Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 10
Update of Dermatologic problems in Adults Suffering from COVID-19
Mir Monir Hossain1,2* and Tasmuna Tamrin Tanmy32Department of Pharmacy, University of Science & Technology Chittagong (USTC), Foy’s Lake, Chittagong, Bangladesh
3Department of Anatomy and Neurobiology, College of Medicine, Northeast Ohio Medical University, Rootstown, Ohio, USA
Mir Monir Hossain, Department of Chemistry, Cleveland State University (CSU), Cleveland, Ohio, USA, Email: m.m.hossain39@vikes.csuohio.edu
Received: 28-Sep-2021 Accepted Date: Oct 22, 2021 ; Published: 29-Oct-2021
Abstract
The novel coronavirus (SARS-CoV-2), the cause of Coronavirus 2019 disease (COVID-19) pandemic, is associated with some cutaneous manifestations. This novel disease is associated mostly with significant morbidity and mortality. While the cutaneous presentations of COVID-19 are infrequent, it is of great importance for all clinicians to be aware of these manifestations, as it may contribute to sooner and better diagnosis and management of the disease, even in asymptomatic or paucisymptomatic patients. Although known to primarily cause interstitial pneumonia and respiratory failure, there are several important dermatologic components in adults that clinicians must be aware of. The reported cutaneous manifestations of COVID-19 are various, dispersed, and sometimes confusing. This review aimed to collate and categorize the dermatologic findings reported in adult patients with COVID-19 and identify specific lesions that may facilitate diagnosis and prognostication.
Keywords
COVID-19, Adults, Dermatologic, Skin, Lesion
Introduction
The symptoms of COVID-19 viral disease, generally range from mild to moderate flu-like conditions to critical situations connected with acute respiratory distress syndrome and cytokine storm with decreased adaptive immune response, portending high morbidity and mortality. On 31 December 2019, a newly emerged pneumonia caused by a novel coronavirus, named SARS-CoV-2, was announced by China [1]. It spread out so rapidly until WHO announced Coronavirus 2019 Disease (COVID-19) as a pandemic condition on 11 March 2020. The firstly reported presentations of COVID-19 were like other viral respiratory infections, including high fever and dry cough. However, it might lead to acute respiratory distress syndrome and the mortality rate was quite high [2]. Since then, a wide spectrum of clinical manifestations has been described, ranging from the absence of any symptoms to fever, cough, dyspnea, diarrhea, ageusia, anosmia, and even cutaneous lesions [3,4]. Although the cutaneous manifestations of COVID-19 are infrequent and much of the focus has been on the cardiac and pulmonary complications, it is of great importance for all clinicians to be aware of these presentations, as they may contribute to sooner and better diagnosis and management of the disease, even in asymptomatic or paucisymptomatic patients. This could be a valuable help for epidemiological control of the disease, especially in regions where diagnostic kits are limited [5]. Therefore, cutaneous lesions are likely to have been underestimated for obvious reasons, including the paucity of dermatology consultations in this group of patients [6]. On the other hand, the reported cutaneous manifestations of COVID-19 are various, dispersed, and sometimes confusing. Moreover, the difficulty in determining the actual prevalence of COVID-19-associated skin manifestations has also been linked to the fact that in some countries only patients with respiratory illness or requiring hospitalization are screened [7]. While the majority of patients will experience respiratory complaints with congestion, cough, and shortness of breath, some patients may present without any pulmonary symptoms [8-10].
Recently, there has been increasing recognition of the dermatologic complications of COVID-19. Thus, we aimed to review and summarize the different skin lesions in adults, which have been reported in adult patients associated with COVID-19 to date, in this article. Recent reports from around the world have indicated that this novel coronavirus may be associated with specific cutaneous manifestations. These dermatologic symptoms may be useful in identifying otherwise asymptomatic COVID-19 carriers, which may help slow the transmission of this highly infectious and dangerous virus. As such, an evidence-based review of peer-reviewed scientific literature was conducted to collect clinically relevant information on the cutaneous signs and symptoms of patients with COVID-19.
