Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
The Influence of Kinesiophobia on Clinical Practice in Physical Therapy: An Integrative Literature Review
Beatriz Castanho*, Nuno Cordeiro and Vítor PinheiraBeatriz Castanho, Department of Physical Therapy, Polytechnic Institute of Castelo Branco, Portugal, Email: beacastanho@gmail.com
Received: 30-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Objective: To analyze how kinesiophobia influences clinical practice in physiotherapy through an integrative analysis of the literature of several published articles. Design: An integrative literature review. Methods: Integrative literature review conducted at the Pedro, b-on, PubMed, Cochrane, and Research Gate databases, using the descriptors physiotherapy, physical therapy, and kinesiophobia between May and June 2019. Articles on the physiotherapist’s work with kinesiophobia, available in full-text, in English, Portuguese or Spanish, with a 10-year publication restriction, were searched. Results: Ultimately, a total of 15 articles fulfilled all inclusion criteria and were selected for the integrative literature review. Conclusion: Kinesiophobia is a frequent condition in many musculoskeletal conditions. Is it a concept that has been increasingly studied and approached, recognizing its importance in clinical practice in physiotherapy? Physiotherapists should not neglect their evaluation through the validated TSK tool. Kinesiophobia should be addressed through the CBT program, coupled with the exercise program. The physiotherapist’s expectation of the patient influences the outcome, and should always offer support and encouragement.
Keywords
Kinesiophobia, Physical therapy, Fear of movement, Catastrophization, Integrative review
Introduction
Kinesiophobia is a condition that began to be understood in the last two decades [1]. The term “kinesiophobia” (kinesis=movement) was introduced by Kori, et al. in 1990; this condition has been described as “an excessive, irrational and debilitating fear of physical movement and activity resulting from a feeling of vulnerability to a painful injury or a new injury” [2-5]. These authors also developed the Tampa Scale for Kinesiophobia (TSK) as a measure of fear of (re) injury/movement [4,5]. When individuals are unable to perform activities because they believe they will increase their pain, kinesiophobia develops. This situation negatively affects the functions of the patients, namely their Activities of Daily Living (ADL) and practice of exercise and/or physical activity [3,6]. Therefore, users are not only afraid of pain but also fear of movement that can cause pain [5].
The prevalence of kinesiophobia in patients with persistent pain varies between 50% and 70%, with men reporting a higher prevalence than women [7]. Rarely is it applicable to all types of physical activity, applying only to certain movements. We have as an example the extension of the neck in patients after whiplash, overload in patients with impingement syndrome of the shoulder, or leaning forward with patients with low back pain. Even if these movements have caused pain in the subacute phase, they are safe to be performed in the chronic phase. As the brain has acquired a long-term memory of pain, it associates these movements or just their preparation to danger or threat [4,8]. These protective behaviors may persist in anticipating pain rather than responding to it [4]. Movement and function are therefore avoided as a result of fear of pain or (re) injury, mediated by catastrophic thoughts about the experience of pain and hypervigilance about painful sensations, with the net result of disuse and inability [1].
Kinesiophobia has also been related to a low level of physical activity in patients with persistent pain, poor clinical performance, reduced performance in behavioral tasks, incapacity in activities of daily living, and loss of work in individuals with low back pain [9].
FAM-Fear Avoidance Model
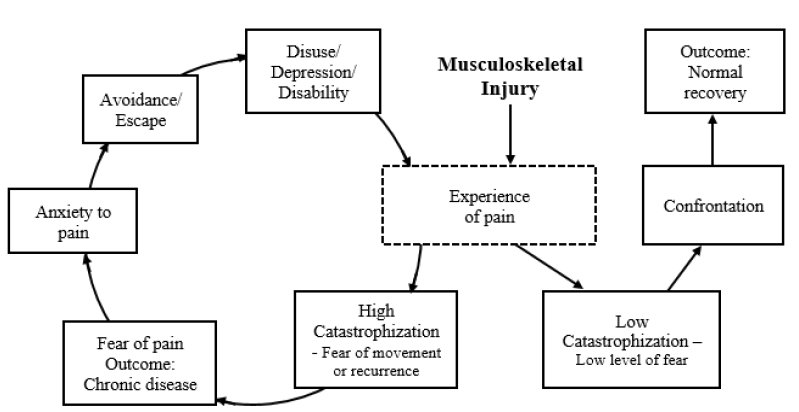
Kinesiophobia is a psychological construct within the Fear Avoidance Model (FAM) [9]. The FAM explains how and why pain injuries result in chronic pain and its comorbidities (disuse, depression, and disability) [10]. FAM may be the major cause of functional dysfunctions in patients with kinesiophobia. According to this model, fear can result in avoidance and inactivity behavior, eventually leading to disability [11,12]. The basic principle of the model is that the way pain is interpreted can lead to two different pathways. When acute pain is perceived as non-threatening, patients are likely to remain involved in daily activities through which functional recovery is promoted. In contrast, a vicious circle can be initiated when the pain is catastrophically (poorly) interpreted. These dysfunctional interpretations give rise to pain-related fear and associated safety-seeking behaviors, such as avoidance/flight and hypervigilance, which may be adaptive at the stage of acute pain, but paradoxically worsen the problem in the case of long-term pain [1,13] (Figure 1).
Figure 1. Adaptation to the Fear Model Avoidance model pain; based on the model of Leewu et al. and Vlayen et al. [5]
Objective
The main objective of this integrative literature review is the execution of a scientific survey and synthesis of the results obtained from the research on the research problem “In what way does kinesiophobia influence clinical practice in physiotherapy?”, In a systematic way, thus constituted a body of knowledge. This integrative review has the purpose of methodological analysis of the included studies of this particular topic.
Materials and Methods
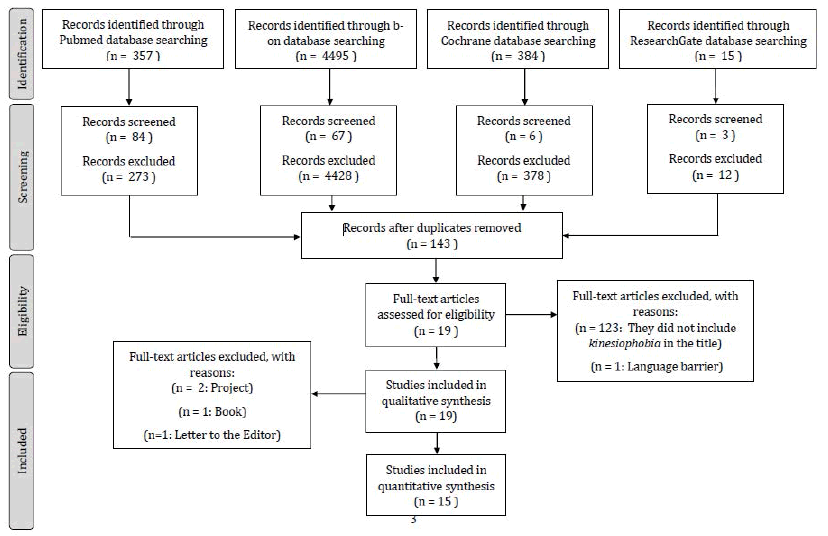
To develop the study, the following steps were followed: selection of the guiding question; establishment of keywords, inclusion and exclusion criteria and search in the literature; evaluation of studies included in the integrative review; definition of the information to be extracted; interpretation of the results and presentation of synthesis of the knowledge produced [14]. The search and selection of the papers are presented according to the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyzes) (Figure 2).
