Research Article - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 5
Extra Corporeal Membrane Oxygenation (ECMO)
Anjalatchi Muthukumaran*Anjalatchi Muthukumaran, Department of Health Science, Era College of Nurshing, Era University, Lucknow, Uttar Pradesh, India, Email: anjalatchidm@gmail.com
Received: 07-Dec-2022, Manuscript No. IJMRHS-22-82644; Editor assigned: 09-Dec-2022, Pre QC No. IJMRHS-22-82644 (PQ); Reviewed: 23-Dec-2022, QC No. IJMRHS-22-82644; Revised: 16-Mar-2023, Manuscript No. IJMRHS-22-82644 (R); Published: 23-Mar-2023
Abstract
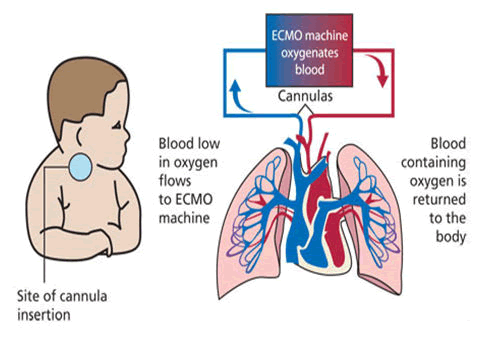
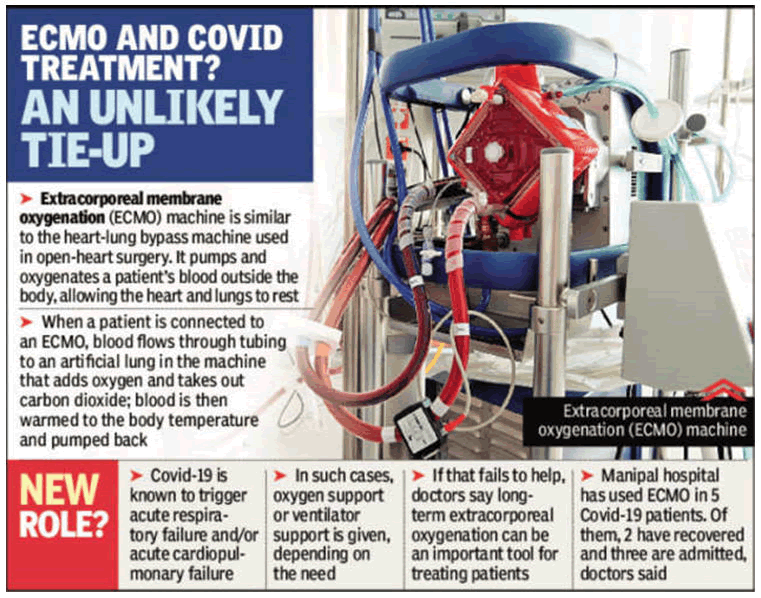
ECMO is a machine support with artificial work of human being when heart not able to function properly as temporary base. The ECMO machine is similar to the heart-lung bypass machine used in open heart surgery. It pumps and oxygenates a patient’s blood outside the body, allowing the heart and lungs to rest. ECMO may be used to help people who are very ill with conditions of the heart and lungs or who are waiting for or recovering from a heart transplant. It may be an option when other life support measures haven’t worked. ECMO does not treat or cure a disease, but can help you when your body temporarily can’t provide your tissues with enough oxygen.
Risks: The most common risks that may occur with ECMO include: Bleeding, blood clot (thromboembolism), blood clotting disorder (coagulopathy), infection, loss of blood in hands, feet or legs (limb ischemia), seizures, stroke (part of the brain is damaged by loss of blood or by a blood vessel that bursts).
Results: The outcomes associated with ECMO depend upon the severity of the health condition that led to useof ECMO. Your doctor can explain how helpful ECMO may be in your situation.
