Research - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 4
A Cross-Sectional Study to Assess the Prevalence and Risk Factors of Irritable Bowel Syndrome IBS among Medical Students at the University of Hail, Saudi Arabia
Fatmah Alreshidi1*, Munira Abdulkarim Alsammari1, Arin Essa Almallahi1, Kholoud Saud Alshammari1, Ebtehaj Saud Almughais1, Farida Habib Khan1, Sadaf Anwar1, Rana Aboras2 and Dalal Alayed32Department of Community Medicine, Faculty of Medicine, University of Hail, Saudi Arabia
3Department of Family and Community Medicine, College of Medicine and Medical Sciences, Qassim University, Buraydah, Saudi Arabia
Fatmah Alreshidi, Department of Family and Community Medicine, College of Medicine, University of Hail, Hail, Saudi Arabia, Email: f.alreshidi@uoh.edu.sa
Received: 17-Apr-2022, Manuscript No. ijmrhs-22-61058 ; Editor assigned: 19-Apr-2022, Pre QC No. ijmrhs-22-61058 (PQ); Reviewed: 28-Apr-2022, QC No. ijmrhs-22-61058 (Q); Revised: 28-Apr-2022, Manuscript No. ijmrhs-22-61058 (R); Published: 05-May-2022
Abstract
Objectives: Irritable Bowel Syndrome (IBS) is a common chronic function Gastrointestinal (GI) disorder presenting with abdominal pain, bloating, and change in bowel habits. This study aims to assess the prevalence of irritable bowel syndrome in medical students at Hail’s University, Saudi Arabia. Methods: A cross-sectional study on the prevalence of irritable bowel syndrome was distributed among medical students at Hail University in Hail, Saudi Arabia from November to February 2022 involving 308 medical student participants. Results: In 21.5% of the participants have been diagnosed with IBS and 23.9% fit Rome IV criteria for the diagnosis of IBS. Stress with a percentage of 63.9% and lack of exercise at 63.6% are the highest risk factors for IBS. Conclusion: Our result showed there are a small number of medical students are suffering from inflammatory bowel syndrome.
Keywords
Irritable bowel syndrome, Medical students, Risk factors, Rome IV criteria
Introduction
Irritable Bowel Syndrome (IBS) is a common chronic function Gastrointestinal (GI) disorder that affected women more than men 1.5-2:1 at age 20 to 39 [1]. It is characterized by recurrent, chronic abdominal pain due to changes in bowel habit frequency or stool consistency [2]. The alteration of bowel habits in the absence of specified organic substances [3]. The main pathophysiology of its development is not fully understood until now. There is a combination of genetic predisposition, bowel microbial alternation, altered gut-brain interactions, mucosal inflammation, visceral hypersensitivity, and psychosocial aspects that may have also contributed to IBS development [2,4,5]. The lack of objective diagnostic features to identify IBS has restricted its diagnosis to the use of individual medical history. At present, an IBS diagnosis depends on using the Rome IV criteria [6]. The Rome IV criteria are as follows: repeated abdominal pain on average at least 1 day per week during the previous 3 months associated with 2 or more of the following factors: pain related to defecation, change in stool frequency, and appearance. In 2016, the Rome III criteria were updated to Rome IV [7]. In addition, abdominal pain is usually not relieved by defecation; it may remain the same or even increase post-defecation [8]. Multiple risk factors have been strongly associated with IBS progress [9]. Cigarette smoking and alcohol are associated with IBS, but no significant association [10]. All types of stress, whether physical, psychosocial, or psychological stresses are strongly associated with IBS and can affect IBS symptoms [11]. An example of psychological stress anxiety is a risk for recurrent IBS symptoms [12]. Chronic stress also raises the severity of symptoms and leads to a delay in the improvement state in patients with IBS [13]. Dietary factors are the eating habits of the individual and cultures [14]. Understanding the impact of these parameters will improve awareness and provide an effective way to protect against IBS. Prevention is better than treatment. It is evident from the prospective causes of IBS, which this study will explore in detail which these factors. This study is significant as it will aid the researchers to recognize the behaviors and habits that are likely to cause IBS and how they can improve upon them to diminish the risk of this disease [3]. The data collection will be achieved with due consent, and all precautions will be taken to ensure that there is no mental or physical harassment of any person [15].
