Research Article - International Journal of Medical Research & Health Sciences ( 2023) Volume 13, Issue 4
Usage of HbA1c as a Marker to Assess Progression of COVID-19
Gamal Lotfy, Sherif Sabri*, Mohamed Abo Hamila and Ahmed YassienSherif Sabri, Department of Critical Care Medicine, Beni Suef University, Beni Suef, Egypt, Email: Dr_sabri@hotmail.com
Received: 29-Nov-2022, Manuscript No. IJMRHS-22-81643; Editor assigned: 01-Dec-2022, Pre QC No. IJMRHS-22-81643 (PQ); Reviewed: 15-Dec-2022, QC No. IJMRHS-22-81643; Revised: 27-Mar-2023, Manuscript No. IJMRHS-22-81643 (R); Published: 03-Apr-2023
Abstract
Objective: To assess the impact of diabetes on the course of COVID-19 disease in critically ill patients by measuring HbA1c in the first 48 hours of admission and follow-up severity of the disease.
Background: Poor glycemic management has been linked to increased mortality from previous viral pandemics, including H1N1 flu and SARS. Incorporating diabetes status assessment into risk management for COVID-19 patients is currently proposed by many investigations.
Methods: A retrospective cohort study was conducted on 40 critically ill patients during the period from October 2021 to April 2022 on patients admitted to the critical care department in Beni-Suef university hospital. HbA1c was measure at first 48 hours from admission.
Results: This study was conducted on 40 patients. Overall, 50% of the participants were diabetic and 62.5% were hypertensive. There was a significant association between the higher HbA1c level (>8.7) and need to mechanical ventilation, higher length of stay in ICU and the mortality in diabetic patients. The HbA1c had a statistically significant role in prediction of need to MV in diabetic group. At a cut off 8.7, HbA1c can predict the need to MV with 91% sensitivity and 63% specificity in diabetic patients. Likewise, the HbA1c had a statistically significant role in prediction of mortality in diabetic group. At a cut off 8.5, HbA1c can predict the mortality with 90.9% sensitivity and 89% specificity in diabetic patients.
Conclusion: HbA1c has a high sensitivity and acceptable specificity in terms of predicting the mortality in diabetic patients with COVID-19.
Keywords
Diabetes, HbA1c, COVID-19, Adverse outcomes, Mechanical ventilation
Introduction
The 2019 Coronavirus Disease (COVID-19), caused by the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2), has emerged as a significant health concern throughout the world [1-3]. In order to direct physicians to carry out targeted treatment, it is vital to identify the risk factors linked with the progression of COVID-19. Recently, it has been shown that a number of demographic and clinical factors might help with the risk stratification of the disease [4-6].
Poor glycemic management has been linked to increased mortality from previous viral pandemics, including H1N1 flu and SARS [7,8]. Incorporating diabetes status assessment into risk management for COVID-19 patients is currently proposed by many investigations. The glycosylated hemoglobin (HbA1c) test gives a reliable three months average of glucose levels [9]. To determine those at high risk for developing COVID-19 who are unaware of their condition, this test may be used to evaluate their current diabetes status [10]. Unlike other risk factors for COVID-19 related mortality, such as older age, HbA1c may be modified by health care interventions and is widely accessible in routine practice [11]. This suggests that HbA1c might be utilized for a quick and accurate evaluation of COVID-19 risk. Several studies have indicated that HbA1c is independently linked with hospital mortality [12-14]. However, it is still unknown how HbA1c relates to severe COVID-19 in both diabetics and non-diabetics. Therefore, further studies are required to investigate the predictive value of HbA1c for adverse prognosis in patients with COVID-19. This study aimed to assess the impact of diabetes on the course of COVID-19 disease in critically ill patients by measuring HbA1c in the first 48 hours of admission and follow-up severity of the disease.
Materials and Methods
The study gained ethical clearance from the responsible committee in the faculty of medicine, Beni-Suef university. Due to the retrospective nature of the study, the need for informed consent was waived.
Subjects
We performed a retrospective cohort study on 40 critically ill patients; 20 cases with diabetes exposure either chronic or recently discovered and 20 free of diabetes. The study was conducted during the period from October 2021 to April 2022 on patients admitted to the critical care department in Beni-Suef university hospital. We included moderate cases of COVID-19 patients, defined by a SpO2 reading of less than 94 percent on room air at sea level and evidence of lover respiratory by clinical examination or imaging. We excluded cases with severe illness at presentation and cases at high risk of mortality as defined by APACHE ll.
