Case Report - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 9
Before Biopsy Of A Pulmonary Nodule, Check If It Is Not An Arteriovenous Malformation.
Chirihan Ayadi*, Kaoutar Sefar, Sara Ezzaky, Laila Jroundi and Fatima Zahra LaamraniChirihan Ayadi, Department of Radiology, Hospital Ibn Sina, Mohamed V University, Rabat, Morocco, Email: chirihane.ayadi@gmail.com
Received: 03-Sep-2022, Manuscript No. ijmrhs-22-73664; Editor assigned: 06-Sep-2022, Pre QC No. ijmrhs-22-73664 (PQ); Reviewed: 15-Sep-2022, QC No. ijmrhs-22-73664 (Q); Revised: 19-Sep-2022, Manuscript No. ijmrhs-22-73664 (R); Published: 30-Sep-2022, DOI: 0
Abstract
Pulmonary arteriovenous malformations (AVMs) are relatively rare and are frequently seen in patients with Osler-Weber-Rendu syndrome (ROS). They are often of little or no symptoms but can be the origin of serious complications. The risk of severe complications makes it necessary to detect them in patients with ROS, their diagnosis is made by chest angiostatin, and the treatment of AVMs is done by embolization, which is an efficient and well-tolerated procedure if performed with well-trained hands.
Keywords
Arteriovenous malformation (AVMs), Chest Franciscan, Embolization
Introduction
Pulmonary arteriovenous malformations (AVMs or fistulas) are defined by direct communication between the pulmonary artery(s) and vein(s), without a capillary network, resulting in a right-left shunt [1]. AVMs are rare, affecting approximately 3-5 cases per 100,000 population. They are more prevalent in women with an estimated ratio of 1:1.5 to 1:2 depending on the series. They can be congenital, which is generally associated with Rendu-Osler disease (80%), or acquired in patients with advanced liver cirrhosis, post-trauma, thoracic surgery, infection (like tuberculosis), or tumoral context (metastasis of a thyroid carcinoma) [2].
Case Presentation
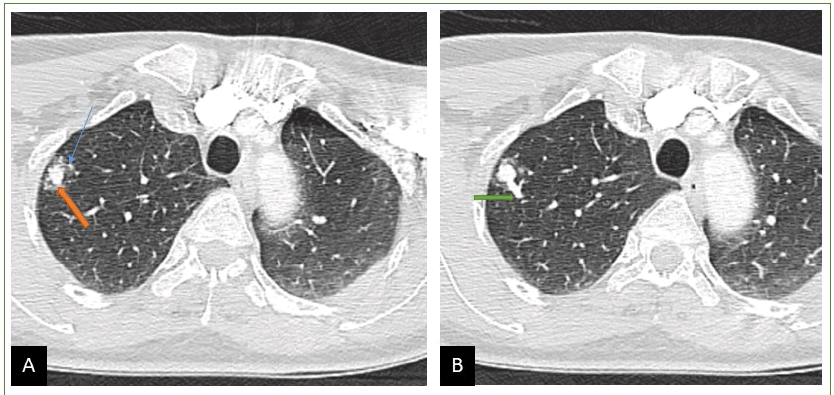
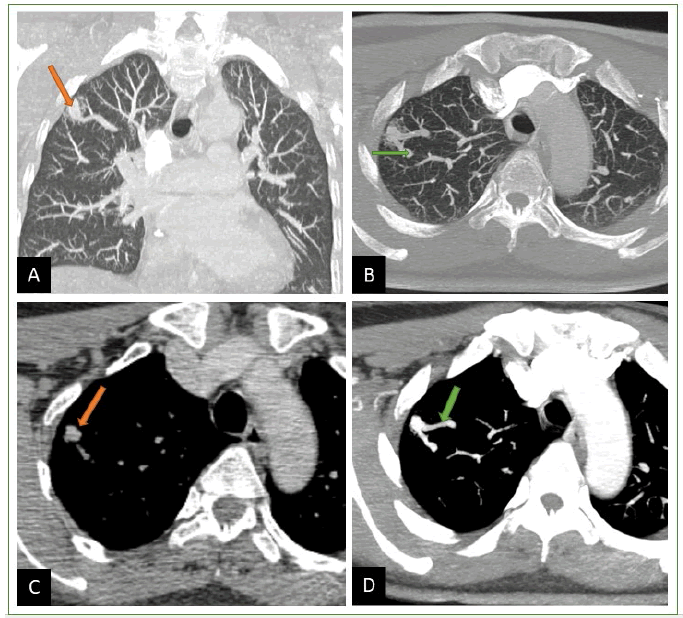
We present the case of a 55-year-old patient, with no previous pathological history, who presented 15 days ago with a fever-free cough, with traces of blood in the sputum, which motivated his consultation. Because of the epidemic context, his doctor evoked Covid 19 pneumopathy, PCR was performed and came back negative, completed by a chest CT scan without injection, which showed a pulmonary nodule, in the upper right lobar, of dense aspect, of irregular contours associated with peripheral ground glass (Figure 1). The patient was referred to our training for biopsy, review of CT scan with multiplanar and MIP reconstructions, and additional injection-oriented diagnosis showing a nodule with double vascular connection (afferent and efferent branch) originating from the upper lobar artery and vein, with opacification of the vascular type at the arterial time, associated with minimal haemorrhage all around (ground glass). The diagnosis of an arteriovenous malformation complicated by a discrete haemorrhage is made based solely on radiological criteria (Figure 2).
