Research Article - International Journal of Medical Research & Health Sciences ( 2025) Volume 14, Issue 1
Evaluating Prognostic Factors and Long-Term Outcomes in Pyelonephritis: A Comprehensive Case Series Study
Pavan Kumar Yanamadala1*, Praveen Sana2, Hepzibah Rani Gidla1, Tejaswini Tirumani3 and Bhargavi Lakshmi Vadagana42Department of Nephrology, Trust Multispeciality Hospitals, Kakinada-533005, Andhra Pradesh, India
3Department of Pharmacy, Shri Vishnu College of Pharmacy, Surampalem-533437, Andhra Pradesh, India
4Department of Pharmaceutical Sciences, Andhra University, Visakhapatnam-537727, Andhra Pradesh, India
Pavan Kumar Yanamadala, Department of Pharmacy, Aditya Pharmacy College (A), Surampalem-533437, Andhra Pradesh, India, Email: pavan.yanamadala@gmail.com
Received: 11-Jul-2024, Manuscript No. IJMRHS-24-141379; Editor assigned: 15-Jul-2024, Pre QC No. IJMRHS-24-141379 (PQ); Reviewed: 31-Jul-2024, QC No. IJMRHS-24-141379; Revised: 14-Feb-2025, Manuscript No. IJMRHS-24-141379 (R); Published: 21-Feb-2025
Abstract
Introduction: Pyelonephritis is a severe bacterial infection of kidney parenchyma, often leading to kidney scarring and is potentially life-threatening.
Objective: The study was aimed at assessing the clinical profile, prognostic factors and the 6-month outcome of patients with pyelonephritis.
Materials and methods: This observational study involved qualitative and quantitative approaches to analyze various factors. The qualitative section includes those related to the antibiotics prescribed, symptoms, risk factors and other demographic details, among which the latter two were approached quantitatively.
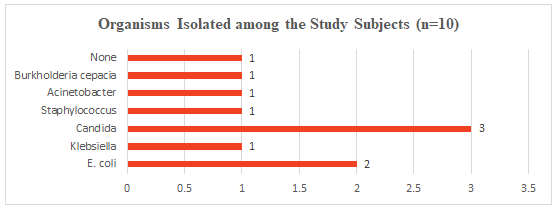
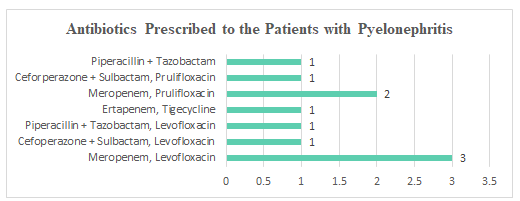
Results: Ten patients who were randomly selected were involved in the study. The mean age of the study group was 52.0 ± 8.628 years. Out of 10 subjects, 5 were males and 5 were females. Most of the subjects with Pyelonephritis suffered from symptoms like pain (90%), pyrexia (80%) and dysuria (70%). In our study, we had 20% subjects with shock, 70% with sepsis and 20% with disseminated intravascular coagulation. In all 10 out of 10 cases, type II diabetes mellitus was present. Among these cases, four showed unilateral involvement while six showed bilateral involvement. The most frequently cultured organism was Candida, accounting for 30% of cases, followed by E. coli at 20%. Eight cases underwent DJ stent and one case had percutaneous nephrostomy. One subject with advanced disease expired. Antibiotics are irreplaceable drugs in the management of pyelonephritis. All the patients were treated with IV antibiotics and 8 out of 10 subjects underwent surgical interventions.
Conclusion: It is important to consider the possibility of pyelonephritis in both male and female patients with diabetes, especially those who are unwell. Early detection and proper treatment, including medical and surgical interventions, are essential for effective management of the condition.
Keywords
Pyelonephritis, Chronic kidney disease, IV antibiotics, Uncontrolled diabetes mellitus, Unilateral and bilateral involvement, E. coli, Candida species
Introduction
Pyelonephritis is an infection-related inflammation of a kidney's parenchyma as well as the lining of its renal pelvis. In the US, there are 15-17 instances of pyelonephritis per 10,000 females and 3-4 cases per 10,000 males per year. It is a subset of urinary tract infections brought on by bacteria that move up the genitourinary system, including the kidney, from the lower to the upper regions. When bacteria, frequently originating from the fecal flora, migrate via the urethra to the bladder, causing symptomatic cystitis or silent bacteriuria, urinary tract infections ensue [1].
