Research Article - International Journal of Medical Research & Health Sciences ( 2025) Volume 14, Issue 3
Study on Clinical and Bacteriological Profile of Acute Tonsillitis
Kolaj Kattel1*, Akriti Shrestha1, Indra Upadhyay2 and Prasansa Basnet22Department of Otorhinolaryngology, Chitwan Medical College Teaching Hospital, Bharatpur, Nepal
Kolaj Kattel, Department of Otorhinolaryngology, Nobel Medical College Teaching Hospital, Biratnagar, Nepal, Email: kolaj.kattel23@gmail.com
Received: 09-Apr-0004, Manuscript No. IJMRHS-24-131904; Editor assigned: 12-Apr-2024, Pre QC No. IJMRHS-24-131904 (PQ); Reviewed: 27-Apr-2024, QC No. IJMRHS-24-131904; Revised: 29-May-2025, Manuscript No. IJMRHS-24-131904 (R); Published: 05-Jun-2025
Abstract
Introduction: Tonsillitis is a frequent condition noticed in the ENT department of every hospital one out of every 10 children visiting the ENT OPD, suffer from acute tonsillitis. Identification of the organisms responsible and their antibiotic sensitivity pattern can guide in early and timely oral antibiotics and preventing wasting hours of work in hospital stay. This study was done to have an insight into various pathogens that are the cause of acute tonsillitis and evaluating their antibiotic susceptibility.
Methods: A descriptive study cross sectional study conducted between January 2018 and January 2019 in a tertiary care center after obtaining ethical approval (Reference number- 222/2018). Patients of age group 5-50 years with acute tonsillitis, who had not taken antibiotics prior to hospital visit, were included. Convenience sampling was done. Collected data were entered in microsoft excel and analyzed using statistical package for social sciences version 24.0.
Results: GABHS (50%) was the predominant pathogen followed by Staphylococcus aureus (20.8%). Maximum sensitivity amongst the isolated organism was observed with Linezolid (77.1%) and Vancomycin (72.9%), while maximum resistance was observed for gentamycin (79.2%) ciprofloxacin (62.5%). The maximum isolated organism GABHS was mostly sensitive to frequently used antimicrobials for acute tonsillitis like amoxicillin +clavulanate (75%), ampicillin (79.1%), cefixime (62.5%) and ceftriaxone (70.8%).
Conclusion: In this study GABHS was found to be the most common offending pathogen. This study also suggests amoxicillin+clavulanate or ampicillin is still a good choice of initial empirical therapy until the arrival of throat swab culture sensitivity reports.
Keywords
Acute tonsillitis, Throat swab, Culture and sensitivity, GABHS
Introduction
Background
Developing at 8 weeks from 2nd pouch (ventral and dorsal). The palatine tonsils which are a component of Waldeyer’s ring, a circumferential array of secondary lymphoid tissue in the oropharynx that provides immunologic surveillance and produces immunoglobin are located in the lateral aspect of the oropharynx, in a fossa bound by two pillars of pharyngeal muscle, the palatopharyngeus posteriorly and the palatoglossus anteriorly [1].
Epidemiology
Tonsillitis is a frequent condition noticed in the ENT department of every hospital one out of every 10 children visiting the ENT OPD, suffer from acute tonsillitis [2].
Pathophysiology
It is inflammation of the pharyngeal tonsils. It occurs when the trapped organisms infiltrate the mucosal barrier and attribute themselves to the epithelial cells, leading to cytokine production and complement activation. These series of reactions produce an inflammatory reaction in the tonsillar mucosa [3].
Clinical features
The clinical presentation of acute tonsillitis varies based on etiology, most commonly presenting with fever, odynophagia, dysphagia and tonsillar erythema. Bacteria cause tonsillitis more frequently in older children and adults than in young children. Staphylococcus aureus and Streptococcus pyogenes are the most common bacteria that cause tonsillitis. Hemophilus influenzae is also a frequent cause of tonsil infection [4].