Main dermatological signs in adult subjects with COVID-19 include (1) urticaria, (2) maculopapular exanthem, (3) papulovesicular exanthem, (4) chilblain-like acral lesions, (5) livedo reticularis or racemosa, (6) purpuric vasculitis. Mostly every dermatological problem may be noticeable at phases of the prodromal, active, or convalescent of COVID-19 disease [11]. SARS-CoV-2 can specifically be responsible for various cutaneous manifestations via direct viral binding or secondarily through various allergic-immunologic mediated processes [12]. Normally SARS-CoV-2 binding to the Angiotensin-Converting Enzyme 2 (ACE2) receptor facilitates viral entry into epithelial cells, primarily in the upper respiratory mucosa. Again, the ACE2 receptor is expressed in the cutaneous or subcutaneous and vascular tissues and thus may contribute to dermatologic problems in SARS-CoV-2 infection [13]. The dermatological signs of COVID-19 can be classified as (1) the viral exanthems, which is an immune response to viral nucleotides, or (2) the systemic immunologic consequences of SARS-CoV-2 such as vasculopathy or micro-thrombotic skin lesions [6]. The Viral exanthems include urticaria or angioedema, maculopapular or morbilliform rashes, vesicular eruptions, and erythema multiforme. The Vasculitic-type lesions include acral lesions, sacral ulcerations, purpuric lesions, and vasculitis. Moreover, evidence directs that cytokine release, coagulation pathway disturbance, and complementmediated microvascular injury play a role in the pathology of this latter group. Medication-caused hypersensitivity exanthems and petechiae in case of acquired thrombocytopenia represent other cutaneous problems.
Methods
This review outlines the underlying pathophysiology and dermatologic manifestations specifically of adult patients having COVID-19. A literature review of the Scifinder, PubMed, and Google Scholar databases was performed from the beginning to 07 February 2021, for articles using the keywords COVID-19, SARS-CoV-2, dermatologic, adult patients, and skin for generation of this review article. In this case, authors included case reports and series, retrospective and prospective studies, systematic reviews and meta-analyses, clinical guidelines, narrative reviews, commentaries, and letters.
Results and Discussion
Pathophysiology and Clinical Presentations
SARS-CoV-2 is an RNA virus that may enter cells through the Angiotensin-Converting Enzyme 2 (ACE2) receptor found on lung alveolar epithelial cells, small intestine enterocytes, and vasculature, as well as neurologic, endocrine, and cardiac systems [14,15]. ACE2 plays several key roles in normal physiology, including a breakdown of angiotensin II [15]. SARS-CoV-2 may cause direct lung injury and systemic inflammation, as well as increased coagulation [16- 18]. These factors can result in multi-organ dysfunction. Recent literature suggests ACE2 is also located in the skin, which may explain some of the dermatologic manifestations in the setting of COVID-19 infection [13].
Dermatological Manifestations in Adults
Although the most common symptoms of COVID-19 include congestion, cough, dyspnea, and fever, skin symptoms can occur in up to 21% of patients [19]. One early study found that only 2 of 1099 patients had a “rash”, but investigators may have missed several patients [8]. A more recent study found rash occurred in 20 of 91 patients, with 8 of these patients having rash at onset, while another study found that rash occurred in 6 out of 108 patients [7]. A rash associated with COVID-19 can involve various body regions, most commonly the trunk, but extremity involvement may also occur. Pruritus is often minimal but depends on the type of rash, and lesions typically heal quickly, appearing within 3 days and disappearing within 8 days.
Urticaria and Angioedema
Urticaria exhibits a histamine-caused reaction due to cutaneous mast cell degranulation, which is characterized by circumscribed wheals with surrounding erythema, localized, scattered, or generalized in distribution. Again, angioedema with histamine-caused may accompany urticaria or occur in isolation, representing deeper dermal edema. Urticaria with or without angioedema in the setting of confirmed or highly suspected COVID-19 infection has been observed in several reports and case series [7,19]. Most likely other viral infections, the urticarial rash may occur concurrently with COVID-19 systemic signs (fever, cough) and last for several days [20,21]. Broad-scale studies suggest that urticaria is highly connected with severe COVID-19 disease, although case reports recount otherwise. Moreover, acute urticaria may occur in asymptomatic or subclinical SARS-CoV-2 infection.