Figure 2 A,B) Chest CT using MPR and MIP reconstructions and injection of PDC, showing a dense image with the double vascular connection. C, D) The mediastinal section before and after injection shows enhancement of the aneurysmal sac and afferent and efferent vessels. confirming the diagnosis of an AVM
Discussion
Pulmonary AVMs present a source of hemoptysis and hemothorax with a risk of rupture, paradoxical embolism, or septic emboli that can in rare cases lead to cerebral abscesses [1]. Diagnosis is based on imaging, in particular, a chest angiogram, showing an aneurysmal sac that creates an arteriovenous shunt, known as a right shunt, which is most often between 1 cm and 5 cm and rarely greater than 10 cm. Diagnosis is easy for large AVMs, but small AVMs can present diagnostic challenges with lung nodules as in the case of our patient. AVMs are classified as “ simple “ and “ complex “, and the treatment of choice is based on the percutaneous embolization of AVMs [3]. Pulmonary Hypertension (PH) is considered a relative counterindication to its realization due to the risk of PH aggravation [2,4],
Conclusion
Pulmonary AVMs represent a rare entity that can cause serious complications. They are often associated with DOS, their diagnosis is based on imaging, but can be confused with pulmonary nodules if it is small with the risk of biopsy as in our case. Treatment of AVMs is based on percutaneous embolization.
Declarations
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Blivet, S., P. Lacombe, and T. Chinet. "Pulmonary arteriovenous malformations." Journal of Lung Disease News, Vol. 3, 2011. pp. S61-6.
Google Scholar Crossref - Elhage, Sarah, B. Degano, and T. Soumagne. "Prise en charge d'une malformation arterio-veineuse pulmonaire avec hypertension pulmonaire." Revue des Maladies Respiratoires, Vol. 37, No. 8, 2020, pp. 671-76.
Google Scholar Crossref - Simonneau, Gerald, et al. "Haemodynamic definitions and updated clinical classification of pulmonary hypertension." European Respiratory Journal, Vol. 53, No. 1, 2019.
Google Scholar Crossref - Shovlin, C. L., J. S. R. Gibbs, and J. E. Jackson. "Management of pulmonary arteriovenous malformations in pulmonary hypertensive patients: a pressure to embolise?." European Respiratory Review, Vol. 18, No. 111, 2009, pp. 4-6.
Google Scholar Crossref