Methods
The following data were collected from every patient: Age, gender, history of chronic diseases, renal and hepatic function tests, coagulation profile, ABG, pulmonary function tests, SpO2, inflammatory markers C-Reactive Protein (CRP), D-dimer, serum ferritin and Total Leucocytic Count (TLC), APACHE II score and COVID-19 Reporting and Data System (CO-RADS) from baseline to 10 days of admission. The HbA1c data was collected in the first 48 hours of ICU admission measured by Beckman Coulter device version AU480. Outcomes of the patients were also collected, including the need for mechanical ventilation and in hospital mortality.
Statistical analysis
Retrieved data were summarized and processed with IBM SPSS statistical software (version 25). Frequencies were used to describe categorizes and numeric were summarized into median (range). The hypothesize of significant associations between various parameters and HbA1c was tested by Chi-square test for categorical variables and Mann-Whitney test for continuous variables. The prediction utilities of HbA1c were investigated by receiver operator characteristic and the outputs were presented diagnostic accuracy measures. P-value<0.05 was regarded as statistically significant.
Results
This study was conducted on 40 patients with confirmed COVID-19 to assess the impact of diabetes on course of COVID-19 disease in critically ill patients by measuring of HbA1c in first 48 hours of admission and follow up severity of the disease. The mean age of the studied patients was 60.2 ± 14.5 years and 47.5% were females. Overall, 50% of the participants were diabetic and 62.5% were hypertensive.
There was no significant difference between diabetic and non-diabetic regarding sex distribution but, diabetic patients were older than non-diabetic. On the other hand, there was a significant increase of serum urea, creatinine, HbA1c, PCO2, APATCHII and ferritin among diabetic than non-diabetic patients. Besides, there was no significant increase CORAD score from the first to the second assessment in non-diabetic but in diabetic group there was a significant increase of CORAD score. There was a significant decrease of the CRP in non-diabetic, but it didn’t change significantly in diabetic patients. Also, there was a significant difference between both groups regarding the CRP at day 10 (P-value<0.05) (Table 1).
| Items | Non-diabetic (no=20) | Diabetic (no=20) | P-value |
|---|---|---|---|
| Age (mean ±SD) | 58.3 ± 14.6 | 66.9 ± 9.4 | 0.032 |
| Sex | |||
| Males | 9 (45.0%) | 12 (60.0%) | 0.342 |
| Females | 11 (55.0%) | 8 (40.0%) | |
| Na | 138.7 ± 5.2 | 135.8 ± 5.2 | 0.084 |
| K | 4.1 ± 0.4 | 4.2 ± 0.6 | 0.227 |
| S Urea | 56.6 ± 9.7 | 108.2 ± 70.2 | 0.017 |
| S Creatinine | 0.9 ± 0.5 | 1.6 ± 1.1 | 0.023 |
| ALT | 47.4 ± 37.6 | 40.8 ± 28 | 0.535 |
| AST | 40.6 ± 31.7 | 45.5 ± 28.9 | 0.606 |
| HbA1C | 5.9 ± 0.8 | 9.5 ± 1.2 | <0.001 |
| PH | 7.4 ± 0.08 | 7.3 ± 0.1 | 0.387 |
| PCO2 | 39.5 ± 6.4 | 47.2 ± 14.1 | 0.034 |
| HCO3 | 24.1 ± 4.9 | 27.4 ± 6.6 | 0.08 |
| PO2 | 80.8 ± 18.4 | 80.1 ± 13.5 | 0.892 |
| FIO2 | 75 ± 18.7 | 83.3 ± 20.2 | 0.187 |
| P/F ratio | 121.3 ± 62 | 103.8 ± 36.5 | 0.283 |
| Sao2 | 87.7 ± 7.2 | 87.9 ± 5.2 | 0.96 |
| ApatchiI | 13.2 ± 4.5 | 20.6 ± 6.3 | <0.001 |
| IL-6 | 75.4 ± 10.7 | 101.4 ± 97.6 | 0.415 |
| LDH | 489.1 ± 232 | 601.3 ± 265.8 | 0.163 |
| TLC | 10.1 ± 4.5 | 8.2 ± 4.4 | 0.188 |
| CRP | 124.3 ± 96.4 | 104.6 ± 102.8 | 0.537 |
| PCT | 0.3 ± 0.2 | 0.6 ± 0.3 | 0.001 |
| D dimer | 2.3 ± 1.3 | 1.7 ± 1.2 | 0.137 |
| Ferritin | 706.7 ± 359.6 | 953.3 ± 169.4 | 0.011 |
| CORAD (on admission) | 4.6 ± 0.8 | 4.5 ± 0.6 | 0.999 |
| CORAD after days | 4.5 ± 0.6 | 4.8 ± 0.4 | 0.082 |
| CRP on the 10th day | 19.6 ± 3.3 | 92.3 ± 9.1 | <0.001 |
There was a significant difference between diabetics and non-diabetic groups regarding the need to mechanical ventilation and length of stay but the mortality was significantly higher in diabetic patients (Table 2).
