was obtained from the Ethical Committee of the institution.
The study was conducted under the standard laboratory conditions (temperature 26 ± 2°C). After assessment of general health and history of any illnesses, the height and weight of the selected subjects were recorded for measurement of BMI (kg/m2).
After a rest for fifteen minutes, resting ECG (for Lead II) recording was done for at least 10 minutes in supine posture. The ECG signals were obtained with the help of an electronic data acquisition system using a Digital polygraph.
The digitalized ECG signals were analyzed with Kubios software. HRV module analyses beat-to-beat interval variation in ECG recordings by detecting the R waves from each ECG waveform and generating an R-R interval tachogram. Then, power spectral density was determined by Fast Fourier Transformation of interval tachogram. HRV analysis includes time and frequency domain indices. Time-domain indices in milliseconds include RMSSD-square root of the mean of the sum of the squares of differences between adjacent NN intervals, pNN50(%)-the percentage of the difference between adjacent NN intervals that are greater than 50 ms. Frequency domain indices include LF (Low Frequency) power, HF (High Frequency) power. The LF and HF are expressed in a ‘normalized unit’ (nu) in our study [9].
Then, the subjects were asked to perform Harvard Step Test, and immediately after the exercise, ECG was recorded for the next 15 minutes. However, only the first 5 minutes of recovery ECG data were considered for the study.
Protocol for Harvard Step Test (HST)
Subjects were asked to perform standard HST by alternately stepping up and down on a 16 inch high stool at a rate of 40 steps/minute for a maximum of five minutes or till complete fatigue, whichever occurs earlier [11].
Statistical Analysis
Mean ± SD of HRV parameters for both control and overweight groups in resting and post-exercise period were determined. Comparison between groups was done using a 2-tailed Mann-Whitney U-nonparametric test. Whereas, Spearman’s Correlation test was used to assess the correlation between BMI and HRV parameters for each group. A p-value of less than 0.05 was considered statistically significant.
Results
Adult healthy male subjects between the age group of 17-25 years (n=42) who met all the inclusion and exclusion criteria were divided into two groups: Group 1 (control) with BMI between 18.5-24.99 and Group 2 (overweight) with BMI ≥ 25.
i. Physical Characteristics
The average BMI of Group 1was 20.99 ± 1.56 and Group 2 was 26.42 ± 1.04 which was found to be significantly different (p<0.05).
ii. At Rest
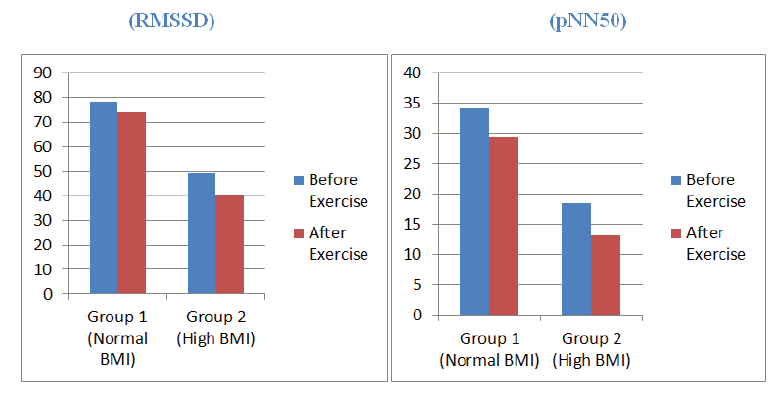
a) HRV indices: The time-domain measures, RMSSD and pNN50 were 78.11 ± 20.6 ms and 34.18 ± 19.97% respectively for the normal BMI subjects which were significantly higher (p<0.05) than overweight individuals (RMSSD 49.23 ± 18.87 ms and pNN50 18.51 ± 9.13%) (Table 1 and Figure 1).
| HRV Indices | Group 1 (Normal BMI) | Group 2 (High BMI) | p-value |
|---|---|---|---|
| RMSSD (ms) | 78.11 ± 20.6 | 49.23 ± 18.87 | 0.00001* |
| pNN50 (%) | 34.18 ± 19.97 | 18.51 ± 9.13 | 0.016* |
| LF (nu) | 39.48 ± 9.36 | 40.81 ± 6.7 | 0.548 |
| HF (nu) | 56.84 ± 13.1 | 55.73 ± 9.84 | 0.503 |
| LF/HF | 0.71 | 0.74 | 0.38 |
| *p<0.05 considered as significant | |||
b) HRV indices: The frequency domain measures, No significant difference was detected between the control and overweight group in terms of their HF and LF or LF/HF. However, both LF (40.81 ± 6.7 nu) and LF/HF (0.74) were higher and HF (55.73 ± 9.84 nu) was lower in the case of high BMI subjects (Table 1).