Maculopapular Rash
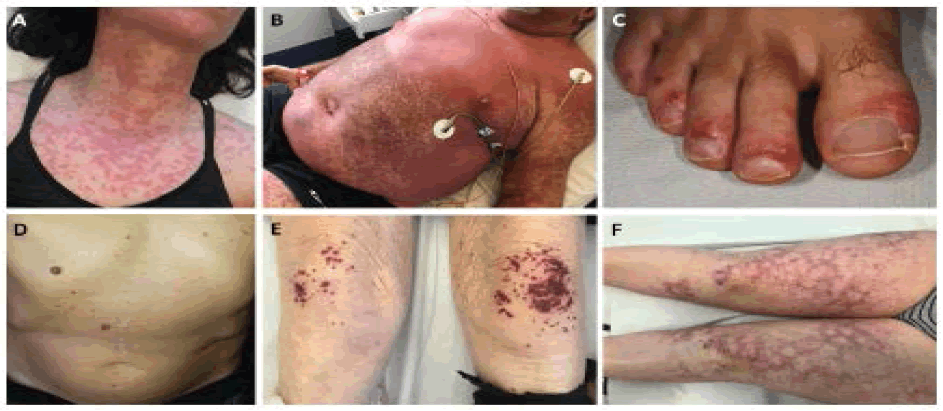
There are multiple reports of patients presenting with a maculopapular rash, characterized by erythematous macules covered with small papules, or with large plaques (Figure 1) [22,23]. The rash may also be perifollicular and associated with scaling and confluence, which may cause it to be mistaken for pityriasis rosea [24]. This type of rash has been suggested to have a mean duration of approximately 9 days [24]. One study of 88 patients in Italy found that a maculopapular rash was present in 14 patients (16%) [19].
Vesicular Eruption
Vesicular eruptions or rashes are usually expressed as small and fluid-filled lesions. Vesicular eruptions with distinct monomorphic lesions occur mainly on the trunk or limbs; those were observed in 9% of cases [24]. Most lesions were pruritic, appeared before the onset of other COVID-19 symptoms in 15% of cases, and usually lasted for a mean of about 10 days. A case series on 22 patients with varicella-like papular-vesicular lesions and confirmed SARSCoV- 2 infection [25]. The majority were middle-aged adult men with non-pruritic to mildly pruritic scattered lesions presented on the trunk that showed a median of 3 days after onset of systemic COVID-19 symptoms; the mortality rate was 13.6% [25].
Chilblains
Chilblains (also known as pernio or perniosis) are an abnormal response to cold, wherein distal arteries and veins constrict, which can lead to pruritic and tender wounds on the extremities. Patients can present with erythematous or violaceous papules and macules, bullae, or digital swelling [26]. This has been increasingly recognized in association with COVID-19. There have been nearly 100 cases of chilblains associated with COVID-19 already described in the literature [23,27]. Still, the pathogenesis of acral chilblain-like lesions remains unclear. But various proposed mechanisms include cutaneous microthrombi, acquired coagulopathy, or CD8+ T lymphocyte endothelial cell cytotoxicity.
Livedo Racemosa
Normally, Livedo Reticularis or racemose (LR) is known by a mottled, lace- or net-like vascular pattern of erythematous which is associated with mild to moderate ischemia of the cutaneous capillaries. By comparing with other cutaneous findings in COVID-19, livedo reticularis is less common (2.3%) but associated with more severe disease and possibly has greater mortality [28]. The livedo eruptions are described in multiple case reports prominently due to inflammation caused by SARS-CoV-2 binding to vascular endothelium. Patients may be at risk for massive systemic thromboembolic cases and multi-organ connections [29]. One series of 21 cases found that the rash had a mean duration of 9.4 days [24]. LR was more common in older patients, with a mean age of 63 years [24]. LR was also associated with a more severe disease (10% mortality rate) [24].
Vasculitis
Vesicular rashes include small, fluid-filled blisters, often on an erythematous base. Numerous case reports have documented vesicular rashes in patients with COVID-19, with the study by Recalcati, et al. finding vesicles in 1.1% of patients [19]. Vesicles are more commonly scattered, rather than diffuse in appearance, with one series finding scattered lesions in 16 of 22 patients and diffuse lesions in the remaining 06 patients [25]. Other case reports have described the appearance of vesicles, with one discussing diffuse involvement of the face and limbs in an 8-year-old [23,30]. A separate case series found that the vesicular rash occurred for a mean duration of 10.4 days, with vesicles appearing mostly on the trunk and extremities.
Sacral Ulcer
“Sacral ulcer” shows a peculiar finding in adult patients with COVID-19. Several risk factors for the development of sacral decubitus ulcers include immobility and prolonged bed rest, incontinence, malnutrition, diabetes, and vascular disease. The sacral ulcer may represent purpuric lesions, violaceous induration, livedoid plaques, and eschars. The pathogenesis is assumed to be multifactorial including a combination of systemic coagulopathy, cutaneous ischemia, and pressure-induced deep tissue injury. The cases of sacral ulcers in old patients with critically ill, multi-organ system COVID-19 disease [31].