| Items | Non-diabetic (no=20) | Diabetic (no=20) |
P-value |
|---|---|---|---|
| Need to MV | |||
| No | 18 (90.0%) | 8 (40.0%) | 0.001 |
| Yes | 2 (10.0%) | 12 (60.0%) | |
| Length of stay (mean ± SD) | 13.4 ± 7.2 | 25.4 ± 13.8 | 0.001 |
| Mortality | |||
| Alive | 18 (90.0%) | 9 (45.0%) | 0.002 |
| Died | 2 (10.0%) | 11 (55.0%) | |
Table 3 shows that there was a significant association between the higher HbA1c level (>8.7) and need to mechanical ventilation, higher length of stay in ICU and the mortality in diabetic patients.
| Items | HbA1c<8.7 (no=6) |
HbA1c ≥ 8.7 (no=14) |
P-value |
|---|---|---|---|
| Need to MV | |||
| No | 5 (83.3%) | 3 (21.4%) | 0.018 (FET) |
| Yes | 1 (16.7%) | 11 (78.6%) | |
| Length of stay (mean ± SD) | 16.3 ± 4.8 | 21.3 ± 12.1 | 0.022 |
| Mortality | |||
| Alive | 5 (83.3%) | 4 (28.6%) | 0.024 (FET) |
| Died | 1 (16.7%) | 10 (71.4%) | |
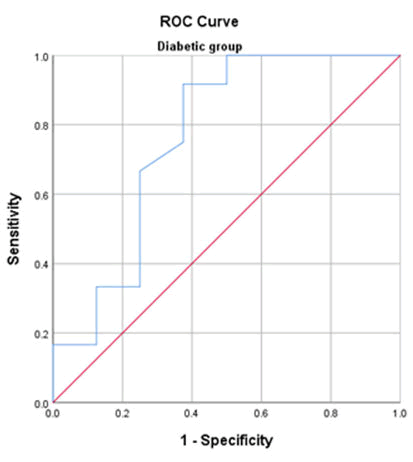
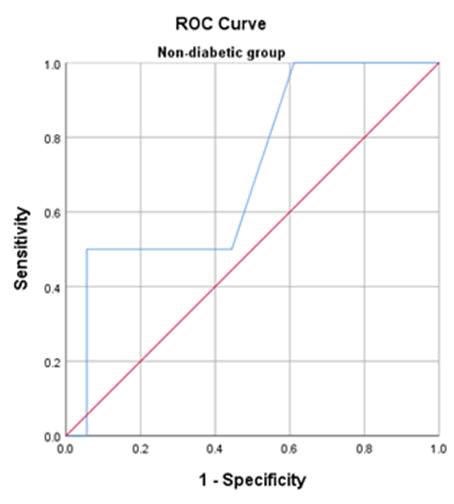
The HbA1c had a statistically significant role in prediction of need to MV in diabetic group. At a cut off 8.7, HbA1c can predict the need to MV with 91% sensitivity and 63% specificity in diabetic patients (Figures 1 and 2).