Selection of the Guiding Question
The guiding question of the study is “In what way does kinesiophobia influence clinical practice in physical therapy?”
Establishment of Keywords
The keywords of this integrative review are Kinesiophobia, Physical therapy, Fear of movement, Catastrophization, Integrative review.
Inclusion and Exclusion Criteria
Articles that meet the following requirements were included in the review:
• Physiotherapy articles on the various implications of kinesiophobia
• Article available in full text
• Article available in English, Spanish or Portuguese
• Less than 10 years of publication
There were excluded from the review articles that are:
• Literature reviews
• Theses
• Monographs
• Works that describe academic activities
Search in Literature
The searches were conducted in the databases PEDro-Physiotherapy Evidence Database-, b-on- Online Knowledge Library, PubMed, Cochrane Library, and ResearchGate through the descriptors physiotherapy, physical therapy, and kinesiophobia. To systematize the searches, the Boolean operators were used with the following scheme: (physiotherapy OR physical therapy AND kinesiophobia).
Evaluation of the Studies
The analysis of the validity of the studies was made by different scales, according to the type of study, to identify the internal validity and if the articles contain enough statistical information for the results to be interpretable. To evaluate the validity of RCT (Randomized Controlled Trial), the PEDro (Physiotherapy Evidence Database scale) adapted to Portuguese was used [15]. To evaluate the validity of RT (Randomized Trials) the CONSORT scale was used. STROBE (The Strengthening of the Reporting of Observational Studies in Epidemiology) was used to evaluate observational studies-cohort, case-control studies, and cross-sectional studies. The STARD (Standards for Reporting Diagnostic Accuracy Studies) was used to evaluate prognostic/diagnostic studies. The CARE (Consensus-based Clinical Case Reporting Guideline Development) was used for the case report (case report), adapted in Portuguese. Finally, the AGREE Reporting Checklist served to evaluate clinical practice guidelines.
Results
Data Extraction
A total of 5251 references were identified from electronic databases in the search performed on May 27 and 28, 2019 (Table 1). The screening was done with the investigation of articles that met the criteria of inclusion and exclusion criteria, remaining only 160 articles. Once duplicate entries had been removed, references were further evaluated for inclusion based on the title and/or abstract [16]. 19 potentially relevant articles were thereby included in the next stage for full-text evaluation.
| Reference | Article | Conclusions | Type of article |
|---|---|---|---|
| [17] | A Higher-Order Analysis Supports Use of the 11-Item Version of the Tampa Scale for Kinesiophobia in People With Neck Pain | The TSK-11 can be considered an interval-level measure when used in people with neck pain. It provides potentially important information regarding the nature of the neck-related disability. The clinically important difference may not be consistent across the range of the scale. | Randomized Controlled Trial |
| [16] | Effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in women with menstrual low back pain: A preliminary trial | This preliminary study assessed the effect of functional lumbar stabilization exercise (with emphasis on deep stability muscles) on pain, disability, and kinesiophobia in women with menstrual LBP. It seems that lumbar stabilization exercise has the potential to decrease LBP and disability for women who have LBP during their menses. | Randomized Trial |
| [18] | Kinesiophobia-Introducing a New Diagnostic Tool | Kinesiophobia Causes Scale may constitute a useful tool for the identification and quantification of both biological and mental causes for kinesiophobic behaviors in individuals and populations. From a prophylactic perspective, the identification of causes of kinesiophobia constitutes a necessary and basic start point to any coordinated actions. | Cross-sectional Study |
| [19] | Prevalence of anxiety, depression, and kinesiophobia in patients with low back pain and their association with the symptoms of low back spinal pain | There was no association between the symptoms of anxiety and depression. However, patients who were classified in the Organic group were more likely to experience kinesiophobia. | Randomized Controlled Trial |
| [20] | Does a Program Based on Cognitive Behavioral Therapy Affect Kinesiophobia in Patients Following Total Knee Arthroplasty? A Randomized, Controlled Trial With a 6-Month Follow-Up | The CBT program was superior to standard care in reducing kinesiophobia, pain catastrophizing, and knee pain and in enhancing knee function in patients who have a high level of kinesiophobia following TKA. The treatment effect was clinically significant and lasted for at least 6 months after the end of the intervention. | Randomized Controlled Trial |
| [6,21] | Group-based task-oriented exercises aimed at managing kinesiophobia improved disability in chronic low back pain | This light group-based multidisciplinary cognitive-behavioral rehabilitation program was superior to traditional exercises in reducing disability, kinesiophobia, catastrophizing, and enhancing the quality of life of subjects with CLBP. The effects lasted for at least 2 years after the end of the intervention. | Randomized Controlled Trial |
| Determining the relationship of kinesiophobia with respiratory functions and functional capacity in ankylosing spondylitis | Kinesiophobia is a condition that may arise in AS. This study showed the effects of this negative belief on functions with a tendency to decrease in individuals such as respiratory functions, chest expansion, functions used frequently in daily life, and axial mobility. This result shows that the losses of individuals due to the disease will be even more severe with kinesiophobia, and the exercise programs organized for individuals with AS should consider kinesiophobia in terms of physiotherapy and rehabilitation and prefer exercise where the individual will be more active. | Observational Study | |
| [22] | Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial | Virtual walking integrated physiotherapy reduces pain and kinesiophobia, and improved function in patients with subacute and chronic non-specific low-back pain in short term. | Randomized Controlled Trial |
| [12] | Effectiveness of Postoperative Home- Exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: A Randomized Controlled Trial | Progressive 12-month home exercise starting 3 months postoperatively was not superior to usual care in decreasing kinesiophobia or increasing physical activity in spondylolisthesis. | Randomized Controlled Trial |
| [23] | Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms | Postpartum women still in pain at 3 months should be managed due to its impacts and to the risk of persistent pain. Because 10%-20% of women report pregnancy as a debut of persistent lumbopelvic pain and because pregnancy is a specific situation that is easy to identify, pregnancy is a potential ‘‘prevention point’’ for persistent lumbopelvic pain. | Randomized Trial |
| [24] | Kinesiophobia After Anterior Cruciate Ligament Rupture and Reconstruction: Noncopers Versus Potential Copers | Kinesiophobia levels were high in both noncopers and potential copers preop- iteratively. Restoration of mechanical knee stability with surgery might have contributed to decreased kinesiophobia levels in noncopers. Kinesiophobia is related to knee function after surgery, regardless of preoperative classification as a potential coper or noncoper. | Cohort Study |