Expectation: It will insert a thin, flexible tube (cannula) into a vein to draw out blood and a second tube into a vein or artery to return warmed blood with oxygen to your body. You will receive other medications, including sedation to make you comfortable while receiving ECMO and may not be able to talk during this time
https://sporbahisleri.livejournal.com https://wakelet.com/@SporBahisleri67459 https://theomnibuzz.com/author/sporbahisleri/ https://lessons.drawspace.com/profile/322207/sporbahisleri/workflow https://writeupcafe.com/profile/sporbahisleri/ http://www.pearltrees.com/sporbahisleri https://pharmahub.org/members/26874/blog https://www.zupyak.com/u/Spor-Bahisleri/ https://www.metroflog.co/sporbahisleri https://www.fuzia.com/fz/spor-bahisleri https://tr.pinterest.com/sporbahislerim/ https://my.getjealous.com/sporbahisleri https://sporbahisleri.contently.com https://hubpages.com/@sporbahisleri https://www.tumblr.com/sporbahisleri https://hub.docker.com/u/sporbahislerim https://betsiteleri.blogfree.net https://betsiteleri.amebaownd.com https://sporbahisleri.pixnet.net/blog https://betsiteleri.seesaa.net https://betsiteleri.threadless.com https://betsiteleri.neocities.org https://bahissiteleri.localinfo.jp https://betsiteleri.shopinfo.jp https://teletype.in/@betsiteleri https://ubl.xml.org/users/sporbahisleri https://betsiteleri.educatorpages.com https://betsiteleri.onlc.fr https://sporbahisleri.gumroad.com
Keywords
ECMO, Blood clot, Seizures, Sedation, Coagulopathy
Introduction
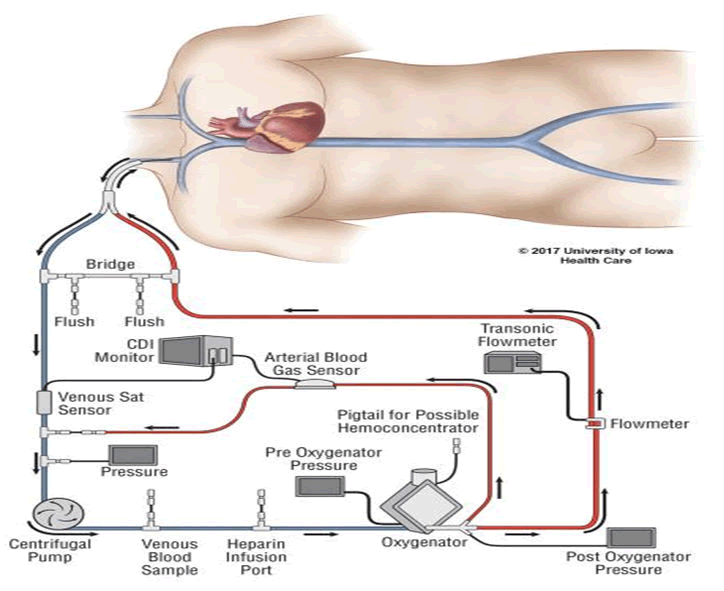
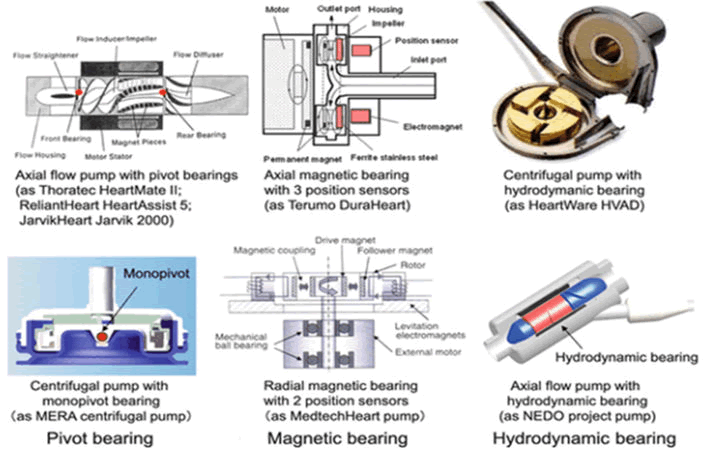
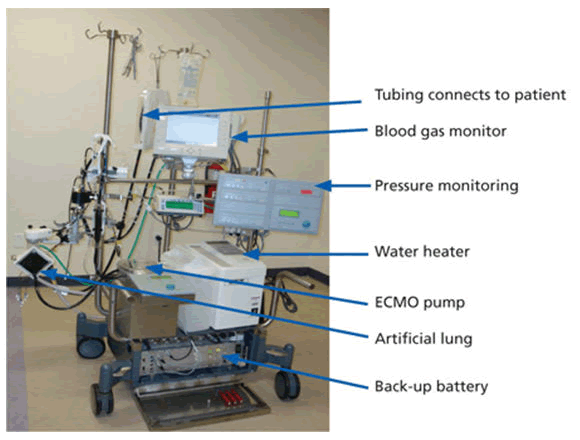
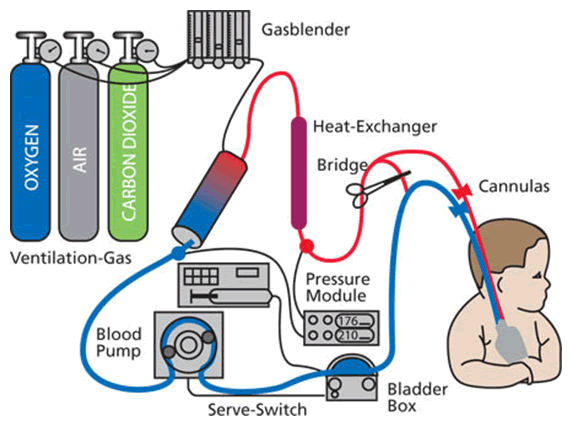