Current treatment and limitations
Presently, penicillin treatment of tonsillo-pharyngitis does not meet the minimum United States food and drug administration standards for first line treatment, which is 85% or greater eradication at the end of therapy. Recent results with amoxicillin suggest its efficacy is also waning. Cephalosporins alone or cephalosporins with metronidazole where anaerobes are implicated have the highest bacteriologic and clinical efficacy [5].
Rationale of study
Antibiotic sensitivity testing is a simple technique that demonstrates the susceptibility or resistance of various microorganisms to the antibiotics tested. This is useful in guiding the physician’s choice of antibiotics by revealing the changing trends in susceptibility [6].
Hence, our aim was to study the antibiotic sensitivity pattern of the offending pathogen that would indicate the optimum line of treatment in terms of preventing antibiotic resistance, complications and avoiding unnecessary surgery [7].
Materials and Methods
Study design: Descriptive cross-sectional study
After obtaining ethical approval (Reference number-222/2018) Thisa descriptive cross-sectional study was conducted between January 2018 and January 2019 in the department of Otorhinolaryngology of Nobel medical college teaching hospital and research centre, Biratnagar, Nepal [8].
Inclusion criteria:
• Patients of age group 5-50 years presenting with sore throat who had a modified center score of >=2 points
Modified centor criteria:
Age<15-1 point
Tonsillar exudates or swelling-1 point
Tender Anterior cervical lymphadenopathy-1point
Fever>100.4 Fahrenheit-1point
No cough-1 point
• Patients who had not taken antibiotics prior to hospital visit
Exclusion criteria:
• Patients on antibiotic prior to hospital visit were excluded.
• Patients with immunocompromised state, HIV/AIDS, diabetes and under steroid medication were excluded.
Study place: Department of otorhinolaryngology, Nobel medical college teaching Hospital, Biratnagar.
Duration of study: 1 year (January 2019-December 2019).
Sample size: Since the calculated sample size calculated was too large for the study, corrected sample size was calculated after checking the hospital records for the number of cases of acute tonsillitis presenting to the department of ENT who did not take medication prior to hospital visit which is estimated roughly to be 50 [9].
Therefore, the corrected sample size was found to be 48 which is calculated using the formula:
Intervention details: Cases were selected by randomization and were subjected to thorough history and clinical examination. The selected patients then underwent routine investigations and throat swab culture and sensitivity before starting treatment with antibiotics. Data entry was done about the clinical and bacteriological profile of patients based on clinical assessment and culture sensitivity reports [10].
Consent
Informed and written consent was signed and obtained from patients prior to study.
Statistical analysis
After collecting, the data were verified and coded accordingly and entered in Microsoft excel and converted into Statistical Package for Social Science V.24.0 (SPSS V.24) for statistical analysis. Obtained data were expressed in frequency, percentage for qualitative data and mean, standard deviation and median as applicable for qualitative data as descriptive statistics.
Results
A total of 48 patients with Acute Tonsillitis were studied. 56% of those were male and 44% were female. Majority of patients were from age group 16-30 years (70.8%). 81% belonged to middle class family. Student constituted majority (47.9%) of the total study group. Commonest symptom among the patient studied was fever (70.8%) and dysphagia (70.8%). Enlarged and tender jugulodigastric lymph node was the commonest sign which was present in 89.6% of the patients. Among the throat swab culture and sensitivity tests performed 85.4% yielded pathogenic organism, rest were negative. GABHS (50%) was the predominant pathogen followed by Staphylococcus Aureus (20.8%). Streptococcus pneumonia was isolated in 6.3%, H. Influenza in 4.2% and 2.1% of isolates had E. coli and Klebsiella pneumonia each. Maximum sensitivity amongst the isolated organism was observed with linezolid (77.1%) and vancomycin (72.9%). While maximum resistance was observed for gentamycin (79.2%) ciprofloxacin (62.5%). The maximum isolated organism GABHS was mostly sensitive to frequently used antimicrobials for acute tonsillitis like amoxicillin+clavulanate (75%), ampicillin (79.1%), cefixime (62.5%) and ceftriaxone (70.8%) while the less frequently used antibiotics like vancomycin and linezolid were highly sensitive accounting for 95.8% and 100% sensitivity respectively. clindamycin was also equally sensitive for GABHS as amoxicillin+clavulanate i.e., 75% (Figures 1 and 2) (Tables 1-3) [11].