Therefore, this study aimed to determine the prevalence of IBS and its associated risk factors among medical students at the University of Hail, Saudi Arabia, using the recent Rome IV diagnostic criteria for IBS.
Materials and Methods
A cross-sectional study among medical college students at Hail University College of Medicine, Saudi Arabia was conducted using an electronic questionnaire, which had been distributed through multiple social media apps to Assess the Prevalence and Risk Factors of Irritable Bowel Syndrome IBS among Medical Students at the University of Hail. The data collected was between November and February 2022. The questionnaire has been distributed in Arabic and was taken and validated from the previous study in Riyadh City (Al-Imam Mohammad Ibn Saud Islamic University Riyadh, Saudi Arabia 2020). The questionnaire consisted of three sections. In the first section Sociodemographic data were obtained which included sex, age, educational level, occupation, body mass index, and marital status of the medical students. The second section involved questions concerning IBS clinical data, management, knowledge, and awareness about symptoms, diagnosis, and treatment of IBS. The third section involved questions regarding Personal habits and stress risk factors and the etiology of IBS among medical students by their socio-demographic data of IBS. The consent of participants was obtained at the beginning of the questionnaire. Data were analyzed using IBM Statistical Package for the Social Science version 23 statistical software used to carry out the analysis throughout this study. Logistic regression analysis is the preferred method since the variable of interest is a binary outcome, i.e., whether the student has Inflammatory Bowel Syndrome (IBS) or not. A p-value less than 0.05 was considered statistically significant.
Results
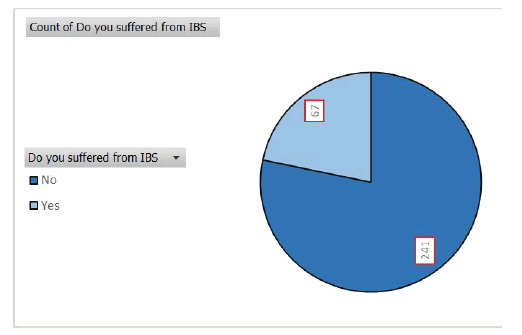
A total of 308 participants completed the questionnaire (Figure 1). Table 1 details the socio-demographic characteristics of the study group. Men comprised 56.5% of the study group, and approximately 54% is between 22 and 25. Most of the study participants are in their clinical years (59%). The majority of the participants were single (97%), living in their family home (73%). About 43% of participants reported a family history of IBS, while 11% of the total sample that they were previously diagnosed by physicians as having IBS.