c) Correlation between BMI and HRV indices: All-time domain indices (RMSSD, pNN50) of control subjects were found to have a negative correlation with BMI, and also LF and HF showed negative correlation but LF/ HF exhibited a positive correlation with BMI. In high BMI subjects; RMSSD, LF, and LF/HF had a negative correlation with BMI but pNN50 and HF had a positive correlation. However, this correlation trend was not found to be statistically significant for any of the parameters (Table 2 and Table 3)
| Variables | Resting/BMI | Post Exercise/BMI | |
|---|---|---|---|
| RMSSD (ms) | Rho | -0.15 | -0.165 |
| p-value | 0.516 | 0.475 | |
| pNN50 (%) | Rho | -0.365 | -0.434 |
| p-value | 0.103 | 0.05 | |
| LF (nu) | Rho | -0.119 | -0.004 |
| p-value | 0.606 | 0.987 | |
| HF (nu) | Rho | -0.109 | -0.088 |
| p-value | 0.636 | 0.703 | |
| LF/HF | Rho | 0.006 | 0.186 |
| p-value | 0.978 | 0.420 | |
| Variables | Resting/BMI | Post Exercise/BMI | |
|---|---|---|---|
| RMSSD (ms) | Rho | -0.245 | -0.251 |
| p-value | 0.284 | 0.272 | |
| pNN50 (%) | Rho | 0.191 | 0.289 |
| p-value | 0.406 | 0.204 | |
| LF (nu) | Rho | -0.039 | 0.009 |
| p-value | 0.868 | 0.966 | |
| HF (nu) | Rho | 0.075 | 0.053 |
| p-value | 0.747 | 0.818 | |
| LF/HF | Rho | -0.329 | -0.211 |
| p-value | 0.145 | 0.358 | |
iii. Post Exercise Recovery
a) HRV indices: The time-domain measures: Both RMSSD and pNN50 were significantly lower for high BMI subjects than the normal BMI group as it was in the pre-exercise time (Table 4).
| HRV Indices | Group 1 (Normal BMI) | Group 2 (High BMI ) | p-value |
|---|---|---|---|
| RMSSD (ms) | 74.03 ± 18.57 | 40.59 ± 16.08 | 0.00001* |
| pNN50 (%) | 29.43 ± 17.53 | 13.17 ± 6.2 | 0.002* |
| LF (nu) | 43.41 ± 9.34 | 47.41 ± 10.51 | 0.069 |
| HF (nu) | 51.95 ± 12.29 | 44.31 ± 13.49 | 0.208 |
| LF/HF | 0.17 | 1.1 | 0.004* |
| *p<0.05 considered as significant | |||
b) HRV indices: The frequency domain measures; as in pre-exercise, HF was lower and LF, LF/HF was higher in high BMI subjects but the LF/HF ratio was significantly higher than normal BMI subjects (Table 4, and Figure 1).
c) Correlation between BMI and HRV indices: Individuals with normal BMI had no change in the correlation pattern during recovery with the entire pattern remaining the same as that of the resting state. Individuals with high BMI also had the same correlation pattern except for LF which had a positive correlation with BMI after exercise (Table 2, and Table 3).
Discussion
In the HRV measurement, the HF component (0.15 Hz to 0.40 Hz) is an indicator of vagal (parasympathetic) activity as observed during various autonomic challenges e.g. electrical stimulation, muscarinic receptor blockade, and vagotomy [9]. Interpreting LF (0.04 Hz to 0.15 Hz) component, on the other hand, is controversial. Earlier it was believed to be a marker of sympathetic tone but is now known to include both sympathetic and vagal modulation and has been associated with baroreflex activity [12].
The time-domain measures, RMSSD and pNN50, are closely linked to the HF component and therefore, are known to be an indicator of parasympathetic activity being linked with cardiac vagal status [13].
In the present study during the resting state, the values of all the time domain measures (significant) and HF were less and the LF and LF/HF ratio were high in an overweight group compared to the control group. It indicates the presence of an early altered state of sympathovagal balance with a predominance of sympathetic tone in the overweight group.
Guizar JM, et al. also has shown in their study that obese adolescents present with reduced parasympathetic and greater sympathetic modulation of the cardiac system [14].
A study conducted by Koenig, et al. conclude that sympathovagal balance is related to BMI in non-obese, healthy individuals, providing evidence for a prominent role of the vagus nerve in the modulation of the energy expenditure of the human organism [15].
After exercise, the values of RMSSD, pNN50, HF were further reduced for the over-weight group and differed significantly from normal BMI subjects. Also the value of LF, LF/HF ratio had increased and the LF/HF ratio became significant for the overweight group compared to the control group. It shows that there is more pronounced sympathetic activity and decreased parasympathetic activity after a stressor like an exercise in the overweight group.
Our results are similar to the study by Latha Ramalingam, et al. where they conclude that overweight and obese females have a prolonged increase in HR and HRV indices indicative of dominant cardiac sympathetic activity in response to simple aerobic exercise compared to the control group [16].
When we consider the correlation between HRV variables and BMI in the control group, there exists a negative correlation between BMI and RMSSD, pNN50, HF, LF. While there is a positive correlation with LF/HF, it implies that the subjects with less BMI have a parasympathetic predominance. After exercise, the correlation patterns remained the same.
The correlation between HRV variables and BMI in the overweight group shows an inconclusive result. RMSSD, LF, and LF/HF had a negative correlation with BMI but pNN50 and HF had a positive correlation. After exercise, the correlation patterns remained the same except for LF which showed a positive correlation with BMI.