| [25] | Kinesiophobia and its relation to pain characteristics and cognitive-affective variables in older adults with chronic pain | Results indicate that potential interventions regarding kinesiophobia among older adults should aim to decrease pain intensity and strengthen health beliefs. | Observational Study |
| [26] | Management of catastrophizing and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomized controlled trial | The rehabilitation program, including the management of catastrophizing and kinesiophobia, was superior to the exercise program in reducing disability, dysfunctional thoughts, and pain, and enhancing the quality of life of patients after lumbar fusion for degenerative spondylolisthesis and/or lumbar spinal stenosis. The effects lasted for at least 1 year after the intervention ended | Randomized Controlled Trial |
| [27] | The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: A pilot study | Pain catastrophizing and kinesiophobia decreased significantly during rehabilitation. A higher level of pain catastrophizing was significantly correlated with a greater level of knee pain during activities, more difficulties experienced during daily activities before and after rehabilitation. A high level of kinesiophobia was significantly correlated with more difficulties experienced in daily activities and poorer knee-related quality of life before and after rehabilitation | Observational Study |
| [28] | Validation of a questionnaire to detect kinesiophobia (fear of movement) in patients with coronary artery disease | They have provided introductory support for the TSK-SV Heart as a reliable instrument for use in patients with CAD, and have established its face, content, and construct validity. Further research is needed in this area to deepen the understanding of kinesiophobia and its meaning for physical activity and exercise in patients with CAD. | Cross-sectional Study |
These publications included: 2 Cross-sectional Studies; 3 Observational Studies; 1 Cohort-studies; 2 Randomized Trials; 7 Randomized Controlled Trials. The other four studies were two projects, one letter to the editor, and one book. Ultimately, a total of 15 articles fulfilled all inclusion criteria and were selected for the integrative literature review.
Study Quality
For the evaluation of the study quality, it was used the PEDro scale was for the Randomized Controlled Trials, CONSORT for Randomized Trials, and STROBE for all kinds of observational studies. The methodological quality of the included studies was satisfactory.
Study Characteristics
The main characteristics of the selected studies are summarized in Table 1. The fifteen studies enrolled a total of 2072 individuals. Of these, six studies divided the subjects into experimental and control groups: 280 in the experimental group (i.e., subjects that were assigned to a program) and 272 in the control group (i.e., subjects receiving standard treatment). 953 subjects were part of six studies whose main objective was to determine the relationship/impact between kinesiophobia and other conditions, and so they didn’t do any division. Two studies evaluated the measurement properties of the TSK-11 and the validation of the TSK-SV, including 567 participants. The remaining article did not include any participants as it was an introduction to a new diagnostic tool. The age of the enrolled subjects in the fifteen studies varied from 15 to 78 years.
Walton, et al. in his study evaluated the measurement properties of the TSK-11 when used in people with mechanical neck pain of any mechanism and any duration (N=235), aged between 18 and 65 years, from 2009 and 2012 [16].
In the study by Shakeri, et al., they investigated the effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in a woman with menstrual LBP (N=30) during the menstrual phase (days 1-6) of the menstrual cycle, from the Tehran region, between the ages of 19 and 39 years. Subjects were assigned to a control group (n=10) and an intervention group (n=20) [16].
In 2011, Knapik, et al. introduced a new tool aiming to diagnose limitations of motor activity, named: Kinesiophobia Causes Scale (KCS). It is devised for an adult population and aims to diagnose original causes of motor passivity [18].
The study by Trocoli, et al., it was evaluated the prevalence of anxiety, depression, and kinesiophobia and their associations with the symptoms of LBP. For that, a total of 65 patients aged 18-80 years (from May to December 2013) were divided into three groups: Organic (n=35), Amplified Organic (n=14), and Non-Organic (n=16) [19].
Cai, et al. in his study (between January and December 2011) evaluated the effects of a Cognitive Behavioral Therapy (CBT) program on kinesiophobia, knee function, pain, and pain catastrophizing in patients following Total Knee Arthroplasty (TKA) from June 2015 to October 2016 (N=100). Subjects were assigned to a control group (n=50) and an experimental group (n=50), aged between 45 and 75 years old [20].
In the study by Monticone, et al., 150 patients aged 42-64 years old were randomly assigned to a 5-week group-based multidisciplinary program of task-oriented exercises integrated with cognitive-behavioral therapy mainly aimed at managing kinesiophobia (experimental group: n=75) or group based traditional exercises (control group: n=75) [21].
Between November 2014 and May 2015, Yilmaz et al. investigated the short-term effect of virtual reality on pain, function, and kinesiophobia in patients with subacute and chronic non-specific LBP, 36-53 years old. 44 participants were randomly assigned to the control group (n=22) and the experimental group (n=22) [22].
In the study by Goktug, et al., 31 individuals with Ankylosing Spondylitis (AS) were included, aged between 20 and 70 years old. The purpose was to investigate the effects of kinesiophobia in AS on pulmonary function tests and functional performance [6].
In the study by Ilves, et al., the main objective was to study the effectiveness of 12-month exercise therapy on kinesiophobia and physical activity in patients (aged 47-71 years old) with spondylolisthesis after lumbar spine fusion. Three months postoperatively, they were randomized into an exercise group (n=48) or usual care group (n=50) [12].
In the study by Gutke, et al., it was evaluated the prevalence of subgroups of lumbopelvic pain, disability, pain intensity, Health-Related Quality of Life (HRQL), activity level, and kinesiophobia in a cohort of women (N=272) aged between 18-44 years old, at 3 months postpartum and to investigate the association between disability and these factors, including depressive symptoms [23].
In the study by Hartigan, et al., two groups were considered: potential copers (n=50) and noncopers (n=61), aged between 15-37 years old, from two clinical trial databases. The main objective was to compare kinesiophobia levels in noncopers and potential copers at time points spanning pre and post-ACL reconstruction and to examine the association between changes in kinesiophobia levels and clinical measures [24].
Larsson et al. studied the prevalence at baseline, development over 12 months, and cognitive-affective variables of kinesiophobia in a population-based sample of older adults (N=433) aged between 65-78 years old with chronic pain [25].