ECMO stands for Extracorporeal Membrane Oxygenation. The ECMO machine is similar to the heart-lung bypass machine used in open heart surgery. It pumps and oxygenates a patient’s blood outside the body, allowing the heart and lungs to rest [1]. When you are connected to an ECMO, blood flows through tubing to an artificial lung in the machine that adds oxygen and takes out carbon dioxide; then the blood is warmed to body temperature and pumped back into your body. The ECMO machine replaces the function of the heart and lungs. People who need support from an ECMO machine are cared for in a hospital’s Intensive Care Unit (ICU). Typically, people are supported by an ECMO machine for only a few hours to days, but may require it for a few weeks, depending on how their condition progresses [2-4]. There are many overlaps and differences between the use of ECMO in children and adults. For a focus on pediatric ECMO, please refer to the Medline plus resource listed at the end, in addition to this fact sheet (Figure 1).
Materials and Methods
What is ECMO?
Extracorporeal Membrane Oxygenation (ECMO) is a life support machine. People who need ECMO have a severe and life threatening illness that stops their heart or lungs from working properly. For example, ECMO is used during life threatening conditions such as severe lung damage from infection or shock after a massive heart attack [5].
Why is ECMO used?
ECMO is used to help people whose:
• Lungs cannot provide enough oxygen to the body even when given extra oxygen.
• Lungs cannot get rid of carbon dioxide even with help from a mechanical ventilator.
• Heart cannot pump enough blood to the body ECMO may also be used to support people with heart or lung disease that cannot be cured while they wait for an organ transplant (e.g. new heart and/or lungs).
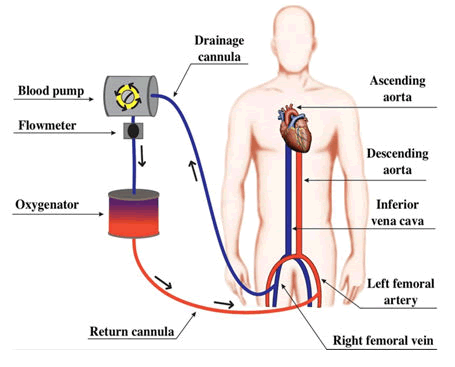
How does an ECMO machine work?