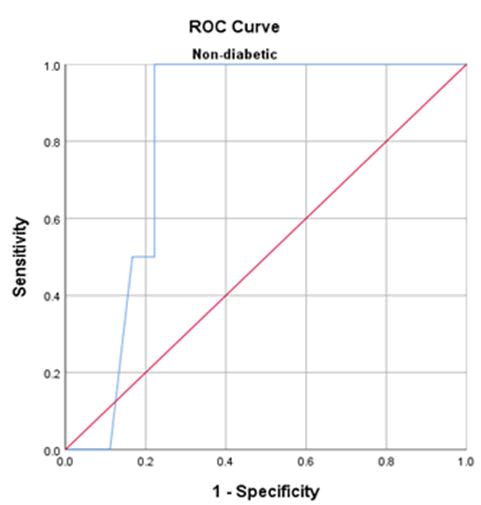
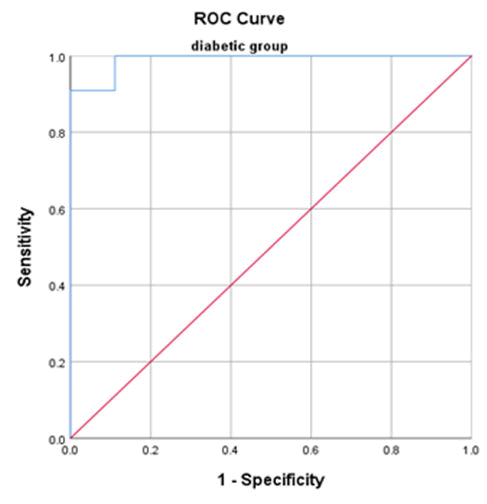
Likewise, the HbA1c had a statistically significant role in prediction of mortality in diabetic group. At a cut off 8.5, HbA1c can predict the mortality with 90.9% sensitivity and 89% specificity in diabetic patients (Figures 3 and 4).
Discussion
In this study, our findings showed that uncontrolled DM, indicated by high levels of HbA1c, was associated with the severity of the disease and high mortality rate. Patients with diabetes who had an HbA1c level of >8.7 were more likely to need mechanical ventilation, have a more prolonged ICU stay, and have a higher rate of mortality. In the diabetic population, HbA1c was a statistically significant predictor of mortality, with a sensitivity of 90.9% and a specificity of 89.1% at a cutoff of 8.5. Moreover, the sensitivity and specificity of HbA1c in predicting the need for mechanical ventilation were 91% and 63%, respectively, at a cutoff value of 8.7.
These findings are consistent with the meta-analysis that was conducted by Shang, et al. who found that DM was related to an elevated risk of severe infection and death in patients with COVID-19 and that diabetic patients with COVID-19 had a greater severe infection and case-Cs compared to non-diabetic patients [15]. Similarly, Guo, et al. reported that in a cohort of COVID-19 patients, those who had diabetes with no other co-morbidities had a higher risk of mortality due to the increased risk of releasing enzymes associated with tissue injury and excessive inflammatory responses and developing severe pneumonia [16]. Uncertainty remains about the mechanism contributing to worse clinical outcomes in COVID-19 individuals with DM. However, some theories attempt to explain this relationship. First, patients with DM may be experiencing chronic inflammation. In diabetic individuals with COVID-19, inflammation indicators such as interleukin-6, erythrocyte sedimentation rate and C-reactive protein are high, which may contribute to a cytokine storm and ultimately, severe pneumonia and mortality [17]. In addition, people with COVID-19 who also have DM may have worse results since DM may promote the hypercoagulable state. Hypercoagulability was more common in diabetic patients with COVID-19 and many critically ill patients with COVID-19 seemed to die of small pulmonary embolisms [18,19]. Furin, a type-1 membrane bound protease in the pro-Protein Convertase Subtilisin/Kexin family (PCSK), is also upregulated in diabetic patients. Furin has a role in entering Coronaviruses into the cell and promoting viral replication [20]. Diabetic patients with hypertension are often prescribed Angiotensin Receptor Blockers (ARBs) and Angiotensin Converting Enzyme Inhibitors (ACEIs), which may increase the expression of ACE2 in tissues, thereby facilitating virus absorption and elevating the risk of severe infection in patients with DM [21].
The Acute Physiology and Chronic Health Evaluation II (APACHE II) score is the most widely used and wellknown effective prediction scoring approach for hospital outcomes among the many similar systems. The APACHE II score is used in most investigations to predict patient outcomes during the first 24 hours of hospitalization [22]. Statistical analysis revealed a substantial difference in APACH II scores between the two groups. Patients with diabetes had a higher score compared to non-diabetic patients. Likewise, Elibol et al. showed that diabetic patients were associated with a higher APACHE II score, which was associated with mortality.