Monticone, et al. also developed another study, where the main objective was to evaluate the effect of a rehabilitation program including the management of catastrophizing and kinesiophobia on disability, dysfunctional thoughts, pain, and the QoL in patients after lumbar fusion for degenerative spondylolisthesis and/or lumbar spinal stenosis. 130 patients aged between 46-70 years old were randomly assigned to a program consisting of exercises and cognitivebehavioral therapy (experimental group: n=65) or exercises alone (control group: n=65) [26].
In the study by Tichonova, there were two main objectives: to measure pain catastrophizing and kinesiophobia levels and determine their association with self-reported subjective knee function during rehabilitation, following ACL reconstruction (n=22) and meniscectomy (n=19). This study included 41 participants aged between 25 to 50 years old [27].
Back, et al., in 2011, investigated the validity and reliability of the Tampa Scale for Kinesiophobia Heart (TSK-SV Heart) in patients with coronary artery disease. A total of 332 participants aged between 46-74 years old were included in the study [28].
Evaluation-Scales Adopted of the Studies for Measuring the Level of Kinesiophobia of the Participants
Table 2 summarizes all the scales adopted of the studies for measuring the level of kinesiophobia of the participants.
| Article | Scale adopted |
|---|---|
| A Higher-Order Analysis Supports Use of the 11-Item Version of the Tampa Scale for Kinesiophobia in People With Neck Pain [17] | 11-item version of the Tampa Scale for Kinesiophobia (TSK-11) |
| Effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in women with menstrual low back pain: A preliminary trial [16] | Tampa Scale for Kinesiophobia (TSK) |
| Kinesiophobia-Introducing a New Diagnostic Tool [18] | Kinesiophobia Causes Scale (KCS) |
| Prevalence of anxiety, depression, and kinesiophobia in patients with low back pain and their association with the symptoms of low back spinal pain [19] | The Brazilian version of the Tampa Scale for Kinesiophobia (TSK) |
| Does a Program Based on Cognitive Behavioral Therapy Affect Kinesiophobia in Patients Following Total Knee Arthroplasty? A Randomized, Controlled Trial With a 6-Month Follow-Up [20] | The simplified Chinese version of the Tampa Scale for Kinesiophobia (SC-TSK); |
| Group-based task-oriented exercises aimed at managing kinesiophobia improved disability in chronic low back pain [21] | Validated Italian 13-item version of the self-report Tampa Scale for Kinesiophobia (TSK) |
| Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial [22] | Tampa Scale for Kinesiophobia (TSK) |
| Determining the relationship of kinesiophobia with respiratory functions and functional capacity in ankylosing spondylitis [6] | Tampa Scale for Kinesiophobia (TSK) |
| Effectiveness of Postoperative Home-Exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: A Randomized Controlled Trial [12] | The Finnish version of the Tampa Scale for Kinesiophobia (TSK) |
| Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms [23] | Tampa Scale for Kinesiophobia (TSK) |
| Kinesiophobia After Anterior Cruciate Ligament Rupture and Reconstruction: Noncopers Versus Potential Copers [24] | 11-item version of the Tampa Scale for Kinesiophobia (TSK-11) |
| Kinesiophobia and its relation to pain characteristics and cognitive-affective variables in older adults with chronic pain [25] | 11-item version of the Tampa Scale for Kinesiophobia (TSK-11) |
| Management of catastrophizing and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomized controlled trial [26] | Validated Italian 13-item version of the self-report Tampa Scale for Kinesiophobia (TSK); |
| The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: A pilot study [27] | 11-item version of the Tampa Scale for Kinesiophobia (TSK-11); |
| Validation of a questionnaire to detect kinesiophobia (fear of movement) in patients with coronary artery disease [28] | The Swedish version of the Tampa Scale for Kinesiophobia Heart (TSK-SV Heart) |
Of the 15 studies, 8 used the conventional 17 items Tampa Scale for Kinesiophobia (TSK); 4 studies used the 11- item version of the Tampa Scale for Kinesiophobia (TSK-11); 1 study used the 13-item version of the Tampa Scale for Kinesiophobia; 1 study used the Tampa Scale for Kinesiophobia Heart (TSK-SV Heart); And finally, 1 study introduced a new tool, the Kinesiophobia Causes Scale (KCS).
Intervention-Control group versus Experimental group
Table 3 summarizes all the types of intervention the experimental and the control groups were submitted.
| Article | Control group | Experimental group |
|---|---|---|
| Effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in women with menstrual low back pain: A preliminary trial [16] | No exercise and performed their regular activity daily living. | Functional lumbar stabilization exercises, 10 repetitions each, 3 times a day, for 3 consecutive months. |
| Does a Program Based on Cognitive Behavioral Therapy Affect Kinesiophobia in Patients Following Total Knee Arthroplasty? A Randomized, Controlled Trial With a 6-Month Follow-Up [20] | Standard care. These patients received standardized information including postoperative routines, pain management, and rehabilitation exercise based on TKA patients in general. | Rehabilitation exercise. Cognitive Behavioral Therapy Program (CBT). |
| Group-based task-oriented exercises aimed at managing kinesiophobia improved disability in chronic low back pain [21] | The usual-care rehabilitation included exercises for passive spinal mobilization, strengthening, muscle segmentary stretching, and postural control. | Task-oriented exercises. Cognitive Behavioral Therapy Program (CBT). |
| Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial [22] | Traditional therapy only using physical agent modalities. | Traditional therapy. Physiotherapy integrated Virtual Walking (VW). |
| Effectiveness of Postoperative Home- Exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: A Randomized Controlled Trial [12] | A single session of physiotherapy instruction. | 12-month progressive home-based training with regular booster sessions. |
| Management of catastrophizing and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomized controlled trial [26] | Exercise training. | Exercise training. Cognitive Behavioral Therapy Program (CBT). |
Of 15 articles, 6 made the distinction between the control group and experimental group. Half of the studies included a Cognitive Behavioral Therapy Program on his experimental group, 1 included exercise training for functional lumbar stabilization, 1 integrated Virtual Walking (VW), and 1 included a Postoperative Home Exercise [3]. All of the studies that proposed CBT in the experimental group also included exercise training/task-oriented exercise/rehabilitation exercise. In the control group, they all provided the standard care, except for the study conducted by Ilves, et al., where the control group only performed their regular activity of daily living.
Discussion
What is kinesiophobia? Is it a dichotomous characteristic or a syndrome that varies in degree?
Why do many people prefer a passive lifestyle although they are aware of numerous advantages of motor activity? To answer such a question, one must understand the meaning of the limitations of the activity. The great variability of human behavior, as well as numerous factors influencing the level of activity prompt to approve a simplified theoretical model explaining the reasons for commencing the motor activity, in which the broad spectrum of motivations and limitations is reduced to two major items: (1) biological: structural, morphologic, energetic, instinctive; (2) psychosocial: personality, culture, emotions. It is worth mentioning that practically the border between the two mentioned spheres is somehow blurred and it is frequently the case that the most important limitation of motor activity is fear of movement, regarded as a component of the personality of an individual. This type of attitude is referred to in the literature as kinesiophobia [18].