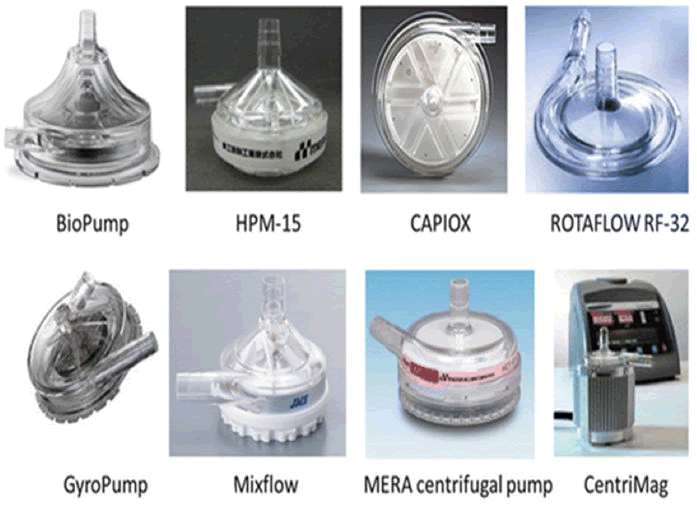
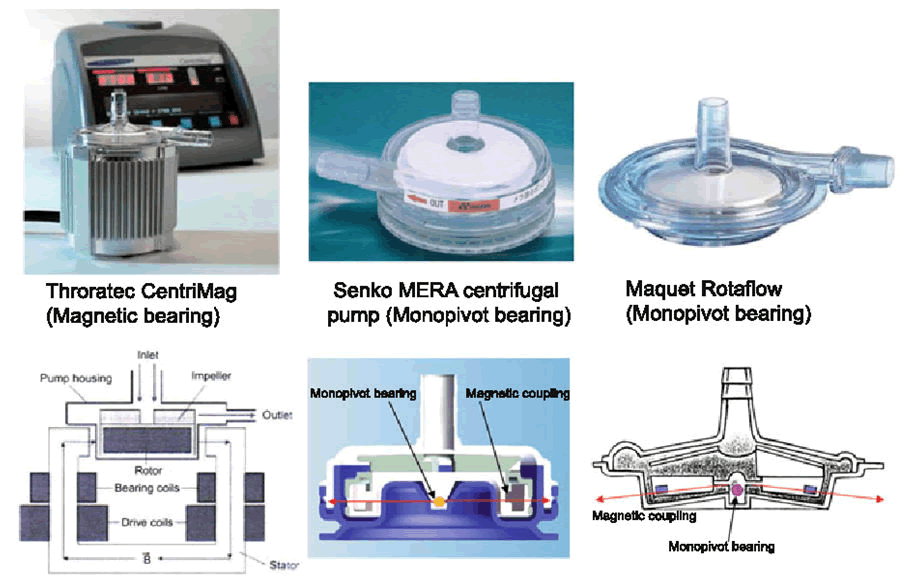
The ECMO machine is connected to a patient through plastic tubes (cannula). The tubes are placed in large veins and arteries in the legs, neck or chest. The procedure by which a healthcare provider places these tubes in a patient is called cannulation. The ECMO machine pumps blood from the patient’s body to an artificial lung (oxygenator) that adds oxygen to it and removes carbon dioxide. Thus, it replaces the function of the person’s own lungs. The ECMO machine then sends the blood back to the patient via a pump with the same force as the heart, replacing its function. The ECMO machine is controlled by a person called a perfusionist or a nurse or respiratory therapist with advanced training called an ECMO specialist [6]. The perfussionist or ECMO specialist will adjust the settings on the machine to give the patient the amount of heart and lung support they need.
How is a patient on an ECMO machine monitored?
Anyone who is connected to an ECMO machine in the ICU is also connected to monitors. These monitors measure heart rate, blood pressure and oxygen levels. Patients on ECMO need their blood tested very often to measure the oxygen and carbon dioxide levels. These tests are called blood gases. Patients on ECMO are also given a medication to thin the blood so it does not clot. Thus, the blood is tested frequently to make sure it is thin enough. All of these results are used to see how well the ECMO machine is helping the patient and to make changes if needed (Figures 2-6).
How long is an ECMO machine used?
An ECMO machine can help save a person’s life, but it does not treat the disease or injury that led to the heart and lung failure. An ECMO machine simply provides support for a person while the healthcare team works on treating the underlying disease or injury (such as an infection) or until organs for transplant become available. Healthcare providers will always try to help people get off the ECMO machine as soon as possible. Some diseases or injuries can be treated quickly and patients only need the ECMO machine for a few hours. Other conditions may take longer to get better, in which case the patient may need the ECMO machine for several days to weeks. Unfortunately, some people do not improve enough to be taken off the ECMO machine. ECMO does not save everyone but it has improved survival for many critically ill people who are not responding to usual life support options.