Distal Ischemia and Necrosis
For adult patients having COVID-19, one of the most severe complications includes distal ischemia resulting in tissue necrosis. One case study described seven patients with acro-ischemia including finger and toe cyanosis, skin bullae, and dry gangrene [32]. Another report of two patients described the appearance of red and purple papules on the distal fingers due to distal ischemia, which occurred before the appearance of other symptoms [33]. Other case reports describe a 13-year-old with distal toe ischemia presenting with blistering and necrosis, as well as one patient with necrotic purpura [23,34]. Given the coagulopathic impact of SARS-CoV-2, these findings necessitate discussion with vascular surgery specialists and consideration of intravenous thrombolytics.
Conclusion
Adult patients with COVID-19 most commonly present with respiratory symptoms, but multi-organ involvement can occur, with multiple skin manifestations. In conclusion, we can say that SARS-CoV-2 has been connected with several different dermatological manifestations, likely of varying pathophysiology, some preceding COVID-19 symptomatology and others occurring during active involvement of disease or later in the progression. Adult subjects having COVID-19 cutaneous presentations may demonstrate a range of illnesses. These dermatological rashes should trigger consideration of COVID-19, and understanding these manifestations is important to help identify potential COVID-19 patients and properly treat complications. We believe modern handful research and updated reporting will more precisely determine the incidence, underlying pathophysiology, potential prognostication, and best treatment options of dermatological manifestations in COVID-19 disease.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Phelan, Alexandra L., Rebecca Katz, and Lawrence O. Gostin. "The novel coronavirus originating in Wuhan, China: Challenges for global health governance." JAMA, Vol. 323, No. 8, 2020, pp. 709-10.
- Li, Qun, et al. "Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia." New England Journal of Medicine, Vol. 382, 2020, pp. 1199-207.
- Rothan, Hussin A., and Siddappa N. Byrareddy. "The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak." Journal of Autoimmunity, Vol. 109, 2020, p. 102433.
- Lechien, Jerome R., et al. "Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study." European Archives of Oto-Rhino-Laryngology, Vol. 277, No. 8, 2020, pp. 2251-61.
- Usher, AD. "COVID-19: Learning from experience." Lancet (London, England), Vol. 395, 2020, p. 1011.
- Suchonwanit, Poonkiat, Kanchana Leerunyakul, and Chaninan Kositkuljorn. "Cutaneous manifestations in COVID-19: Lessons learned from current evidence." Journal of the American Academy of Dermatology, Vol. 83, No. 1, 2020, p. e57.
- Hedou, M., et al. "Comment on “Cutaneous manifestations in COVID‐19: A first perspective” by Recalcati S." Journal of the European Academy of Dermatology and Venereology, 2020.
- Guan, Wei-jie, et al. "Clinical characteristics of coronavirus disease 2019 in China." New England Journal of Medicine, Vol. 382, No. 18, 2020, pp. 1708-20.
- Long, Brit, et al. "Cardiovascular complications in COVID-19." The American Journal of Emergency Medicine, Vol. 38, No. 7, 2020, pp. 1504-07.
- Bridwell, Rachel, Brit Long, and Michael Gottlieb. "Neurologic complications of COVID-19." The American Journal of Emergency Medicine, Vol. 38, No. 7, 2020, p. 1549.e3.
- Rahimi, Hoda, and Zohreh Tehranchinia. "A comprehensive review of cutaneous manifestations associated with COVID-19." BioMed Research International, Vol. 2020, 2020.
- Criado, Paulo Ricardo, et al. "Are the cutaneous manifestations during or due to SARS-CoV-2 infection/COVID-19 frequent or not? Revision of possible pathophysiologic mechanisms." Inflammation Research, Vol. 69, 2020, pp. 745-56.
- Li, Meng-Yuan, et al. "Expression of the SARS-CoV-2 cell receptor gene ACE2 in a wide variety of human tissues." Infectious Diseases of Poverty, Vol. 9, No. 1, 2020, pp. 1-7.
- Hamming, Inge, et al. "Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis." The Journal of Pathology: A Journal of the Pathological Society of Great Britain and Ireland, Vol. 203, No. 2, 2004, pp. 631-37.