In recent years, the integration of the bio-psychosocial model in rehabilitation has been receiving attention in clinical research. Implementing psychological factors assessment and management in rehabilitation for patients with musculoskeletal injuries/pain can aid in the decision-making process and improve outcomes. Therefore, it is important to know which psychological factors are related to the rehabilitation process and can contribute to a good recovery. The psychological influences such as self-efficacy, confidence in function, pain catastrophizing, kinesiophobia, or re-injury may modulate individual perception and response to the illness and may influence functional level after musculoskeletal injury [27].
Kinesiophobia, as described previously, is defined as an excessive, irrational, and debilitating fear of physical movement and activity resulting from a feeling of vulnerability due to painful injury or re-injury [20].
According to the fear-avoidance model, patients can respond to a fear of movement in 1 of 2 ways: by confronting fear or avoiding fear. Confrontation leads to reduced fear, active exercise, and faster recovery [19,20]. In contrast, avoidance can lead to kinesiophobia, pain-related fear of movement, which may lead to impaired behavior and subsequent disability characterized by poor cognitive and physical performance, such as disuse syndrome, depression, and decreased physical function, thus creating a vicious cycle of pain and disability, causing a new problem [19,20]. When a painful experience is interpreted as threatening, it can generate catastrophizing cognitions that activity will result in more pain and re-injury. As this goes on, this can lead to avoidance behavior, which in the long run causes disability, disuse, and depression as well as a patient trapped in a cycle of increased fear of pain, more pain, and disability. For older adults the consequences of disuse and decreased activity can be serious, increasing the risk for a wide range of health problems, functional decline, and premature death [25,27]. Pain catastrophizing and fear of pain is a major cause of delayed recovery and discharge after musculoskeletal injury and surgery [27].
About the fear-avoidance model, psychological factors such as catastrophizing, fear-avoidance beliefs, and mood alterations may coexist and become important determinants of chronic symptoms, disability, and illness behaviors that induce subjects to sacrifice everyday tasks or the use of adaptive coping strategies [26].
Contemporary, the phenomenon of kinesiophobia has however a broader range of influence and cannot be fully explained as a simple fear of pain. It may well appear as a fear of physiological symptoms of fatigue or exhaustion or, even more comprehensively, fear of physical or mental discomfort. In the case of kinesiophobia, various defense mechanisms may appear, such as repression, negation, simulation, and projection or, most frequently used, rationalization. Typical psychosomatic symptoms are rather rare and may only appear when a kinesiophobia individual is, by any means, forced to increase activity [18].
Except for the mechanisms outlined in the fear-avoidance model, increasing attention has been given to self-efficacy as a mediating factor between pain-related fear (kinesiophobia) and avoidance behavior. Self-efficacy relates to the belief in one’s capacities and individuals with high self-efficacy seem to have a higher ability to manage challenging situations and setbacks than individuals with low self-efficacy [25].
Increasing attention has been given to self-efficacy in explaining pain and pain disability. Self-efficacy is the strongest predictor of pain disability, suggesting self-efficacy as a mediator between pain-related fear and avoidance behaviors in the fear-avoidance model. However, the mediating effect was dependent on the level of self-efficacy, i.e., when selfefficacy was high, elevated pain-related fear did not lead to greater pain and disability. But where self-efficacy was low, elevated pain-related fear was more likely to lead to greater pain and disability [25].
How can it be measured? Tampa Scale for Kinesiophobia-Evaluating the level of Kinesiophobia
As with most musculoskeletal pain conditions, cognitions and beliefs about the symptoms, fear of movement or reinjury, and social or environmental factors also contribute to a person’s experience of disability. In the absence of hard diagnostic signs of these constructs, clinicians must rely upon the judicious use of carefully constructed, wellvalidated self-report measures to better identify specific factors that could influence clinical outcomes. One such tool is the Tampa Scale of Kinesiophobia (TSK) [16].
The Tampa Scale of Kinesiophobia has been used as a powerful selector of patients with poor psychological profiles and, therefore, those with a poor prognosis for therapy [19]. Originally intended for use in people with chronic low back pain, both forms of the TSK have shown increasing use among other clinical populations [16]. The TSK is a 17-item questionnaire designed to assess kinesiophobia. Subjects were asked to indicate their level of agreement to each of the 17 statements on a 4-point response scale, with scoring alternatives from “strongly disagree” to “strongly agree.” Results range from 17 to 68, with scores greater than 37 indicating a high degree of kinesiophobia. The TSK has been considered to have a face and content validity as well as stability over time and internal consistency [16].
A re-evaluation of the original scale’s properties by Woby and colleagues led to the removal of the 4 reverse-scored items and 2 additional poorly performing items, creating an 11-item version of the Tampa Scale for Kinesiophobia (TSK-11) [17]. Comparing TSK-11 scores between different musculoskeletal pain conditions should be considered pain duration and intensity, disease category, injury mechanism, patterns of improvement in pain intensity and function, the prognosis of recovery, and rehabilitation professionals’ attitudes toward different medical conditions [27].
Goktug, et al. claim that currently, no firm diagnostic criteria exist for identifying kinesiophobia, and they suggest that the TSK-11 provides a measure of general negative valence toward exercise, but not an irrational fear or specific phobia [17].
The TSK has been adapted to different situations, including for neck pain and patients with Coronary Artery Disease (CAD) [17,28]. Walton, et al. concluded that The TSK-11 can be considered an interval-level measure when used in people with neck pain and that it provides potentially important information regarding the nature of the neck-related disability, although the clinically important difference may not be consistent across the range of the scale [17].
The results of the study of Back et al support the reliability and validity of the TSK-SV Heart questionnaire for use in patients with CAD. The TSK-SV Heart was found to be stable over time, and this result is consistent with the previously reported test-retest reliability of the TSK in patients with chronic pain, providing introductory support for the TSK-SV Heart as a reliable instrument for use in patients with CAD [28].
The use of scales for diagnostics may allow physiotherapists to identify subgroups of patients who need the treatment for negative fear-avoidance beliefs. Also, a better understanding of factors that influence pain catastrophizing and kinesiophobia levels is needed so that interventions can be targeted to individuals who will benefit the most [27].
Kinesiophobia Causes Scale (KCS)-A new scale to measure kinesiophobia: Knapik, et al. postulated that there is a need for proper diagnosis of the causes and intensity of kinesiophobia [18].
And so, they develop the Kinesiophobia Causes Scale (KCS). It is devised for an adult population and aims to diagnose original causes of motor passivity [18]. KCS may constitute a useful tool for the identification and quantification of both biological and mental causes for kinesiophobic behaviors in individuals and populations. From a prophylactic perspective, the identification of causes of kinesiophobia constitutes a necessary and basic start point to any coordinated actions [18].