Our findings showed that patients with DM were associated with a higher rate of mechanical ventilation and more extended hospital stay than non-diabetic patients. Zhang, et al. reported that the mean length of hospital stay was 11 days and 1.6% needed ECMO, 11.1% needed invasive mechanical ventilation, 15.9% needed non-invasive ventilation, and 28.6% needed invasive ventilation. Based on these findings, it may be concluded that diabetic patient’s clinical results are less favorable than those without diabetes. The average length of hospital stays due to COVID-19 was substantially longer in patients with uncontrolled DM (16.94 days) compared to patients with controlled DM (13.91 days), according to a study by Bhandari, et al.
Biomarkers are quantitative measurements used clinically for many conditions reflecting pathological development. Different biochemical parameters were used to diagnose and assess the severity of COVID-19, including CRP, Ddimer, ferritin, LDH, TLC, IL-6 and pro calcitonin. Our study showed that the IL-6, LDH, CRP and D-dimer values were elevated in both groups with no statistically significant differences. There were statistically significant differences between both groups regarding ferritin and pro-calcitonin. Alguwaihes, et al. revealed that both groups had comparable values in terms of TLC, LDH, IL-6, CRP, ESR, procalcitonin and D-dimer. On the other hand, ferritin was significantly higher in the diabetic group. Coppelli et al. reported that diabetic patients had worse inflammatory profiles and were associated with a higher D-dimer compared with non-diabetic patients. Inflammatory markers such C-reactive protein, dimer-D and ferritin are elevated in COVID-19, indicating a high grade systemic inflammation, according to Zhou, Pititto and Ferreira, et al. who also emphasized that DM is a low grade inflammatory condition. When serum Na and K were measured, they were within normal limits. The electrolytes did not vary significantly between the two groups. Alguwaihes, et al. found no non-significant variations in blood Na and K levels between diabetic and non-diabetic participants in their investigation. ALT, AST, Urea, and creatinine were used to evaluate renal and liver functions. Regarding the results of the liver function tests, there were no notable variations between the two groups. On the other hand, kidney functions were elevated in diabetic patients and there was a significant difference between both groups, which is supported by Beigmohammadi, et al. Oxygen saturation did not differ significantly between both groups; however, it decreased in both groups and reached 87.9 ± 5.2 for diabetic patients. On the other hand, the mean PCO2 was higher in diabetic patients compared to non-diabetic patients. Bezuidenhout, et al. had the same results in their study about arterial blood gas and acid base abnormalities in COVID-19 intensive care patients. They revealed that most patients had acidemia (pH<7.35) and low oxygen saturation of 88%. Chest CT imaging is a more reliable, feasible and rapid method to diagnose and assess COVID-19 in comparison to RT-PCR, especially in epidemic regions. According to our findings, there was no significant increase in CORADs score from the first to the second assessment in non-diabetic patients, but in the diabetic group, there was a significant increase in CORADs score. Similarly, Bhandari revealed that the CT severity score was significantly higher in the uncontrolled diabetes group than in the controlled diabetes group.
We acknowledge that our study has some limitations including the small sample size and the single center setting, which may hinder the generalizability of our findings. Moreover, we could not conduct a logistic regression analysis based on the patient’s diabetic status.
Conclusion
COVID-19 patients with diabetes were associated with unfavorable outcomes, including prolonged hospitalization, need for mechanical ventilation and high mortality rate. The renal function tests were found to be worse in diabetic patients with COVID-19. HbA1c has a high sensitivity and AUC and acceptable specificity in terms of predicting the mortality in diabetic patients with COVID-19.
References
- Young BE, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA, Vol. 323, No, 15, 2020, pp. 1488-1494.
[Crossref] [Google Scholar] [PubMed]
- Rothe C, et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. New England Journal of Medicine, Vol. 382, No. 10, 2020. pp. 970-971.
[Crossref] [Google Scholar] [PubMed]
- Chen N, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel Coronavirus pneumonia in Wuhan, China: A descriptive study. The Lancet, Vol. 395, No. 10223, 2020, pp. 507-513.
[Crossref] [Google Scholar] [PubMed]
- Abdelgawad HAH, et al. Clinical review of COVID-19; pathogenesis, diagnosis and management. Current Pharmaceutical Design, Vol. 27, No. 41, 2021, pp. 4232-4244.