Acute pyelonephritis is primarily caused by gram-negative bacteria, with Escherichia coli being the most common type. Up to 80% of cases have Escherichia coli as the probable cause. Along with Pseudomonas aeruginosa, Klebsiella pneumonia, Enterococcus, Proteus mirabilis, Klebsiella oxytoca and others, gram-negative bacteria can also colonize the urinary tract. While the Viridians streptococci group, Staphylococcus saprophyticus and Streptococcus agalactiae are among the gram-positive species. The fecal flora of the majority of patients is the source of the infectious organism [2].
Although pyelonephritis is a common condition, there are still unresolved issues with the diagnostic process, the development of abscesses and the indication of hospitalization. Despite being five times more likely to be impacted than males, women die at a lower rate [3].
Women are more likely than men to get pyelonephritis and populations with diabetes are more susceptible to infection. Renal calculi, anatomical abnormalities of the urinary system and immunosuppression are the most prevalent related comorbidities in the non-diabetic population [4].
Despite the presence of poorly controlled type-II diabetes mellitus in patients, there was no significant correlation found between high tissue glucose levels and an elevated risk of mortality or the need for dialysis. This is noteworthy, as it was previously thought that such elevated glucose levels could potentially promote the growth of gas-producing bacteria in individuals with diabetes [5].
Pyelonephritis occurs when the uropathogens, primarily Escherichia coli, ascend to the kidneys from fecal flora; it is a rare complication of bacteremia that seeds the kidneys. Sexual activity frequency, genetic susceptibility, advanced age, urinary devices, diabetes, and recent urinary tract infections are risk factors. It is unclear exactly how adult pyelonephritis and vesicoureteral reflux relate to one another [6].
The general objective of the study is to study the clinical profile prognostic factors and the 6-month outcome of patients with pyelonephritis and the specific objectives of the study are to identify the group that is most susceptible to pyelonephritis, to clarify the clinical characteristics, radiological categorization and prognostic variables of Pyelonephritis and to evaluate the outcomes of the various therapy approaches (nephrectomy, percutaneous catheter drainage with DJ stent and antibiotic treatment alone) [7].
This case study series helps practice-based literature on the treatment of pyelonephritis. Additionally, it emphasizes the significance of investigating pyelonephritis as a diagnosis in patients with urinary infections who share some of the risk variables we listed in our case series [8].
Materials and Methods
Our work entails the case study examination of the clinical profile, prognostic variables and outcomes of 10 patients with pyelonephritis, even though there are many dissertations and other works linked to pyelonephritis as a whole and those relevant to kidney disease and urinary tract infections specifically. We did adhere to certain procedures in which findings of various aspects were done on a predetermined basis and the outcomes of our investigations were contrasted with those of earlier studies [9].
It is a kind of observational study in which the sample population's data variables are examined after data collection, which takes place at a set period without interfering with the subjects. The following advantages of the study were taken into consideration when choosing the study design such as all kinds of descriptive analysis can be performed with this, multiple results could be achieved simultaneously and the collection of variables simultaneously and quickly [10].
A self-structured data collecting form and certain criteria were used to select the sample. The study that was conducted comprised criteria for inclusion as well as exclusion for the conduct of the study following patient approval.
The patients from both genders who met the inclusion criteria for pyelonephritis diagnosis and management were the subjects enrolled. The persons aged below 30 years and who have crossed 80 years along with the pregnant and lactating women were excluded along with those who weren’t willing to participate in the study.