In this article, the authors introduced a new, original tool aiming to diagnose the limitations of motor activity. These limitations must be described in the light of phobic behaviors, which normally are not susceptible to change, of relatively constant intensity, connected with avoidance of triggering factors and irrational. Therefore, a numeric scale is proposed in which a score of 100 would mean a highly kinesiophobic attitude and 0 would represent a lack of any symptoms of kinesiophobia [18].
According to the authors, the identification of causes of kinesiophobia should be followed by actions directed towards their minimization or elimination. This creates a new and broad area of research. After testing its validity, reliability and internal consistency KCS may well serve as a diagnostic tool helping to start preventive and therapeutic procedures [18].
How can it be treated?-Managing Kinesiophobia
Cognitive behavioral therapy: The integration of the biopsychosocial model in rehabilitation has recently received attention in clinical research. It has been reported that psychological factors, such as self-efficacy, pain catastrophizing, and kinesiophobia, strongly influence pain perceptions, rehabilitation compliance, and response to physical activity, which may influence outcomes after knee arthroplasty [20].
Multidisciplinary programs based on Cognitive Behavioral Therapy (CBT) have been increasingly used in addition to other therapies such as exercise, to alter maladaptive thoughts and behaviors, improve lumbar function and enhance the use of self-management skills [21].
Previous studies included a wide range of cognitive-behavioral interventions, such as problem-solving, restructuring of maladaptive thinking patterns, relaxation, management of fear-avoidance behaviors, and maladaptive coping strategies, but further evidence is required to better define which should be the preferred approach when group-based multidisciplinary rehabilitation is planned [21].
Few studies have attempted to examine the management of kinesiophobia by adopting a cognitive-behavioral approach. Earlier research has shown that interventions based on CBT may decrease kinesiophobia and pain catastrophizing, thus contributing to improved knee function [20].
Cai, et al. conducted a program based on cognitive behavioral therapy in patients following Total Knee Arthroplasty (TKA). For the experimental group, they had 4 different sessions [20]. The first Session included the analysis of kinesiophobia, person-centered. The purpose of this session was to analyze the factors causing kinesiophobia. The physiotherapist discussed with patients the kinds of physical activities the patients wished to perform during the first or second day after TKA surgery. Patients were asked to make a list of physical activities that they would like to do but had stopped performing because of kinesiophobia after TKA. Then, the patients were encouraged to select one of these physical activities and set daily activity goals. Assessment questionnaires were used to identify psychological risk factors for a high level of kinesiophobia. Before session 2, the patients were asked to complete the TSK and Pain Catastrophizing Scale (PCS) questionnaires [20]. The second session was about kinesiophobia education. The patients were involved in an individual kinesiophobia education program aimed at modifying their kinesiophobia beliefs and pain catastrophizing under the supervision of a clinical psychologist [20].
At the third session, progressive muscular relaxation. This session aimed to teach patients how to apply rapid relaxation in risky situations and improve patients’ self-efficacy, which was regarded as important for the ability to stay active despite pain [20]. In the last session, they graded knee functional rehabilitation exercises. The purpose of this session was to help patients transfer their attention from kinesiophobia to the knee functional rehabilitation exercise using graded exposure to situations they had previously identified as dangerous [20].
Monticone, et al. similarly developed program Group-based task-oriented exercises in patients with chronic low back pain [20].
For the experimental group, basic exercises were firstly introduced to improve spinal mobility and deep muscle awareness. Additional exercises, such as turning, standing on unstable surfaces, and walking while changing speed and direction, were aimed at recovering coordination, balance, and walking abilities as well as other functional demands of daily living [20]. Under the supervision of a clinical psychologist, the patients were also involved in group-based CBT aimed at modifying fear of movement beliefs and ensuring gradual reactions to illness behaviors. After explaining the fear-avoidance model, patients were educated to view pain as a situation that can be self-managed rather than a serious disease needing vigilant protection. The main situations avoided were identified based on the fear-avoidance beliefs emerging from the group discussion regarding the activities more frequently reported, the administered questionnaires, and the presentation of images showing back-stressing activities. Whenever fear-avoidance behaviors of a single subject were revealed, these were shared and debated within the whole group to identify the most suitable solutions, as correct re-learning and cognitive restructuring were based on developing an awareness of the problem and seeking a means of reacting to frightening thoughts [21].
Solutions were provided by educating subjects on the nature of chronic pain: information on chronic conditions had to be retained, understood, and applied to current problems to reduce the threat of pain itself as well as to change how they see themselves and behave; subjects were encouraged to combine pain physiology with active and paced movement approaches to gradually increase physical capacity, reduce pain and improve quality of life [21]. Relaxation, as well as attention techniques such as distraction and desensitizing, were shared with the subjects to facilitate graded exposure and control over pain. Moreover, advice to develop helpful ways of thinking was provided to master fearful situations and to minimize the level of distress; ways to challenge and change the unhelpful way of thinking were also encouraged to keep under control mood disorders [21]. Based on a close collaboration between the psychologist and the physiotherapists, the fear-avoidance beliefs coming out were used to choose the task-oriented exercises to perform to outline an exposition treatment to feared movement [21].
Monticone, et al. also developed a cognitive-behavioral therapy program for patients with lumbar spondylolisthesis and stenosis [26]. Under the supervision of the psychologist, the purpose was to modify catastrophizing and the fear of movement by ensuring gradual reactions to illness behaviors. After explaining the fear-avoidance model, the patients were educated to view their pain as something that can be self-managed rather than a serious disease that needs vigilant protection. Correct relearning was based on developing an awareness of the problem and seeking a means of reacting to frightening thoughts. The subjects were assisted in transferring their attention from a fear of moving to increase their level of activity using graded exposure to the situations they had previously identified as dangerous. The reacquisition of adaptive coping strategies was promoted using communication, motivation, and sharing the goals to be reached during common activities [26]. As for the Control Group, in both programs, standard care was provided to the control group at the ward. These patients received standardized information including postoperative routines, pain management, and rehabilitation exercise based on TKA/Low back pain/lumbar spondylolisthesis and stenosis patients in general. Based on their clinical experience, scientific knowledge, and self-convictions, the physiotherapists believed they were doing the best treatment for their patients [20,21,26]. The results of these programs were consent: A multidisciplinary program of group-based task-oriented exercises aimed at managing kinesiophobia was superior to an exercise program of similar duration in reducing disability, fear-avoidance beliefs, catastrophizing and pain, and enhancing the Quality of Life (QoL) of subjects [20,21,26]. The TSK scores were significantly lower in the experimental group than in the control group after the end of the intervention, which was because the CBT program focused on kinesiophobia management, cognitive restructuring, problem-solving, and relaxation training. Moreover, patients were encouraged to take responsibility for their excessive and irrational thoughts, to develop active behaviors, and reduce their perception of pain and disability [20,21,26].