[Crossref] [Google Scholar] [PubMed]
- AbdelGhaffar MM, et al. Prediction of mortality in hospitalized Egyptian patients with Coronavirus disease-2019: A multicenter retrospective study. PLoS One, Vol. 17, No. 1, 2022, pp. 0262348.
[Crossref] [Google Scholar] [PubMed]
- Omran D, et al. Predictors of severity and development of critical illness of Egyptian COVID-19 patients: A multicenter study. PLoS One, Vol. 16, No. 9, 2021, pp. 0256203.
[Crossref] [Google Scholar] [PubMed]
- Yang JK, et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabetic Medicine, Vol. 23, No. 6, 2006, pp. 623-628.
[Crossref] [Google Scholar] [PubMed]
- Badawi A and Ryoo SG. Prevalence of diabetes in the 2009 influenza A (H1N1) and the Middle East respiratory syndrome Coronavirus: A systematic review and meta-analysis. Journal of Public Health Research, Vol. 5, No. 3, 2016, pp. 733.
[Crossref] [Google Scholar] [PubMed]
- Wang Z, et al. Glycosylated hemoglobin is associated with systemic inflammation, hypercoagulability and prognosis of COVID-19 patients. Diabetes Research and Clinical Practice, Vol. 164, 2020, pp. 108214.
[Crossref] [Google Scholar] [PubMed]
- Liu L, et al. Glycemic control before admission is an important determinant of prognosis in patients with Coronavirus disease 2019. Journal of Diabetes Investigation, Vol. 12, No. 6, 2021, pp. 1064-1073.
[Crossref] [Google Scholar] [PubMed]
- Holman N, et al. Risk factors for COVID-19 related mortality in people with type 1 and type 2 diabetes in England: A population based cohort study. The Lancet Diabetes and Endocrinology, Vol. 8, No. 10, 2020, pp. 823-833.
[Crossref] [Google Scholar] [PubMed]
- Zhu L, et al. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metabolism, Vol. 31, No. 6, 2020, pp. 1068-1077.
[Crossref] [Google Scholar] [PubMed]
- Agarwal S, et al. Preadmission diabetes specific risk factors for mortality in hospitalized patients with diabetes and Coronavirus disease 2019. Diabetes Care, Vol. 43, No. 10, 2020, pp. 2339-2344.
[Crossref] [Google Scholar] [PubMed]
- Cariou B, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: The CORONADO study. Diabetologia, Vol. 63, No. 8, 2020, pp. 1500-1515.
[Crossref] [Google Scholar] [PubMed]
- Shang L, et al. Diabetes mellitus is associated with severe infection and mortality in patients with COVID-19: A systematic review and meta-analysis. Archives of Medical Research, Vol. 51, No. 7, 2020, pp. 700-709.
[Crossref] [Google Scholar] [PubMed]
- Guo W, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metabolism Research and Reviews, Vol. 36, No. 7, 2020, pp. 3319.
[Crossref] [Google Scholar] [PubMed]
- Maddaloni E and Buzzetti R. COVID-19 and diabetes mellitus: Unveiling the interaction of two pandemics. Diabetes Metabolism Research and Reviews, Vol. 36, No. 7, 2020, pp. 33213321.
[Crossref] [Google Scholar] [PubMed]
- Connors JM and Levy JH. Thromboinflammation and the hypercoagulability of COVID-19. Journal of Thrombosis and Haemostasis, Vol. 18, No. 7, 2020, pp. 1559-1561.
[Crossref] [Google Scholar] [PubMed]
- Connors JM and Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood, Vol. 135, No. 23, 2020, pp. 2033-2040.
[Crossref] [Google Scholar] [PubMed]
- Fernandez C, et al. Plasma levels of the proprotein convertase Furin and incidence of diabetes and mortality. Journal of Internal Medicine, Vol. 284, No. 4, 2018, pp. 377-387.
[Crossref] [Google Scholar] [PubMed]
- Aleksova A, et al. Diabetes mellitus and vitamin D deficiency: Comparable effect on survival and a deadly association after a myocardial infarction. Journal of Clinical Medicine, Vol. 9, No. 7, 2020, pp. 2127.
[Crossref] [Google Scholar] [PubMed]
- Tian Y, et al. Dynamic APACHE II score to predict the outcome of intensive care unit patients. Frontiers in Medicine, Vol. 8, 2022, pp. 744907.
[Crossref] [Google Scholar] [PubMed]