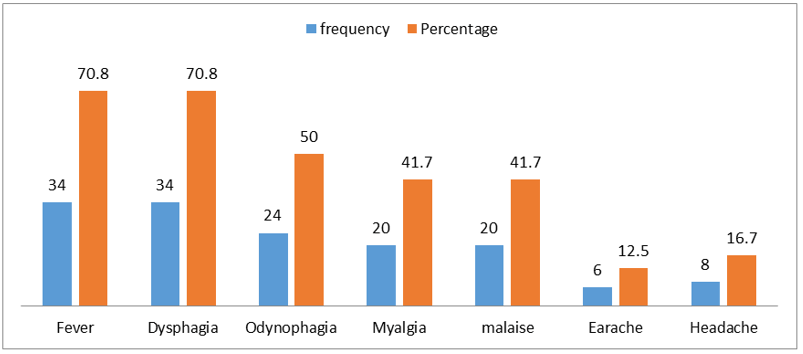
Figure 1 Symptoms of patients
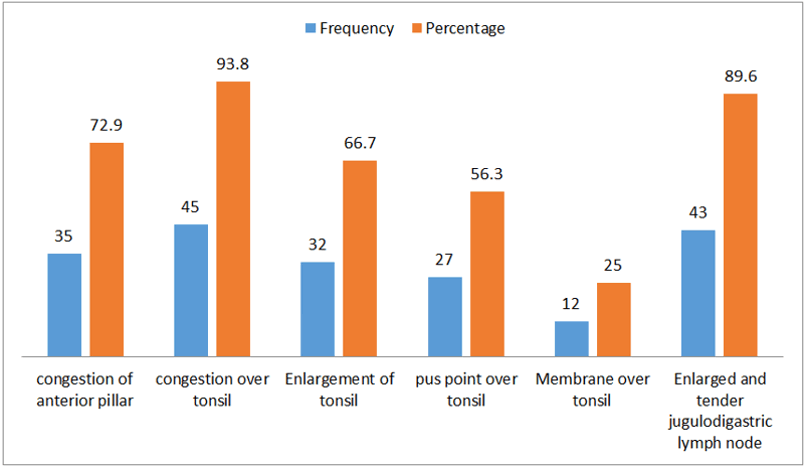
Figure 2 Signs of patients
| Isolated organism | Frequency | Percent |
| E. coli | 1 | 2.1 |
| GABHS | 24 | 50 |
| H. influenza | 2 | 4.2 |
| Klebsiella pneumonia | 1 | 2.1 |
| Staph. aureus | 10 | 20.8 |
| Streptococcus pneumonia | 3 | 6.3 |
| Negative | 7 | 14.6 |
| Total | 48 | 100 |
Table 1 Organisms isolated from throat swab culture and sensitivity
| S. no | Antibiotics | Sensitive frequency | Sensitive percentage | Resistant frequency | Resistant percentage |
| 1 | Penicillin | 19 | 39.6 | 22 | 45.8 |
| 2 | Methicillin | 26 | 54.2 | 15 | 31.3 |
| 3 | Amoxi-clav | 29 | 60.4 | 12 | 25 |
| 4 | Ampicillin | 30 | 62.5 | 11 | 22.9 |
| 5 | Cefuroxime | 22 | 45.8 | 19 | 39.6 |
| 6 | Cefexime | 27 | 56.3 | 14 | 29.2 |
| 7 | Ceftriaxone | 29 | 60.4 | 12 | 25 |
| 8 | Ciprofloxacin | 11 | 22.9 | 30 | 62.5 |
| 9 | Clindamycin | 26 | 54.2 | 15 | 31.3 |
| 10 | Vancomycin | 35 | 72.9 | 6 | 12.5 |
| 11 | Gentamycin | 3 | 6.3 | 38 | 79.2 |
| 12 | Linezolid | 37 | 77.1 | 4 | 8.3 |
| 13 | Cotrimoxazole | 15 | 31.3 | 26 | 54.2 |
| 14 | Erythromycin | 28 | 58.3 | 13 | 27.1 |
Table 2 Overall antibiotic sensitivity pattern
Table 3 Antibiotic sensitivity pattern by organism isolated
Discussion
Diagnosis and treatment of acute tonsillitis continues to account for a significant financial expenditure annually. The impact of infection from tonsillar disease, especially on the health may not be localized just to the tonsil alone. Major ill effects on the related anatomic structures of the nose and paranasal sinus, the upper aerodigestive tract and Eustachian tube middle ear complex is well established. Thus understanding the classification, pathophysiology, evaluation and treatment of disease process encountered in the tonsil is not only important but also to a great deal of practical benefits to the practicing otolaryngologist [12].