| Socio-demographic data | Suffered from IBS | ||||||
|---|---|---|---|---|---|---|---|
| Total | Yes | No | |||||
| No | % | No | % | No | % | ||
| Academic phase
|
Pre-clinical | 120 | 39.00% | 28 | 23.30% | 92 | 76.70% |
| Clinical | 181 | 58.80% | 35 | 19.30% | 146 | 80.70% | |
| Intern | 7 | 2.30% | 4 | 57.10% | 3 | 42.90% | |
| Age in years
|
18-21 | 129 | 41.90% | 26 | 20.20% | 103 | 79.80% |
| 22-25 | 165 | 53.60% | 38 | 23.00% | 127 | 77.00% | |
| >25 | 14 | 4.50% | 3 | 21.40% | 11 | 78.60% | |
| Gender
|
Male | 174 | 56.50% | 30 | 17.20% | 144 | 82.80% |
| Female | 134 | 43.50% | 37 | 27.60% | 97 | 72.40% | |
| Body mass index
|
Underweight | 46 | 14.90% | 10 | 21.70% | 36 | 78.30% |
| Normal | 151 | 49.00% | 30 | 19.90% | 121 | 80.10% | |
| Overweight | 76 | 24.70% | 16 | 21.10% | 60 | 78.90% | |
| Obese | 35 | 11.40% | 11 | 31.40% | 24 | 68.60% | |
| Marital status
|
Unmarried | 299 | 97.10% | 64 | 21.40% | 235 | 78.60% |
| Married | 9 | 2.90% | 3 | 33.30% | 6 | 66.70% | |
| Monthly income
|
<5000 SR | 24 | 7.80% | 6 | 25.00% | 18 | 75.00% |
| 5000-10000 SR | 49 | 15.90% | 13 | 26.50% | 36 | 73.50% | |
| 10000-15000 SR | 66 | 21.40% | 7 | 10.60% | 59 | 89.40% | |
| 15000-20000 SR | 71 | 23.10% | 18 | 25.40% | 53 | 74.60% | |
| >20000 SR | 98 | 31.80% | 23 | 23.50% | 75 | 76.50% | |
| Family history of IBS
|
Yes | 133 | 43.10% | 13 | 9.80% | 120 | 90.20% |
| No | 175 | 56.90% | 64 | 36.60% | 111 | 63.40% | |
| Type of own car
|
Don’t have a car | 10 | 3.20% | 5 | 50.00% | 5 | 50.00% |
| Small car | 86 | 27.90% | 18 | 20.90% | 68 | 79.10% | |
| Intermediate care | 192 | 62.30% | 36 | 18.75% | 156 | 81.25% | |
| Big car | 20 | 6.50% | 8 | 40.00% | 12 | 60.00% | |
| Who drive the car
|
Taxi | 11 | 3.60% | 5 | 45.50% | 6 | 54.50% |
| My self | 205 | 66.60% | 33 | 16.10% | 172 | 83.90% | |
| Family member/friend | 45 | 14.60% | 17 | 37.80% | 28 | 62.20% | |
| Private driver | 47 | 15.30% | 12 | 25.50% | 35 | 74.50% | |
| Living with whom?
|
With my family | 225 | 73.10% | 45 | 20% | 180 | 80.00% |
| At students housing | 6 | 1.90% | 1 | 16.70% | 5 | 83.30% | |
| Alone | 56 | 18.20% | 15 | 26.80% | 41 | 73.20% | |
| With friends | 21 | 6.80% | 6 | 28.60% | 15 | 71.40% | |
The prevalence of IBS based on Rome IV criteria in the study was 22% (Table 2). IBS was more prevalent in females than males (28% and 17%). Among IBS subtypes, mixed (16%) and constipation-predominant (24%) subtypes were dominant. Only 31 (41%) of the total 76 cases were previously diagnosed by a physician.
| Clinical data | No | % |
|---|---|---|
| The onset of having IBS | ||
| Before university | 22 | 34.40% |
| During university | 42 | 65.60% |
| Who diagnosed IBS | ||
| Physician | 31 | 47.00% |
| My self | 26 | 39.40% |
| Family | 9 | 13.60% |
| Consulted a doctor specialized in IBS?
|
||
| Yes | 28 | 41.80% |
| No | 39 | 58.20% |
| Received treatment for IBS
|
||
| Yes | 32 | 50% |
| No | 32 | 50% |
| Duration of having treatment
|
||
| No treatment | 35 | 53.00% |
| <3 months | 15 | 22.70% |
| 3-6 months | 6 | 9.10% |
| >6 months | 10 | 15.20% |
| How often have you felt discomfort or pain anywhere in your abdomen?
|
||
| Never | 3 | 4.50% |
| Sometimes | 29 | 43.30% |
| Most times | 27 | 40.30% |
| All times | 8 | 11.90% |
| Have you had this discomfort or pain for 6 months or longer?