- Zhang, Haibo, et al. "Angiotensin-Converting Enzyme 2 (ACE2) as a SARS-CoV-2 receptor: Molecular mechanisms and potential therapeutic target." Intensive Care Medicine, Vol. 46, No. 4, 2020, pp. 586-90.
- Huang, Chaolin, et al. "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China." The Lancet, Vol. 395, No. 10223, 2020, pp. 497-506.
- Zhou, Fei, et al. "Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study." The Lancet, Vol. 395, No. 10229, 2020, pp. 1054-62.
- Wang, Dawei, et al. "Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China." JAMA, Vol. 323, No. 11, 2020, pp. 1061-69.
- Recalcati, Sebastiano. "Cutaneous manifestations in COVID-19: A first perspective." Journal of the European Academy of Dermatology and Venereology, Vol. 34, No. 5, 2020.
- Henry, D., et al. "Urticarial eruption in COVID‐19 infection." Journal of the European Academy of Dermatology and Venereology, Vol. 34, No. 6, 2020, pp. e244-45.
- Van Damme, C., et al. "Acute urticaria with pyrexia as the first manifestations of a COVID‐19 infection." Journal of the European Academy of Dermatology and Venereology, 2020.
- Sanchez, Adrien, et al. "Digitate papulosquamous eruption associated with severe acute respiratory syndrome coronavirus 2 infection." JAMA Dermatology, Vol. 156, No. 7, 2020, pp. 819-20.
- Bouaziz, J. D., et al. "Vascular skin symptoms in COVID-19: A french observational study." Journal of the European Academy of Dermatology and Venereology, Vol. 34, No. 9, 2020, pp. e451-52.
- Casas, C. Galván, et al. "Classification of the cutaneous manifestations of COVID‐19: A rapid prospective nationwide consensus study in Spain with 375 cases." The British Journal of Dermatology, 2020.
- Marzano, Angelo Valerio, et al. "Varicella-like exanthem as a specific COVID-19-associated skin manifestation: Multicenter case series of 22 patients." Journal of the American Academy of Dermatology, Vol. 83, No. 1, 2020, pp. 280-85.
- Recalcati, S., et al. "Acral cutaneous lesions in the time of COVID‐19." Journal of the European Academy of Dermatology and Venereology, Vol. 34, No. 8, 2020, pp. e346-47.
- Landa, Nerea, et al. "Chilblain‐like lesions on feet and hands during the COVID‐19 pandemic." International Journal of Dermatology, Vol. 59, No. 6, 2020, pp. 739-43.
- Chibane, Sarah, et al. "Hyperacute multi-organ thromboembolic storm in COVID-19: A case report." Journal of Thrombosis and Thrombolysis, Vol. 51, 2021, pp. 25-28.
- Gianotti, Raffaele, et al. "Histopathological study of a broad spectrum of skin dermatoses in patients affected or highly suspected of infection by COVID-19 in the northern part of Italy: Analysis of the many faces of the viral-induced skin diseases in previous and new reported cases." The American Journal of Dermatopathology, Vol. 42, No. 8, 2020, pp. 564-70.
- Genovese, Giovanni, Cristiana Colonna, and Angelo V. Marzano. "Varicella‐like exanthem associated with COVID‐19 in an 8‐year‐old girl: a diagnostic clue?" Pediatric Dermatology, Vol. 37, No. 3, 2020, pp. 435-36.
- Young, Sarah, et al. "Large sacral/buttocks ulcerations in the setting of coagulopathy: A case series establishing the skin as a target organ of significant damage and potential morbidity in patients with severe COVID‐19." International Wound Journal, Vol. 17, No. 6, 2020, pp. 2033-37.
- Zhang, Y., et al. "Clinical and coagulation characteristics in 7 patients with critical COVID-2019 pneumonia and acro-ischemia." Zhonghua xue ye xue za zhi= Zhonghua xueyexue zazhi, Vol. 41, No. 4, 2020, pp. 302-07.
- Alramthan, A., and W. Aldaraji. "A case of COVID-19 presenting in clinical picture resembling chilblains disease: First report from the Middle East.” Clinical and Experimental Dermatology, Vol. 45, 2020, pp. 746-48.
- Mazzotta, F., and T. Troccoli. "Acute acro-ischemia in the child at the time of COVID-19." European Journal of Pediatric Dermatology, Vol. 30, No. 2, 2020, pp. 71-74.