Age: Maximum numbers of patients were in the age group 16-30 years, which is in accordance with Abhilash A M and Bista, et al. and Cherian, et al., all of whom noted highest frequency of acute tonsillitis 20-29-year age group while Simla, et al., had majority of the patients in the age group of 5-14 years (40.32%).
Sex ratio: Majority of the patients were males (56%) as compared to females (44%) in this study which was the similar to studies conducted by various authors [13].
Socio-economic status: In our study, it was observed that 81% of the studied population belonged to the middle-class family whilst lower class and upper class constituted 15% and 4% respectively as opposed to study done by Vijayashree, et al. where it was observed that 61% of the cases were in low-income group, 35% in middle income group [14].
Occupation: Students constituted majority (47.9%) of the total study group followed by housewife (20.8%), banker (10.4%), farmer (8.3%), teacher (6.3%) and driver (2.1%) in decreasing order of frequency. Students (70 %) comprised the maximum percentage in other similar study done by Vijayashree, et al.
Symptoms: Fever (70.8%) and dysphagia (70.8%) was commonest symptom among the patient studied. Other symptoms like odynophagia, myalgia, malaise, earache and headache accounted for 50%, 41.7%, 41.7%, 12.5% and16.7% respectively. In a study conducted by Vijayashree, et al., the commonest symptoms in all patients were sore throat whilst the other symptoms like fever, odynophagia and constitutional symptoms were 73%, 36% and 45% respectively. In study done by Abhilash A M and Cherian, et al. the commonest symptoms was sore throat and fever, the former accounted for 85.1% of the total observed patients and the latter 62.3% [15].
Signs: On clinical examination in this study, enlarged and tender jugulodigastric lymph node was the commonest sign which was present in 89.6% of the patients under observation. Congestion of anterior pillar, congestion of tonsil, enlargement of tonsil, pus point over tonsil and membrane over tonsil was present in 72.9%, 93.8%, 66.7%, 56.3% and 25% respectively. The study conducted by Vijayashree, et al noted palpable digastric lymph node in 70% of the cases studied.19 Simla, et al., in their study found congested pillars in all patients and tender jugulodigastric lymph node in 79.03%.18 The study conducted by Abhilash A M and Cherian, et al., also showed enlarged tonsils in 80.6% of the patients and follicles on the congested surface of one or both tonsil in 94.4% [16].
Organism isolated: In this study GABHS (50%) was the predominant pathogen followed by Staphylococcus aureus (20.8%). Streptococcus pneumonia was isolated in 6.3%, H. Influenza in 4.2% and 2.1% of isolates had E. coli and klebsiella pneumonia each. 14.6% of the samples had no yield [17].
Simla, et al. and Vijayashree, et al., found β-hemolytic Streptococci in 51.4% and 62.16% respectively. Similarly, Ba Saddik, et al., findings of 41.5% group a beta hemolytic Streptococcus is also consistent with our study.