Results and Discussion
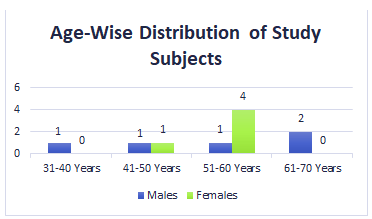
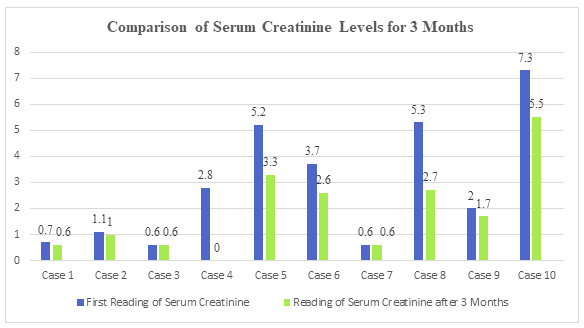
Our study's key conclusions are that serum creatinine levels greater than 5 mg/dL, shock and DIC all independently predict poor prognosis and that the disease's overall mortality rate of 10% is substantially lower than previously thought. Our study reveals that the condition primarily affected people in the age range (52.0 ± 8.628 years) and had a similar incidence in men (50% and women, respectively). Our data on gender is in contrast to other studies' findings that the disease primarily affects females. According to other records from the Indian subcontinent, the average age of ailment is significantly younger (54.4 ± 20.6 years) than it is in western data (60 years). This may be due to the Indian ethnic population's rising prevalence of diabetes mellitus, the most significant risk factor for developing pyelonephritis, which manifests at a much younger age (Tables 1-7 and Figures 1-7).
| S. no | Age group | Male (n=5) | Female (n=5) | Total (n=10) |
| 1 | 31-40 years | 1 | 0 | 1 |
| 2 | 41-50 years | 1 | 1 | 2 |
| 3 | 51-60 years | 1 | 4 | 5 |
| 4 | 61-70 years | 2 | 0 | 2 |
Table 1 Age-wise and gender-wise distribution of study subjects
Figure 1 Age-wise distribution of study subjects
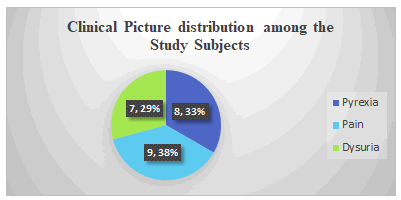
| S. no | Clinical picture | No. of subjects |
| 1 | Pyrexia | 8 |
| 2 | Pain | 9 |
| 3 | Dysuria | 7 |
Table 2 Clinical picture distribution among the study subjects
Figure 2: Clinical picture distribution among the study subjects
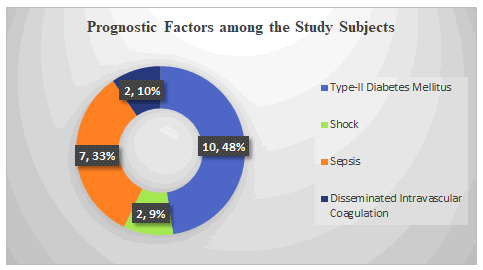
| S. no. | Prognostic factors | No. of subjects |
| 1 | Type-II diabetes mellitus | 10 |
| 2 | Shock | 2 |
| 3 | Sepsis | 7 |
| 4 | Disseminated intravascular coagulation | 2 |
Table 3: Prognostic factors in the patients with pyelonephritis
Figure 3 Prognostic factors in the patients with pyelonephritis
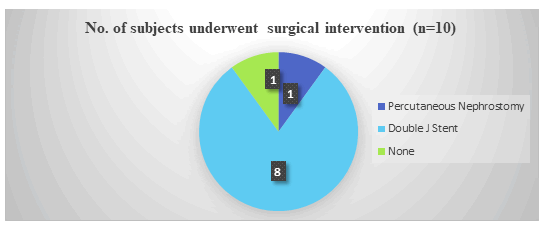
| S. no. | Surgical interventions undergone | No. of study subjects (n=10) |
| 1 | Percutaneous nephrostomy | 1 |
| 2 | Double J Stent | 8 |
| 3 | None | 1 |
Table 4 Surgical interventions underwent by the study subjects
Figure 4 Surgical interventions underwent by the study subjects
| S. no | Antibiotics prescribed | No. of patients (n=10) |
| 1 | Meropenem, Levofloxacin | 3 |
| 2 | Cefoperazone+Sulbactam, Levofloxacin | 1 |
| 3 | Piperacillin+Tazobactam, Levofloxacin | 1 |
| 4 | Ertapenem, Tigecycline | 1 |
| 5 | Meropenem, Prulifloxacin | 2 |
| 6 | Ceforperazone+Sulbactam, Prulifloxacin | 1 |
| 7 | Piperacillin+Tazobactam | 1 |
Table 5 Different antibiotics prescribed for the patients with pyelonephritis
Figure 5 Distribution of organisms isolated among the subjects
| S. no | Case details | Serum creatinine (First reading) | Serum creatinine (After 3 months) |
| 1 | Case 1 | 0.7 mg/dL | 0.6 mg/dL |
| 2 | Case 2 | 1.1 mg/dL | 1.0 mg/Dl |
| 3 | Case 3 | 0.6 mg/dL | 0.6 mg/dL |
| 4 | Case 4 | 2.8 mg/dL | 0 mg/dL |
| 5 | Case 5 | 5.2 mg/dL | 3.3 mg/dL |
| 6 | Case 6 | 3.7 mg/dL | 2.6 mg/dL |
| 7 | Case 7 | 0.6 mg/dL | 0.6 mg/dL |
| 8 | Case 8 | 5.3 mg/dL | 2.7 mg/dL |