Adopting a CBT mainly aimed at addressing fear-avoidance beliefs proved to is a successful strategy even when group-based, additionally offering the opportunity for peer-group support and encouragement as well as for decentering and challenging beliefs and cognitions. Having explained to the patients how to modify their mistaken fears and encouraged them to adopt appropriate behaviors induced early positive attitudes towards perceived disability; subjects became more comfortable with their usual activities after readjusting their beliefs about the possibility of performing them despite the pain, and this enhanced their positive attitude towards the exercises and increased physical performance [20,21,26].
The significant between-group difference in disability was due to the levels of catastrophizing and kinesiophobia, which improved in the experimental group but remained unchanged throughout the study in the control group, thus representing a major barrier to improved physical performance and disability. About the fear-avoidance model, satisfactory levels were maintained until the end of the follow-up, probably because the patients consolidated appropriate behaviors [20,21,26].
Physiotherapy integrated virtual walking: Cognitive-behavioral therapy specifically exposure therapy, has been suggested in the literature as a useful alternative therapy for reducing pain catastrophizing. Virtual Reality (VR) exposure therapy is a technology that exposes patients to computer-generated images to provide a distraction from the patients’ pain symptoms. VR has been found to reduce the focus on incoming signals from pain receptors, dividing the attention tasks. It also makes it possible to increase movement in patients with kinesiophobia due to chronic pain [22].
The experimental group was asked to passively watch the same virtual walking video clip in a sitting position. For the virtual walking task, a video clip was taken by a cameraman who was naturally walking down Ireland forest at the speed of approximately 1.0 km/h. The patients were asked to imagine as if they were walking, while they were watching the video clip [22].
This study showed that a physical therapy program integrated with virtual walking improved pain, function, and kinesiophobia in patients with LBP. Distraction is one possible analgesic mechanism to reduce anxiety. Watching the movement or just imaging the activity increases motor and premotor cortex activity [22].
The main limitation of the study was they did not use an active treatment option, such as walking, during watching the video. In this study, the patients only watched the video during the hot pack application and did not do any activity. Thus, they were passive. The patients were asked to watch the same video clip for every session, and they reported that they were satisfied, but sometimes, they found watching the same video to be boring [22].
The findings of Yelvar, et al. suggest the short-term effectiveness of physiotherapy program-integrated virtual walking in improving pain, kinesiophobia, and function in patients with non-specific LBP [22].
Postoperative home-exercise: Ilves, et al. developed the Lumbar Spine Fusion (LSF) exercise program, consisted of 12 months of progressive home-based back-specific and aerobic training together with fear-avoidance counseling by a physiotherapist, starting 3 months postoperatively. A physiotherapist gave each patient individual instruction on the exercises by the exercise protocol. The patients exercised independently at home and had booster sessions with the physiotherapist every second month (6 meetings in total) [12].
The participants in the LSF-EX group were also instructed to increase the total number of daily steps during the intervention by walking training, performance of which was encouraged at least 3 times per week [12].
During the booster sessions in physiotherapy, barriers to physical activity, such as kinesiophobia or pain, were identified and discussed with the patient. The physiotherapist sought to allay harmful, irrational beliefs and fears regarding activity and provided additional telephone support when needed. The physiotherapist also reviewed the patient’s experiences regarding the previous phase of the exercise program, instructed the patient in the next phase of the program, and defined the new target number of daily steps (walking training) [12].
The patients in the LSF control group received just one guidance session with a physiotherapist 3 months after surgery. The session consisted of instructions for the standard home exercises. The home exercise program included light muscle endurance exercises, stretching, and balance training. The patients were advised to perform the home exercises 3 times per week [12].
The results of the study showed a slight tendency towards a decrease in fear of movement during the 12-month intervention in the LSF exercise group compared with the LSF control group. The preoperative measurements showed that kinesiophobia was at a high level before the LSF surgery, but had decreased by the 3-month follow-up after surgery. However, participants’ physical activity levels remained unchanged during the first 3 postoperative months [12].
The TSK total score decreased significantly soon after surgery. This was understandable, as pain relief was experienced after surgery. It is also possible that patients’ fear of movement is lessened by the belief that surgery has remedied their lower back problem [12].
Ilves, et al. proposed a cycle, in which the reduction in pain achieved by surgery provided a safe foundation for intensive back-training intervention. As pain and kinesiophobia decreased, physical activity started gradually to increase. The time frame might also explain the increase in physical activity during the intervention in both groups: the first 3 months are the most critical phase in the postoperative healing processes, after which the majority of mobility limitations are removed [12].
In conclusion, the progressive 12-month home exercise program, starting 3 months postoperatively, and including patient education and regular follow-up meetings, was not more effective than usual care after LSF in relieving kinesiophobia or increasing physical activity [12].
Expectation about the condition may or may not affect the outcome-External influences
Surveys of orthopedic surgeons in the United States show that they often discuss fear of reinjury with athletes, and most surgeons agree that athletes with ACL deficiency will be unable to participate in all recreational sporting activities without surgery. The large decrease in kinesiophobia after surgery could also reflect expectations passed between surgeons and patients, with the recommendation for ACL reconstruction influencing patient expectations that surgery is necessary to restore knee stability. Pain studies have shown that outcomes are related to expectations suggested to, or perceived by, the patient. Specifically, better outcomes were observed when there was an expectation that the intervention would be successful and worse outcomes were observed when low expectations were suggested to the patient. Additionally, a social-learning response can occur when one observes a positive response to an intervention [24].
Rehabilitation professionals’ attitudes toward the severity of musculoskeletal conditions and duration of recovery can affect patient fear-avoidance beliefs. For example, among patients with not severe musculoskeletal injuries, a rehabilitation professional may be confident of recovery in a short duration of time and may convey a reassuring message to the patient. When patients view their condition as temporary, they can cause that patients experience less fear of pain related to the activity. This may result in a more confrontational response to the pain and better functional recovery. In contrast, with more severe musculoskeletal injuries, a rehabilitation professional may convey that rehabilitation may not be successful, and the patient may eventually need additional treatments (e.g., surgery) if the symptoms persist. These expectations of more delayed recovery may support the maintenance of fear-avoidance beliefs, which can cause delayed recovery [27].
George, et al. also highlighted that a physiotherapist should identify people with a continued high kinesiophobia level and then address it. Many studies emphasize that psychological response to the initial injury, to surgery, to recovery, and rehabilitation might be an important additional determinant of reintegration into usual activities and returning to sport after surgery. Methods that assess kinesiophobia or re-injury can be implemented in patient assessment in conjunction with a physical assessment before rehabilitation. This can help to identify those at risk of developing potentially maladaptive psychological responses to injury and implement strategies to address these issues [16].
