Review Article - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 3
Zika Virus: An Update-A Brief Review
M Jaivant1, MS Nandini2*, S Hariharan3 and B Krishna Prasanth42Department of Microbiology, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India
3Department of Community Medicine, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India
4Department of Community Medicine, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India
MS Nandini, Department of Microbiology, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email: drmsnandini@gmail.com
Received: 24-May-2021, Manuscript No. IJMRHS-21-32124; Editor assigned: 27-May-2021, Pre QC No. IJMRHS-21-32124(PQ); Reviewed: 10-Jun-2021, QC No. IJMRHS-21-32124; Revised: 10-Feb-2023, Manuscript No. IJMRHS-21-32124(R); Published: 10-Mar-2023
Abstract
Zika virus is a mosquito borne disease caused by the Flavivirus genus and the Flaviviridae family of arthropod borne viruses (arbovirus). The Zika virus is predominantly transmitted by Aedes aegypti, but the virus can also be transmitted by other Aedes species. In Africa, ZIKV was first isolated from rhesus monkeys in 1947 and from mosquitoes in 1948. For half a century before appearing in the Pacific and the Americas, ZIKV infections in humans were intermittent. ZIKV is normally spread via the bite of mosquitoes that are infected. The clinical presentation of Zika fever, especially those due to arboviruses such as dengue and chikungunya, is unspecific and may be misdiagnosed as other infectious diseases. Before the major french diagnosis, the virus gained the attention of public health authorities because of its strongly suspected relationship with maternal fetal transmission and microcephalus in infected animals. ZIKV infection was only associated with mild disease. Serological diagnosis is complicated by cross reactivity among members of the genus Flavivirus. Moreover, this article will give a brief review on Zika virus epidemic in India.
Keywords
Zika virus, Mosquito borne disease, Flavivirus, Infection
Introduction
The Zika virus is now a global epidemic. Evidence of Zika transmission has been recorded in more than 72 countries and territories since 2007. The transfer of ZIKA has prompted the World Health Organization (WHO) to recognize the situation as a health emergency. This situation is critical because the link between infection during pregnancy and the incidence of microcephaly and Guillain Barre syndrome appears to be highly tangible. The Zika virus is an icosahedral, enveloped, single stranded RNA virus. A virus spread mainly by Aedes mosquitoes causes the Zika virus disease. In February 2016, the WHO declared the Zika virus and its related complications a public health emergency of the international concern. In the United States, Zika virus infection is among the globally notifiable diseases. An unexplained sharp rise in the occurrence of babies born with microcephaly and a summary of a new disease, congenital Zika syndrome, followed the first outbreak of infection with the Zika virus in Brazil [1].
Literature Review
History of Zika virus
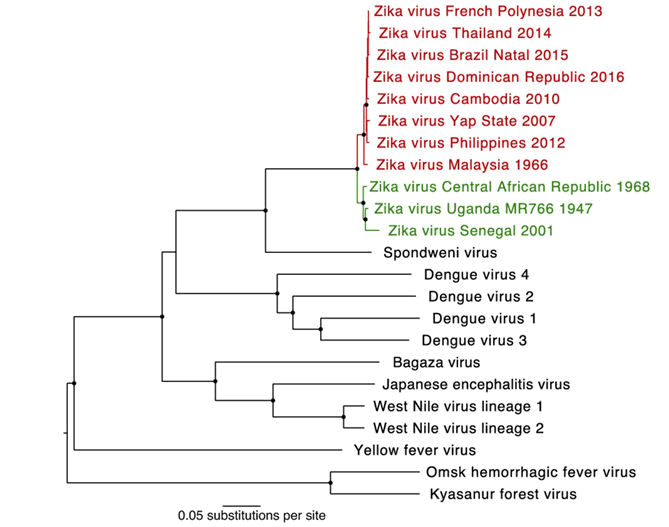
In 1947, the Zika virus was originally discovered in a sentinel rhesus monkey in Uganda's Zika forest. The virus is a member of the Flaviviridae family, the Flavivirus genus, and is spread to humans by mosquitoes of the Aedes group. In 1948 it was isolated from Aedes africanus mosquito; in 1952 the first human cases are detected in Uganda by demonstrating neutralizing antibodies to Zika virus in sera. Geographical distribution of Zika virus expands to Asia, including India, Malaysia and Pakistan from 1969-1983 but in Africa sporadic human cases were detected with mild symptoms without any outbreaks. In 2007, when the virus was associated with a minor outbreak in the Yap Province, part of the Federated States of Micronesia, the first evidence of the Zika virus was outside of Africa and Asia. Since then, infections of the Zika virus have been recorded worldwide, including in Southeast Asia, French Polynesia and the Pacific Islands, and parts of South, Central, and North America. Symptomatic human infection typically results in mild and self-limiting febrile disease, although recent studies have indicated a potential link with more extreme sequelae such as Guillain Barre syndrome and microcephaly during pregnancy in newborn babies of mothers infected with Zika virus. During this 2007 outbreak, 49 confirmed and 59 probable cases of Zika virus infection have been recorded in this outbreak, while an estimated 440,000-1,300,000 cases have been documented in the most recent outbreak in Brazil. The alarming scale of the current outbreak and the potential for autochthonous transmission of this virus in North America and elsewhere have increased understanding of this emerging mosquito trit virus (Figure 1) [2].