| 9 | Case 9 | 2.0 mg/dL | 1.7 mg/Dl |
| 10 | Case 10 | 7.3 mg/dL | 5.5 mg/Dl |
Table 6 Comparison of serum creatinine levels at admission and after 3 months
Figure 6 Different antibiotics prescribed for the patients with pyelonephritis
| S. no. | Age of the study subjects | Type of pyelonephritis (Kidney involvement) | No. of days of hospital stay | Number of days of IV antibiotic therapy |
| 1 | 55 years | Right | 5 days | 5 days |
| 2 | 59 years | Right | 13 days | 13 days |
| 3 | 54 years | Bilateral | 4 days | 4 days |
| 4 | 65 years | Right | 7 days | 6 days |
| 5 | 47 years | Bilateral | 11 days | 10 days |
| 6 | 34 years | Bilateral | 5 days | 4 days |
| 7 | 50 years | Left | 6 days | 6 days |
| 8 | 65 years | Emphysematous | 5 days | 4 days |
| 9 | 58 years | Bilateral | 3 days | 3 days |
| 10 | 53 years | Bilateral | 8 days | 5 days |
Table 7 Details of the patients with the hospital stay and number of days of IV antibiotic therapy
Figure 7 Comparison of serum creatinine levels at admission and after 3 months
The patient profiles for those who were admitted with pyelonephritis are shown in the Table 8. There were five female patients with a mean age of 55.2 ± 3.563 years and five male patients with a mean age of 49.04 ± 11.366 years (Table 9).
| Age | Type-II DM | Sepsis | Shock | DIC | Pain | Pyrexia | Dysuria | Organism |
| 55F | Yes | Yes | No | No | Yes | Yes | Yes | Candida |
| 59F | Yes | No | No | Yes | Yes | Yes | No | Candida |
| 54F | Yes | No | No | Yes | Yes | Yes | No | Acinetobacter |
| 65M | Yes | No | No | No | Yes | No | Yes | Klebsiella |
| 47M | Yes | Yes | No | No | Yes | Yes | Yes | Staphylococcus |
| 34M | Yes | Yes | Yes | No | No | Yes | No | None |
| 50F | Yes | Yes | No | No | Yes | Yes | Yes | Candida |
| 65M | Yes | Yes | Yes | No | Yes | No | Yes | E. coli |
| 58F | Yes | Yes | No | No | Yes | Yes | Yes | E. coli |
| 53M | Yes | Yes | No | No | Yes | Yes | Yes | Burkholderiacepacia |
Table 8 Complete case variables of the patients with pyelonephritis (n=10)
| Age | Antibiotics prescribed | Surgical intervention | RRT | S. Cr at admission | Stay days | eGFR at admission |
| 55F | Piperacillin+Tazobactam | PCN | No | 0.7 mg/dL | 5 | 102.6 ml/min |
| 59F | Levofloxacin | None | No | 1.1 mg/dL | 13 | 54.9 ml/min |
| 54F | Meropenem Levofloxacin | DJ Stent | No | 0.6 mg/dL | 4 | 103.3 ml/min |
| 65M | Meropenem | DJ Stent | No | 2.8 mg/dL | 7 | 22.6 ml/min |
| 47M | Meropenem | DJ Stent | No | 5.2 mg/dL | 11 | 13.4 ml/min |
| 34M | Meropenem | DJ Stent | No | 3.7 mg/dL | 5 | 20.1 ml/min |
| 50F | Meropenem, Levofloxacin | DJ Stent | No | 0.6 mg/dL | 6 | 106.3 ml/min |
| 65M | Cefoperazone, Sulbactam, Prulifloxacin | DJ Stent | No | 5.3 mg/dL | 5 | 11 ml/min |
| 58F | Ertapenem, Tigecycline | DJ Stent | No | 2 mg/dL | 3 | 26.8 ml/min |
| 53M | Piperacillin+Tazobactam, Tigecycline | DJ Stent | Yes | 7.3 mg/dL | 8 | 7.7 ml/min |
Table 9 Complete case variables of the patients with pyelonephritis (n=10)