While Abhilash AM and Cherian, et al., showed that Streptococcus was the commonest species identified, the majority being alpha hemolytic streptococci, Mahajan GD, Ingale M found Staphylococcus aureus as the commonest organism [18].
Fahad HM showed the frequency of Streptococcus species as 88.6%. 9 While Bista, et al. identified Streptococcus viridans (40.625%) with Beta hemolytic streptococci constituting 21.875% of the total isolates [19].
Babaiwa, et al. and Wang et al found Staphylococcus aureus as the highest occurring organism 32.6% and 70% respectively.
The finding of a study done by Evans AS, Dick EC concluded the presence of hemolytic streptococci with a frequency of 33.8%.
Antibiotic sensitivity pattern
In our study, maximum sensitivity amongst the isolated organism was observed with linezolid (77.1%) and vancomycin (72.9%). While maximum resistance was observed for gentamycin (79.2%) ciprofloxacin (62.5%). The maximum isolated organism GABHS was mostly sensitive to frequently used antimicrobials for acute tonsillitis like amoxicillin+clavulanate (75%), ampicillin (79.1%), cefixime (62.5%) and ceftriaxone (70.8%) while the less frequently used antibiotics like Vancomycin and linezolid were highly sensitive accounting for 95.8 % and 100 % sensitivity respectively. Clindamycin was also equally sensitive for GABHS as amoxicillin+clavulanate i.e., 75%. Among the gram-positive isolates penicillin and methicillin resistance was found in 45% each for GABHS and 60% and 20% respectively for Staphylococcus aureus.
In study by Vijayshree, et al. majority of the isolates were susceptible to antibiotics penicillin, erythromycin, ampicillin, gentamycin, chloramphenicol, ciprofloxacin, cephalexin, cefotaxime, cefotaxime and amikacin. Drug resistance was observed for 3 of the 9 coagulase positive Staphylococci.
Mahajan, et al., found Methicillin Resistant Staphylococcus Aureus (MRSA) in maximum percentage (56%), followed by Methicillin Sensitive Staphylococcus Aureus (MSSA) which was prevalent in 34% of the cases.
Abhilash A M and Cherian, et al., also found Streptococcus species were sensitive to third or fourth generation Cephalosporins and Amoxycillin-clavulanic acid while Some organisms were multidrug resistant, being sensitive only to piperacillin, ceftriaxone, cefotaxime and meropenem.
In a work done by Wang, et al., beta-hemolytic streptococcus reacted well to penicillin in both groups. However, other bacteria were resistant to penicillin to different degrees. The bacteria in both the RT and TH groups showed nearly 100% sensitivity to third-generation cephalosporin.
Babaiwa, et al. found 81% of Staphylococcus aureus was susceptible to ciprofloxacin, 77% to gentamicin, but were conspicuously resistant to amoxicillin and amoxicillin – clavulanic acid.
Fahaad HM, found sensitivity pattern of penicillin was 60.6%, erythromycin 81.9%, ciprofloxacin 87.6% and vancomycin 81.4%.
Conclusion
In this study GABHS was found to be the most common offending pathogen. This study also suggests amoxicillin+clavulanate or ampicillin is still a good choice of initial empirical therapy until the arrival of throat swab culture sensitivity reports.
Ethical Approval
Ethical approval was obtained from the Institutional review committee of Nobel medical college and teaching hospital.
References
- Yildizoglu U, et al. Effect of antibiotic use on bacterial flora of tonsil core in patients with recurrent tonsillitis. European Archives of Oto-Rhino-Laryngology. Vol. 272, 2015, pp. 1525-1528.
[Crossref] [Google Scholar] [PubMed]
- Gul M, et al. The comparison of tonsillar surface and core cultures in recurrent tonsillitis. American Journal of Otolaryngology. Vol. 28, No. 3, 2007, pp. 173-176.