Discussion
Epidemiology
Originally, the Zika virus was isolated from a sentinel monkey placed on a platform in the Zika forest near Entebbe, Uganda. In 1947, the first sample from which the Zika virus was isolated was obtained, and in 1948, when the virus was isolated from a pool of Aedes africanus mosquitoes obtained in the same forest, a second isolation of the virus was achieved. Intra cerebral inoculation of the virus to monkeys in one of the five monkeys studied resulted in only moderate fever. High levels of neutralizing antibodies were found in about 6 percent of individuals examined in a concurrent serological survey and antibodies were found in one of 15 monkeys examined. Specimens were taken from a child attending a health clinic in Kampong Speu Province, Cambodia in 2010, which subsequent tests found positive for Zika virus. The child had mild symptoms (fever, sore throat, cough, and headache, but no maculopapular rash) and did not need to be admitted to the hospital. Around this time, no other cases of Zika virus infection were recorded, and this was the only positive non-dengue, non-Japanese encephalitis Flavivirus infection observed, while approximately 10,000 blood and throat swab samples were screened as part of the surveillance programme of US Naval Medical Research Unit [3].
The global prevalence of Zika virus infection has not been widely reported owing to asymptomatic clinical course, clinical resemblance to other infection with other Flaviviruses (dengue, chikungunya), and difficulty in confirming diagnosis. Based on sporadic case reports, entomological surveys and seroprevalence surveys, Zika virus infection had been reported in various hosts, including humans, primates, and mosquitoes, in 14 countries across Africa, Asia, and Oceania, as of 2014. Zika viral infection has been registered in more than 28 countries with the highest number of infections in Brazil in 2016. The latest outbreak in Brazil began in the month of April, in the year 2015. The town of 'Natal,' located in the state of Rio Grande do Norte in the northeast of Brazil, registered the first case of infection with ZIKV. Shortly afterward, virus spread throughout the country and frequent reports of microcephaly coincided with ZIKV infections [4].
Transmission
Zika virus is transmitted to humans mainly through the bite of infected Aedes mosquito species (Ae. aegypti and Ae. albopictus). These are the same mosquitoes which spread dengue and chikungunya viruses. A pregnant woman can transfer Zika virus to her fetus during pregnancy. Zika is a cause of microcephaly and other significant fetal abnormalities of the brain. We're researching the full range of other potential health problems that Zika virus infection can cause during pregnancy. A pregnant woman who has already been infected with Zika virus will transmit the virus to her fetus during pregnancy or around the time of birth. Zika virus has been discovered in breast milk. Possible infections of the Zika virus in breast feeding infants have been reported, but transmission of the Zika virus via breast milk has not been confirmed [5]. In addition, we do not yet know the long term effects of Zika virus on young infants that have been infected after birth. Since existing research shows that the benefits of breastfeeding outweigh the risk of Zika virus transmission by breast milk, CDC tends to encourage mothers to breastfeed, even though they have been infected or lived in or travelled to areas at risk of Zika. Aedes aegypti and Aedes albopictus were recognized as major vectors for transmission of Zika virus. Since then, the infection has spread rapidly to several other countries, becoming a pandemic. The main mode of transmission is through the bite of an infected mosquito, although few sexual transmission events have been reported. The risk of infection depends therefore on the local risk of mosquito borne transmission. It may be high during epidemics, but lower levels of ongoing virus circulation are still expected in areas where ZIKV circulation is considered endemic; in these areas the risk of is low to medium [6-8]. Sexual transmission among humans has also been described. In addition, great concern is emerging over congenital malformations due to trans placental transmission of Zika virus, including microcephaly and various ophthalmic abnormalities. Zika can be passed through sex from a person who has Zika to his or her partners. Zika can be passed through sex, even if the infected person does not have symptoms at the time. There have been several accounts of potential cases of blood transfusion in Brazil. During the French Polynesian outbreak, 2.8% of blood donors tested positive for Zika and in previous outbreaks, the virus was detected in blood donors [9-11].