Conclusion
Kinesiophobia is a frequent condition in many musculoskeletal conditions. Is it a concept that has been increasingly studied and approached, recognizing its importance in clinical practice in physiotherapy? Physiotherapists should not neglect their evaluation through the validated TSK tool. Kinesiophobia should be addressed through the CBT program, coupled with the exercise program. The physiotherapist’s expectation of the patient influences the outcome and should always offer support and encouragement.
As with every systematic review, this integrative review has some limitations. In this case, limitations result from selection of the studies, choice of relevant outcome, methods of analysis, interpretation of heterogeneity, and generalization application results.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Butler, David Sheridan, and G. Lorimer Moseley. "Explain Pain 2nd Edn." Noigroup publications, 2013.
- Verwoerd, Annemieke JH, et al. "Does kinesiophobia modify the effects of physical therapy on outcomes in patients with sciatica in primary care? Subgroup analysis from a randomized controlled trial." Physical Therapy, Vol. 95, No. 9, 2015, pp. 1217-23.
- Oksuz, Sevim, and Edibe Unal. "The effect of the clinical pilates exercises on kinesiophobia and other symptoms related to osteoporosis: Randomised controlled trial." Complementary Therapies in Clinical Practice, Vol. 26, 2017, pp. 68-72.
- Vlaeyen, Johan WS, et al. "The role of fear of movement/(re) injury in pain disability." Journal of Occupational Rehabilitation, Vol. 5, No. 4, 1995, pp. 235-52.
- Vlaeyen, Johan WS, et al. "Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance." Pain, Vol. 62, No. 3, 1995, pp. 363-72.
- Er, Goktug, and Ender AngIn. "Determining the relationship of kinesiophobia with respiratory functions and functional capacity in ankylosing spondylitis." Medicine, Vol. 96, No. 29, 2017, p. e7486.
- Akerstrom, Mona-Lisa, Anna Grimby-Ekman, and Mari Lundberg. "Work ability is influenced by kinesiophobia among patients with persistent pain." Physiotherapy Theory and Practice, Vol. 33, No. 8, 2017, pp. 634-43.
- Nijs, Jo, et al. "Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories." Manual Therapy, Vol. 20, No. 1, 2015, pp. 216-20.
- Goldberg, Penny, et al. "Kinesiophobia and its association with health-related quality of life across injury locations." Archives of Physical Medicine and Rehabilitation, Vol. 99, No. 1, 2018, pp. 43-48.
- Maeda, Yoshiki, et al. "Verbal instruction can induce extinction of fear of movement-related pain." The Journal of Pain, Vol. 19, No. 9, 2018, pp. 1063-73.
- Guney-Deniz, Hande, et al. "Does kinesiophobia affect the early functional outcomes following total knee arthroplasty?" Physiotherapy Theory and Practice, Vol. 33, No. 6, 2017, pp. 448-53.
- Ilves, Outi, et al. "Effectiveness of postoperative home-exercise compared with usual care on kinesiophobia and physical activity in spondylolisthesis: A randomized controlled trial." Journal of Rehabilitation Medicine, Vol. 49, No. 9, 2017, pp. 751-57.
- Moseley, Lorimer G. "A new direction for the fear avoidance model?" Pain, Vol. 152, No. 11, 2011, pp. 2447-48.
- Mendes, Karina Dal Sasso, Renata Cristina de Campos Pereira Silveira, and Cristina Maria Galvão. "Integrative review: Research method for incorporating evidence in health and nursing." Text & Context-Nursing, Vol. 17, No. 4, 2008, pp. 758-64.
- Pedro, E. "Scala de PEDro–Português (Portugal) 1. 2009; 1-7."
- Shakeri, Hassan, et al. "Effect of functional lumbar stabilization exercises on pain, disability, and kinesiophobia in women with menstrual low back pain: A preliminary trial." Journal of Chiropractic Medicine, Vol. 12, No. 3, 2013, pp. 160-67.
- Walton, David, and James M. Elliott. "A higher-order analysis supports use of the 11-item version of the tampa scale for kinesiophobia in people with neck pain." Physical Therapy, Vol. 93, No. 1, 2013, pp. 60-68.
- Knapik, Andrzej, Edward Saulicz, and Rafał Gnat. "Kinesiophobia-Introducing a new diagnostic tool." Journal of Human Kinetics, Vol. 28, No. 1, 2011, pp. 25-31.
- Trocoli, Tathiana O., and Ricardo V. Botelho. "Prevalence of anxiety, depression and kinesiophobia in patients with low back pain and their association with the symptoms of low back spinal pain." Brazilian Journal of Rheumatology, Vol. 56, No. 4, 2016, pp. 330-36.
- Cai, Libai, et al. "Does a program based on cognitive behavioral therapy affect kinesiophobia in patients following total knee arthroplasty? A randomized, controlled trial with a 6-month follow-up." The Journal of Arthroplasty, Vol. 33, No. 3, 2018, pp. 704-10.
- Monticone, Marco, et al. "Group‐based task‐oriented exercises aimed at managing kinesiophobia improved disability in chronic low back pain." European Journal of Pain Vol. 20, No. 4, 2016, pp. 541-51.
- Yelvar, Gul Deniz Yilmaz, et al. "Is physiotherapy integrated virtual walking effective on pain, function, and kinesiophobia in patients with non-specific low-back pain? Randomised controlled trial." European Spine Journal, Vol. 26, No. 2, 2017, pp. 538-45.
- Gutke, Annelie, et al. "Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms." European Spine Journal, Vol. 20, No. 3, 2011, pp. 440-48.
- Hartigan, Erin H., et al. "Kinesiophobia after anterior cruciate ligament rupture and reconstruction: noncopers versus potential copers." Journal of Orthopaedic & Sports Physical Therapy, Vol. 43, No. 11, 2013, pp. 821-32.
- Larsson, Caroline, et al. "Kinesiophobia and its relation to pain characteristics and cognitive affective variables in older adults with chronic pain." BMC Geriatrics, Vol. 16, No. 1, 2016, pp. 1-7.
- Monticone, Marco, et al. "Management of catastrophising and kinesiophobia improves rehabilitation after fusion for lumbar spondylolisthesis and stenosis. A randomised controlled trial." European Spine Journal, Vol. 23, No. 1, 2014, pp. 87-95.
- Tichonova, Ana, et al. "The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: A pilot study." Medicina, Vol. 52, No. 4, 2016, pp. 229-37.
- Back, Maria, et al. "Validation of a questionnaire to detect kinesiophobia (fear of movement) in patients with coronary artery disease." Journal of Rehabilitation Medicine, Vol. 44, No. 4, 2012, pp. 363-69.