|
||
| Yes | 51 | 76.10% |
| No | 16 | 23.90% |
| This pain is accompanied by
|
||
| No pain/Nothing accompanies it | 13 | 19.40% |
| More desire for defecation | 41 | 61.20% |
| Less desire for defecation | 7 | 10.40% |
| Uncontrolled defecation | 6 | 9.00% |
| After defecation, does this pain or discomfort improve or stop?
|
||
| Becomes better | 44 | 65.70% |
| No change/No pain | 19 | 28.30% |
| More worse | 4 | 6.00% |
| For women. Does this pain increases during the menstrual cycle?
|
||
| Yes | 11 | 28.90% |
| No | 27 | 71.10% |
| In the past three months, have you had?
|
||
| Mixed (D&C)
|
11 | 16.40% |
| Diarrhea | 14 | 20.90% |
| Constipation | 16 | 23.90% |
| Urgency for defecation | 18 | 15.70% |
| Sense of incomplete evacuation | 45 | 39.10% |
Regarding Table 3 Personal habits and stress risk factors, about (12%) of participants were smokers, and (36%) practiced physical exercise. This portrays the relationship between IBS and the psychological aspect of participants; 64% of medical students and interns who experienced emotional stress in the 6-months that preceded the study had IBS. After analysis, the table also revealed the prevalence of IBS among participants who had an anxiety problem (prevalence of IBS was 25.3%, 24.0%, and 31.2% among students with severe anxiety, moderate anxiety, or slight).
| Personal habits and stress factors | Suffered from IBS | p-value | |||
|---|---|---|---|---|---|
| Yes | No | ||||
| No | % | No | % | ||
| Sleep duration/day
|
|||||
| <3 hours | 9 | 50.00% | 9 | 50.00% | 0
|
| 3-8 hours | 43 | 18.90% | 184 | 81.10% | |
| >8 hours | 15 | 23.80% | 48 | 76.20% | |
| Smoking duration
|
|||||
| Non-smoker | 54 | 19.90% | 217 | 80.10% | 0.000
|
| <3 years | 3 | 21.40% | 11 | 78.60% | |
| 3-6 years | 4 | 36.40% | 7 | 63.60% | |
| 6-9 years | 3 | 50.00% | 3 | 50.00% | |
| >9 years | 3 | 50.00% | 3 | 50.00% | |
| Do you have bouts of anxiety, stress, or depression?
|
|||||
| Yes | 57 | 28.90% | 140 | 71.10% | 0.000
|
| No | 10 | 9.00% | 101 | 91.00% | |
| If yes, the degree of stress/anxiety
|
|||||
| Slight | 14 | 24.10% | 44 | 75.90% | 0.000
|
| Normal | 7 | 18.40% | 31 | 81.60% | |
| Moderate | 22 | 29.70% | 52 | 70.30% | |
| Severe | 18 | 39.10% | 28 | 60.90%
|
|
| How many hours do you exercise/per day?
|
|||||
| Not practice exercise | 43 | 21.90% | 153 | 78.10% | 0.000
|
| < 1 hour | 3 | 42.90% | 4 | 57.10% | |
| 1-2 hours | 17 | 18.30% | 76 | 81.70% | |
| > 2 hours | 4 | 33.30% | 8 | 66.70% | |
| How many cups of coffee do you drink/day?