Pathophysiology
Zika virus is well adapted to grow in various hosts, ranging from arthropods to vertebrates. Viral attachment to unidentified cellular receptors is mediated by the E (Envelope) glycoprotein. This is followed by endocytic uptake and then uncoating of the nucleo capsid and release of viral RNA into the cytoplasm [12-14]. A viral polyprotein is produced and modified by the endoplasmic reticulum. Immature virions collect both in the endoplasmic reticulum and in secretory vesicles before being released [15].
Clinical symptoms
Zika is usually mild with symptoms lasting from days to weeks. People usually don't get sick enough to go to the hospital and very rarely die of Zika. For this reason, many people may not realize that they have been infected. Symptoms of Zika are similar to other viruses transmitted by mosquito bites, such as dengue and chikungunya. Zika virus typically stays in the blood of an infected person for around a week. If you develop symptoms and live in or have recently travelled to a Zika risk location, see your doctor or other health care provider. Your doctor or other health care provider can order a blood or urine test to help decide if you have Zika. If a person is infected, he or she is likely to be safe from potential infections [16-18].
The spectrum of Zika virus disease overlaps with that of arboviral infections, but rash (maculopapular and potentially immune mediated) is usually predominant. Rash in Zika virus infection is typically a fine maculopapular rash that is diffusely dispersed. It can include the face, trunk, and extremities, including palms and soles. Occasionally, the rash may be pruritic. Rash, along with other symptoms, typically develops within 2 weeks of travel to the infected region of the Zika virus. Zika virus rash typically develops in the first week of infection, with infection itself lasting from days to weeks. Zika virus infection should therefore be regarded among individuals with acute myelitis who reside in or travel from endemic areas of Zika virus [19].
Laboratory investigations
Zika virus infection is diagnosed based on the identification and isolation of Zika virus RNA from serum using Reverse Transcriptase Polymerase Chain Reaction (RT-PCR). During the initial week of illness, the greatest sensitivity of PCR testing is marked by high viremia. Serological tests for virus-specific Immunoglobin M (IgM) and anti-Zika virus neutralising antibodies can be performed after the initial week of illness using the Enzyme Linked Immunosorbent Assay (ELISA). Diagnosis of Zika virus infection is generally focused on serological tests, but the CDC is now recommending the tests of urine. Urine can be tested using real time Reverse Transcription Polymerase Chain Reaction (rRT-PCR) samples obtained less than 2 weeks after onset of symptoms [20].
Treatment
There are no specific treatment options for Zika virus infection.
Prevention and control
There is no vaccine for Zika virus. The best way to prevent infection with Zika virus is to avoid travel to areas with active transmission of Zika virus. Residents living in endemic areas or visitors to endemic areas are recommended to prevent mosquito bites.
Conclusion
Various methods to avoid mosquito bites include wearing full sleeved shirts and long pants, sleeping under a mosquito bed sheet, and clothing treatment with permethrin. Mosquito repelling agents such as DEET, picaridin, IR3535, and para-menthane-diol can be used in all age groups except those younger than 2 months for the prevention of mosquito bites. Mosquito larval habitats can be managed by the careful handling of water containers, including routine discarding or covering stagnant water or by the use of larvical agents.
References
- Faye O, et al. Molecular evolution of Zika virus during its emergence in the 20th century. PLOS Negl Trop Dis, Vol. 8, No. 1, 2015, pp. 26-36.