It is also interesting that, even though all 10 individuals were known to have diabetes, three had poorly regulated blood sugar levels at the time of admission. According to several earlier case series, diabetes is the underlying diagnosis in 80%-100% of cases. The other prevalent risk factor for the condition, urinary tract blockage, has been observed in 58%–60% of cases. In 50% of our cases, we found renal calculi or a co-existing blockage.
Both diabetics and non-diabetics have been known to develop pyelonephritis and the condition has been successfully treated with conservative measures. The therapy for all instances included aggressive hydration, IV antibiotics and renal support. DJ stenting was used in eight (80%) patients, while percutaneous nephrostomy was used in one case.
The most frequently reported symptoms included lower abdominal discomfort (9/10; 90%), fever (8/10; 80%) and dysuria (7/10; 70%). Huang et al. found that fever (79%) and flank pain (71%) were the most prevalent symptoms in their study of 48 EPN patients.
In their series of 21 patients, Tang et al., noted the same thing. In our research, 9 out of 10 (90%) patients reported experiencing loin pain or tenderness. Although there have been a variety of symptoms recorded, soreness in the loin area is usually reported.
E. coli was shown to be the cause of 65.6% of EPN cases in a thorough assessment of published data, followed by Klebsiella in 19.5% of cases and mixed organisms in 10%. Our findings show the opposite. E. coli 2/10 (20%), Klebsiella 1/10 (10%), Candida 3/10 (30%), Staphylococcus 1/10 (10%), Acinetobacter 1/10 (10%) and Burkholderiacepacia 1/10(10%) were all present in two instances each. Acinetobacter was isolated from one patient who had renal/ureteric calculi, whereas E. coli and Burkholderia were isolated from another patient.
The eGFRs of patients upon admission to our study encompassed all stages of CKD from I to V, with none of the patients necessitating renal replacement therapy.
In contrast to other reports, our series' overall mortality rate was substantially lower at 10%. Since percutaneous drainage/DJ stenting has become widely used, there has been a decline in mortality during the past ten years.
Early control of bacteremia is more probable when potent medications targeting extended-spectrum beta-lactamaseproducing pathogens are accessible. A majority of our patients received treatment with fourth-generation cephalosporins and carbapenems, both of which are classes of extended-spectrum antibiotics known for their high efficacy against coliforms. We believe that early identification of the disease is crucial for its effective treatment.
Seven out of ten (70%) of our cases had sepsis. Sepsis has never been studied or characterized as an independent prognostic factor in any of the previously published big series. Three of our cases (30%) had thrombocytopenia. It has also been noted that having thrombocytopenia at admission of less than 1, 20, 000 cells/cu.mm is a separate prognostic indicator in the past. In 2/10 (20%) of the instances, shock was evident. 40 percent of cases (4 out of 10) had hypotension. Once more, serum creatinine (>5.0 mg/dL) was linked to death. Our findings are consistent with those of other studies in which serum creatinine was identified as a distinct predictive factor.