|
|||||
| Never / irregular | 14 | 17.90% | 64 | 82.10% | 0.000*
|
| 1-3 cups | 37 | 18.60% | 162 | 81.40% | |
| 3-5 cups | 12 | 54.50% | 10 | 45.50% | |
| > 5 cups | 4 | 44.40% | 5 | 55.60% | |
| Your preferred food
|
|||||
| Proteins | 31 | 22.30% | 108 | 77.70% | 0.000*
|
| Carbohydrates | 30 | 21.70% | 108 | 78.30% | |
| Fruits and vegetables | 2 | 4.00% | 24 | 96.00% | |
| All foods | 4 | 80.00% | 1 | 20.00% | |
| *p<0.05 (significant)
|
|||||
Discussion
The global prevalence of IBS is approximately 11.2% in the general population, which varies regionally [9]. Our study results in a prevalence of 21.5% of IBS among the medical students and interns of Hail University in Hail city, KSA, and 23.9% fit Rome IV criteria for the diagnosis of IBS which is higher than a similar study was done in 2018 in our collage of medicine which reported a prevalence of 18% of medical students are having IBS [16]. In Saudi Arabia 16.3% of medical doctors have IBS and in Jazan Region, Saudi Arabia IBS prevalence was 16% [17,18]. However, our study result is lower compared with a study in Japan 25.2% of the male nursing and medical school students have IBS, and in Nigeria, 26.1% of the medical students are also having IBS [19,20]. In Al-Imam Mohammad Ibn Saud Islamic University Riyadh, Saudi Arabia the prevalence was 35% among medical students who have IBS [21]. In Najran City, Saudi Arabia 39.8% of male secondary school students expressed symptoms suggestive of IBS [22]. The disparity of our results with those of the cited published studies may be attributed to the variability of the study group, diagnostic criteria, age group, and learning environment. The difference in sample size may also be another reason for this difference in disparity. It turns out that IBS is increasing these days not only worldwide but also among medical students of Hail University in Hail city of Saudi Arabia. There was no significant difference in terms of the prevalence of IBS between male and female participants. This result would mean the gender is unrelated to IBS, which is mean everyone can get it. In this study, stress (63.9%) and lack of exercise (63.6%) are the highest risk factors for IBS. This study is confirming that medical students experience increased stress. In this study the habits (stress, sleep duration, lack of exercise, drinking coffee, and type of food show a highly significant association with IBS.
Conclusion
This study reveals a relatively low prevalence (22%) of IBS among medical college students at Hail University College of Medicine. IBS in females was more prevalent than in males (28% and 17%). A significant association was found between depression and anxiety and IBS and between having discomfort or pain and IBS. Those students with anxiety and depression and discomfort or pain for 6 months are more likely to have IBS. The students and smokers were more prone to develop IBS. A new finding suggests that when students have a family history, they also develop IBS. It is advisable to offer students psychological and emotional support to deal with stress and anxiety during their studies.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Lehrer, JK. "Irritable Bowel Syndrome (IBS)." Medscape, 2022.
- Defrees, Dean Nathanial, and Justin Bailey. "Irritable bowel syndrome: Epidemiology, pathophysiology, diagnosis, and treatment." Primary Care: Clinics in Office Practice, Vol. 44, No. 4, 2017, pp. 655-71.
Google Scholar Crossref - Jafri, Wasim, et al. "Frequency of irritable bowel syndrome in college students." Journal of Ayub Medical College Abbottabad, Vol. 17, No. 4, 2005, p. 9.
Google Scholar - Camilleri, Michael, Karen Lasch, and Wen Zhou. "Irritable bowel syndrome: methods, mechanisms, and pathophysiology. The confluence of increased permeability, inflammation, and pain in irritable bowel syndrome." American Journal of Physiology-Gastrointestinal and Liver Physiology, Vol. 303, No. 7, 2012, pp. 775-85.
Google Scholar Crossref - Ng, Qin Xiang, et al. "The role of inflammation in Irritable Bowel Syndrome (IBS)." Journal of Inflammation Research, Vol. 11, 2018, pp. 345-49.
Google Scholar Crossref - Palsson, Olafur S., et al. "Rome IV diagnostic questionnaires and tables for investigators and clinicians." Gastroenterology, 2016.
Google Scholar Crossref - Schmulson, Max J., and Douglas A. Drossman. "What is new in Rome IV." Journal of Neurogastroenterology and Motility, Vol. 23, No. 2, 2017, pp. 151-63.