Though we did not find any significant correlation of BMI with HRV indices, control group subjects exhibited a negative correlation with all the parasympathetic measures (RMSSD, pNN50, and HF) and positive correlation with sympathetic indicators i.e. LF/HF. LF showed a positive correlation. This indicates that increasing BMI coincides with a reduced parasympathetic and increased sympathetic tone.
There is a study by Rajalingamgari, et al. where they get an exactly opposite result from our study [17]. They observed an inhibited autonomic response and thereby caused reduced HRV in overweight (pre-obese) individuals in response to even simple and mild to moderate degrees of exercise like the Harvard Step Test when compared to the control group [17]. So we need further studies with more number of subjects for clarification.
Conclusion
A sedentary lifestyle has become common in the present generation due to the fast and competitive world which has led to an increased incidence of obesity and many other lifestyles related disorders in the population.
Our study results have shown that the overweight individuals have HRV indices indicative of dominant cardiac sympathetic activity and reduced parasympathetic activity in response to simple aerobic exercise compared to individuals with normal BMI. Hence, it is likely that these individuals are prone to develop hypertension and other cardiac complications in their future life. Hence, the practice of regular physical activities which aim at reducing body weight must be encouraged among these young females to avoid various health hazards in the future.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
REFERENCES
- Bleich, Sara N., et al. "Why is the developed world obese?" Annual Review of Public Health, Vol. 29, 2008, pp. 273-95.
Google Scholar Crossref - Dw, Haslam. "Obesity." Lancet, Vol. 366, No. 9492, 2005, pp. 1197-209.
Google Scholar Crossref - Triggiani, Antonio Ivano, et al. "Heart rate variability is reduced in underweight and overweight healthy adult women." Clinical Physiology and Functional Imaging, Vol. 37, No. 2, 2017, pp. 162-67.
Google Scholar Crossref - Millis, Richard M., et al. "Association of body fat percentage and heart rate variability measures of sympathovagal balance." Life Sciences, Vol. 86, No. 5-6, 2010, pp. 153-57.
Google Scholar Crossref - Davy, Kevin P., and Jeb S. Orr. "Sympathetic nervous system behavior in human obesity." Neuroscience & Biobehavioral Reviews, Vol. 33, No. 2, 2009, pp. 116-24.
Google Scholar Crossref - Grassi, Guido, et al. "Sympathetic activation in obese normotensive subjects." Hypertension, Vol. 25, No. 4, 1995, pp. 560-63.
Google Scholar Crossref - Laborde, Sylvain, Emma Mosley, and Julian F. Thayer. "Heart rate variability and cardiac vagal tone in psychophysiological research-recommendations for experiment planning, data analysis, and data reporting." Frontiers in Psychology, Vol. 8, 2017, p. 213.
Google Scholar Crossref - Shaffer, Fred, and Jay P. Ginsberg. "An overview of heart rate variability metrics and norms." Frontiers in Public Health, 2017, p. 258.
Google Scholar Crossref - Task Force of the European Society of Cardiology. "Heart rate variability: Standards of measurement, physiological interpretation and clinical use." Circulation, Vol. 93, 1996, pp. 1043-65.
Google Scholar Crossref - Grant, Catharina Cornelia, and James A. Ker. "Autonomic response to exercise as measured by cardiovascular variability." South African Journal of Sports Medicine, Vol. 20, No. 4, 2008, pp. 102-08.
Google Scholar Crossref - Ghai, C. L. "Cardiac efficiency tests: II Harvard step test." A Textbook of Practical Physiology, Vol. 186, 2013.
Google Scholar Crossref - Billman, George E. "The LF/HF ratio does not accurately measure cardiac sympatho-vagal balance." Frontiers in Physiology, Vol. 4, 2013, p. 26.
Google Scholar Crossref - Barrett, K. E., et al. "Cardiovascular regulatory mechanisms." Ganong's Review of Medical Physiology. 23rd Ed. New Delhi, Tata McGraw-Hill Companies, 2010, pp. 555-68.
Google Scholar Crossref - Guizar, J., et al. "Heart autonomic function in overweight adolescents." Indian Pediatrics, Vol. 42, No. 5, 2005, pp. 464-69.
Google Scholar Crossref - Koenig, Julian, et al. "Body mass index is related to autonomic nervous system activity as measured by heart rate variability-A replication using short term measurements." The Journal of Nutrition, Health & Aging, Vol. 18, No. 3, 2014, pp. 300-02.
Google Scholar Crossref - Ramalingam, Latha, and Rajalakshmi Ramesh. "Effect of aerobic exercise as a stressor on the cardiac autonomic status of young sedentary overweight and obese females." National Journal of Physiology, Pharmacy and Pharmacology, Vol. 7, No. 3, 2017, pp. 311-16.
Google Scholar Crossref - Prasad, Rajalingamgari Venkata Mallikarjuna Vara, et al. "Resting and post exercise Heart Rate Variability in preobese individuals: A comparative study." Asian Journal of Medical Sciences, Vol. 9, No. 4, 2018, pp. 23-30.
Google Scholar Crossref