In two of the ten instances in which DJ stenting was performed, DIC was a standalone risk with a bad prognosis. Our study was further limited by the fact that it was a retrospective analysis and that there weren't enough cases to properly examine the other risk factors. Additionally, statistical discrepancies in relation to the other risk factors may have been explained by this. We are aware that a 6-month follow-up period is not very long, but we believe that it still provides us with a general idea of how the disease is progressing.
Conclusion
Men and women who have diabetes are more likely to be affected by pyelonephritis, but this is not always the case. While coliforms are the most common bacteria causing the illness, EPN can also be caused by rare bacteria. For a mild form of the condition, early and aggressive hydration, along with the appropriate IV extended-spectrum antibiotics, is the preferred treatment. In advanced stages, percutaneous drainage (and if necessary, nephrectomy) should be performed.
With the latest dialysis technologies, it is important to initiate kidney support early. All diabetic individuals with kidney complications should be suspected and evaluated for the disease. The significance of early disease detection and proper treatment with a combination of medical and surgical therapy cannot be emphasized enough. Furthermore, larger prospective trials are needed.
Data Availability
The data supporting this research is accessible from the corresponding author upon a reasonable request.
Conflicts of Interest
The authors have disclosed that there are no conflicts of interest associated with the present manuscript
Author’s Contributions
Dr. Pavan Kumar Yanamadala and Dr. Praveen Sana designed the study. Dr. Tejaswini Tirumani performed the data analysis and drafted the Manuscript along with Dr. Pavan Kumar Yanamadala. Dr. Pavan Kumar Yanamadala collected the data. All authors have read and approved the final manuscript.
Funding
The present study has received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical Considerations
The authors have conscientiously ensured that ethical matters, including plagiarism, data falsification and redundant publication, have been thoroughly considered and addressed.
References
- Nicolle LE. Uncomplicated urinary tract infection in adults including uncomplicated pyelonephritis. Urological Clinics of North America. Vol. 35, No. 1, 2008, pp. 1-2.
[Crossref] [Google Scholar] [PubMed]
- Gupta K, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical Infectious Disease. Vol. 52, No. 5, 2011, pp. e103-e120
[Crossref]
- Mohsin N, et al. Emphysematous pyelonephritis: A case report series of four patients with review of literature. Renal Failure. Vol. 31, No. 7, 2009, pp. 597-601.
[Crossref] [Google Scholar] [PubMed]
- Arsene C, et al. A case series of emphysematous pyelonephritis. Case Reports in Medicine. Vol. 2014, No. 1, 2014, pp. 587926.
[Crossref] [Google Scholar] [PubMed]
- Huang JJ and Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Archives of Internal Medicine. Vol. 160, No. 6, 2000, pp. 797-805.
[Crossref] [Google Scholar] [PubMed]
- Alâ?Geizawi SM, et al. Renal allograft failure due to emphysematous pyelonephritis: successful nonâ?operative management and proposed new classification scheme based on literature review. Transplant Infectious Disease. Vol. 12, No. 6, 2010, pp. 543-550.
[Crossref] [Google Scholar] [PubMed]
- Fatima R, et al. Emphysematous pyelonephritis: A single center study. Indian Journal of Nephrology.Vol. 23, No. 2, 2013, pp. 119-124.
[Crossref] [Google Scholar] [PubMed]
- Huang JJ and Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Archives of Internal Medicine.Vol. 160, No. 6, 2000, pp. 797-805.
[Crossref] [Google Scholar] [PubMed]
- Tang HJ, et al. Clinical characteristics of emphysematous pyelonephritis. Journal of Microbiology, Immunology, and Infection.Vol. 34, No. 2, 2001, pp. 125-130.
[Google Scholar] [PubMed]
- Khaira A, et al. Retrospective analysis of clinical profile prognostic factors and outcomes of 19 patients of emphysematous pyelonephritis. International Urology and Nephrology.Vol. 41, 2009, pp. 959-966.
[Crossref] [Google Scholar] [PubMed]