Google Scholar Crossref - Aziz, Imran, et al. "How the change in IBS criteria from Rome III to Rome IV impacts on clinical characteristics and key pathophysiological factors." Official journal of the American College of Gastroenterology| ACG, Vol. 113, No. 7, 2018, pp. 1017-25.
Google Scholar - Lovell, Rebecca M., and Alexander C. Ford. "Global prevalence of and risk factors for irritable bowel syndrome: A meta-analysis." Clinical Gastroenterology and Hepatology, Vol. 10, No. 7, 2012, pp. 712-21.
Google Scholar Crossref - Sirri, Laura, Silvana Grandi, and Eliana Tossani. "Smoking in irritable bowel syndrome: A systematic review." Journal of Dual Diagnosis, Vol. 13, No. 3, 2017, pp. 184-200.
Google Scholar Crossref - Mayer, Emeran A., et al. "V. Stress and irritable bowel syndrome." American Journal of Physiology-Gastrointestinal and Liver Physiology, Vol. 280, No. 4, 2001, pp. G519-24.
Google Scholar Crossref - Fond, Guillaume, et al. "Anxiety and depression comorbidities in Irritable Bowel Syndrome (IBS): A systematic review and meta-analysis." European Archives of Psychiatry and Clinical Neuroscience, Vol. 264, No. 8, 2014, pp. 651-60.
Google Scholar Crossref - Bennett, E. J., et al. "Level of chronic life stress predicts clinical outcome in irritable bowel syndrome." Gut, Vol. 43, No. 2, 1998, pp. 256-61.
Google Scholar Crossref - Sandler, Robert S., et al. "The burden of selected digestive diseases in the United States." Gastroenterology, Vol. 122, No. 5, 2002, pp. 1500-11.
Google Scholar Crossref - Wang, Ying, et al. "Gender differences in irritable bowel syndrome among medical students at Inner Mongolia Medical University, China: A cross-sectional study." Psychology, Health & Medicine, Vol. 21, No. 8, 2016, pp. 964-74.
Google Scholar Crossref - Alshammari, Omar Mohammad, et al. "Prevalence of irritable bowel syndrome among medical students in Hail University, Saudi Arabia." The Egyptian Journal of Hospital Medicine, Vol. 71, No. 2, 2018, pp. 2581-84.
Google Scholar - AlAmeel, Turki, Lee S. Roth, and Eman Al Sulais. "The prevalence of irritable bowel syndrome among board-certified medical doctors in Saudi Arabia: A cross-sectional study." Journal of the Canadian Association of Gastroenterology, Vol. 3, No. 6, 2020, pp. e32-36.
Google Scholar Crossref - Arishi, Abdulelah M., et al. "Irritable bowel syndrome: Prevalence and risk factors in Jazan Region, Saudi Arabia." Cureus, Vol. 13, No. 6, 2021.
Google Scholar - Okami, Yukiko, et al. "Lifestyle and psychological factors related to irritable bowel syndrome in nursing and medical school students." Journal of Gastroenterology, Vol. 46, No. 12, 2011, pp. 1403-10.
Google Scholar Crossref - Okeke, Edith N., et al. "Prevalence of irritable bowel syndrome in a Nigerian student population." African Journal of Medicine and Medical Sciences, Vol. 34, No. 1, 2005, pp. 33-36.
Google Scholar - Aljasser, Khalid Ahmed, et al. "Prevalence and risk factors of irritable bowel disease among medical students at Al Imam Mohammad Ibn Saud Islamic University Riyadhm, Saudi Arabia." International Journal of Medicine in Developing Countries, Vol. 4, No. 12, 2020, pp. 2038-49.
Google Scholar Crossref - Saad Alshahrani, M. D. "Prevalence and risk factors for irritable bowel syndrome among male secondary school Saudi students in Najran City, Saudi Arabia." The Medical Journal of Cairo University, Vol. 88, 2020, pp. 1917-21.
Google Scholar