[Crossref] [Google Scholar] [PubMed]
- Dick GW, Kitchen SF, Haddow AJ. Zika virus (I). Isolations and serological specificity. Trans R Soc Trop Med Hyg, Vol. 46, No. 5, 2014, pp. 509-520.
[Crossref] [Google Scholar] [PubMed]
- Bogoch II, et al. Anticipating the international spread of Zika virus from Brazil. Lancet, Vol. 387, No. 10016, 2016, pp. 335-336.
[Crossref] [Google Scholar] [PubMed]
- Gatherer D and Kohl A. Zika virus: A previously slow pandemic spreads rapidly through the Americas. J Gen Virol, Vol. 97, No. 2, 2016, pp.269-273.
[Crossref] [Google Scholar] [PubMed]
- Kelser EA. Meet dengue's cousin, Zika. Microbes Infect, Vol. 18, No. 3, 2015, pp. 163-166.
[Crossref] [Google Scholar] [PubMed]
- Attar N. Zika virus circulates in new regions. Nat Rev Microbiol, Vol. 14, No. 2, 2016, pp. 62.
- Dick GW, Kitchen SF and Haddow AJ. Zika virus (II): Pathogenicity and physical properties. Trans R Soc Trop Med Hyg, Vol. 46, No. 5, 1952, pp. 17-19.
[Crossref] [Google Scholar] [PubMed]
- Heang V, et al. Zika virus infection, Cambodia, 2010. Emerg Infect Dis, Vol. 18. No. 2, 2012, pp. 349.
[Crossref] [Google Scholar] [PubMed]
- Henderson BE, Hewitt LE and Lule M. Serology of wild mammals. Annu Rev Virol, Vol. 3. No. 4, 1968, pp. 48-51.
- Driggers RW, et al. Zika virus infection with prolonged maternal viremia and fetal brain abnormalities. N Engl J Med, Vol. 374, No. 22, 2016, pp. 2142-2151.
[Crossref] [Google Scholar] [PubMed]
- Musso D, et al. Potential sexual transmission of Zika virus. Emerg Infect Dis, Vol. 21, No. 2, 2015, pp. 359.
[Crossref] [Google Scholar] [PubMed]
- Hills SL. Transmission of Zika virus through sexual contact with travelers to areas of ongoing transmission continental United States, 2016. Morb Mortal Wkly Rep, Vol. 5, No. 4, 2016, pp. 65.
[Crossref] [Google Scholar] [PubMed]
- Meaney Delman D, et al. Prolonged detection of Zika virus RNA in pregnant women. Obstet Gynecol, Vol. 128, No. 4, 2016, pp. 724-730.
[Crossref] [Google Scholar] [PubMed]
- Musso D, et al. Potential for Zika virus transmission through blood transfusion demonstrated during an outbreak in French Polynesia, November 2013 to February 2014. Eurosurveillance. Vol. 19, No. 14, 2014, pp. 20761.
[Crossref] [Google Scholar] [PubMed]
- Tamura K, et al. MEGA6: Molecular evolutionary genetics analysis version 6.0. Mol Biol Evol, Vol. 30, No. 12, 2013, pp. 2725-2729.
[Crossref] [Google Scholar] [PubMed]
- Dick GW, Kitchen SF and Haddow AJ. Zika virus (I). Isolations and serological specificity. Trans R Soc Trop Med Hyg, Vol. 46, No. 5, 1952, pp. 509-520.
[Crossref] [Google Scholar] [PubMed]
- Marchette NJ, Garcia R and Rudnick A. Isolation of Zika virus from Aedes aegypti mosquitoes in Malaysia. Am J Trop Med, Vol. 18, No. 3, 1969, pp. 24-26.
[Crossref] [Google Scholar] [PubMed]
- Weinbren MP and Williams MC. Zika virus: Further isolations in the Zika area, and some studies on the strains isolated. Trans R Soc Trop Med Hyg, Vol. 52, No. 3, 1958, pp. 263-268.
[Crossref] [Google Scholar] [PubMed]
- Olson JG and Ksiazek TG. Zika virus, a cause of fever in Central Java, Indonesia. Trans R Soc Trop Med Hyg, Vol. 75, No. 3, 1981, pp. 389-393.
[Crossref] [Google Scholar] [PubMed]
- Vanya M. Prevention of Zika virus and related complications. Rev Med Microbiol, Vol. 28, No. 2, 2017, pp. 75-78.