[Crossref] [Google Scholar] [PubMed]
- Loganathan A, et al. Comparative study of bacteriology in recurrent tonsillitis among children and adults. Singapore Medical Journal. Vol. 47, No. 4, 2006, pp. 271-275. [Crossref]
[Google Scholar] [PubMed]
- Alasmari NS, et al. Causes and treatment of tonsillitis. The Egyptian Journal of Hospital Medicine. Vol. 69, No. 8, 2017, pp. 2975-2980.
- Ingale MH and Mahajan GD. Evaluation of antibiotic sensitivity pattern in acute tonsillitis. International Journal of Otorhinolaryngology and Head and Neck Surgery. Vol. 4, No. 5, 2018, pp. 1162.
- Babaiwa UF, et al. Bacterial tonsillar microbiota and antibiogram in recurrent tonsillitis. Biomedical Research. Vol. 24, No. 3, 2013, pp. 298-302.
- Alexander EH and Hudson M. Factors influencing the internalization of Staphylococcus aureus and impacts on the course of infections in humans. Applied Microbiology and Biotechnology. Vol. 56, 2001, pp. 361-366.
[Crossref] [Google Scholar] [PubMed]
- Sidell D and L Shapiro N. Acute tonsillitis. Infectious Disorders-Drug Targets. Vol. 12, No. 4, 2012, pp. 271-276.
[Crossref] [Google Scholar] [PubMed]
- Fahad HM. Types of aerobic bacteria isolated from Iraqi patients with acute tonsillitis and their susceptibility to different antibiotics. Journal of Pure and Applied Microbiolog. Vol. 12, No. 4, 2018, pp. 1855-1859.
- Kocatürk S, et al. Comparison of adenoid and tonsil core cultures in chronic adenotonsillitis. Kulak Burun Bogaz Ihtisas Dergisi: KBB=Journal of Ear, Nose, and Throat. Vol. 10, No. 3, 2003, pp. 105-109.
[Google Scholar] [PubMed]
- Pichichero ME. Pathogen shifts and changing cure rates for otitis media and tonsillopharyngitis. Clinical Pediatrics. Vol. 45, No. 6, 2006, pp. 493-502.
[Crossref] [Google Scholar] [PubMed]
- Alasil S, et al. Bacterial identification and antibiotic susceptibility patterns of Staphyloccocus aureus isolates from patients undergoing tonsillectomy in Malaysian University Hospital. African Journal of Microbiology Research. Vol. 5, No. 27, 2011, pp. 4748-4752.
- Palumbo FM. Pediatric considerations of infections and inflammations of Waldeyer's ring. Otolaryngologic Clinics of North America. Vol. 20, No. 2, 1987, pp. 311-316.
[Crossref] [Google Scholar] [PubMed]
- Bista M, et al. Tonsillar microbial flora: A comparison of infected and non-infected tonsils. Kathmandu University Medical Journal (KUMJ). Vol. 4, No. 1, 2006, pp. 18-21.
[Google Scholar] [PubMed]
- Cowan DL and Hibbert J. Acute and chronic infection of the pharynx and tonsils. Scott-Brown1s Otolaryngology. Vol. 5, No. 6, 1997.
- Cherian M, et al. Acute tonsillitis in adults: the bacteriological profile and antibiotic sensitivity pattern in Ajman, UAE. Gulf Medical University: Proceedings. Vol. (5-6), 2012, pp. 61-65.
- Baâ?Saddik IA, et al. Prevalence of Group A betaâ?haemolytic Streptococcus isolated from children with acute pharyngotonsillitis in Aden, Yemen. Tropical Medicine and International health. Vol. 19, No. 4, 2014, pp. 431-439.
[Crossref] [Google Scholar] [PubMed]
- Wang Q, et al. Bacteriology and antibiotic sensitivity of tonsillar diseases in Chinese children. European Archives of Oto-Rhino-Laryngology. Vol. 274, 2017, pp. 3153-3159.
[Crossref] [Google Scholar] [PubMed]
- Evans AS and Dick EC. Acute pharyngitis and tonsillitis in University of Wisconsin students. JAMA. Vol. 190, No. 8, 1964, pp. 699-708.
[Crossref] [Google Scholar] [PubMed]