How does it feel to be on ECMO?
When a person is first being connected to an ECMO machine, he or she is sedated and does not feel the tubes going into their veins and arteries. A person on ECMO is usually already connected to a breathing machine (ventilator) through a tube (Endotracheal or ET tube) that is placed in the mouth or nose and down into the windpipe (For more information, see mechanical ventilation). Once connected to an ECMO machine, the cannulae are not painful. People who are on an ECMO machine may be given medicines (sedatives or pain controllers) to keep them comfortable. These medicines may also make them sleepy. Some people are awake and can talk and interact with people while on an ECMO machine. In some cases, patients can exercise to help build up their strength while they are on an ECMO machine. However, some movements can cause the ECMO tubes to get kinked, so patients need to be assisted and carefully supervised when they are moving.
Types of ECMO machine
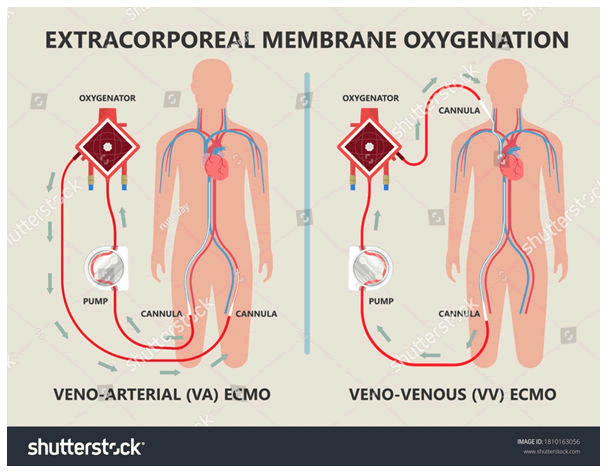
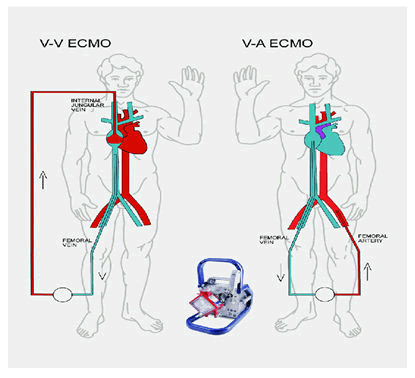
There are two types of ECMO:
• The VA ECMO is connected to both a vein and an artery and is used when there are problems with both the heart and lungs.
• The VV ECMO is connected to one or more veins, usually near the heart and is used when the problem is only in the lungs.
USCF is also now using a smaller portable ECMO device that is light enough to be carried by one person and can be transported in an ambulance or helicopter, making it possible to provide ECMO relief in emergency cases (Figures 7 and 8).
When is ECMO used
• For patients recovering from heart failure or lung failure or heart surgery.
• As a bridge option to further treatment, when doctors want to assess the state of other organs such as the kidneys or brain before performing heart or lung surgery.
• For support during high risk procedures in the cardiac catheterization lab.
• As a bridge to a heart assist device, such as Left Ventricular Assist Device (LVAD).
• As a bridge for patients awaiting lung transplant. The ECMO helps keep tissues well oxygenated, which makes the patient a better candidate for transplant.
How does ECMO work?
Special tubes called cannula are put into the blood vessels that go directly into your child’s heart or bloodstream. Your child’s doctor chooses the size of the tubes based on his or her size, age, weight and the reason why ECMO is being used. The cannula transfer the blood from the child’s heart by using a pump to push the blood through tubes to the machine where the blood receives oxygen and the carbon dioxide is removed. Next the blood is warmed to body temperature. Finally, the warm blood goes through another cannula back your child’s body.
Look at the following pictures of the ECMO circuit/machine. They are labeled to help you understand how the blood flows from the child through the cannula, into the machine and back to the child (Figure 9).
What are the modes of ECMO support?
Veno-Venous (VV): This type of ECMO provides support for the lungs only. One or two cannulas are placed in large vein(s) on the side of the neck or in the groin area at the top of the leg. Your child’s heart will continue to work normally. The ECMO machine will drain the blood from the vein through the cannula, oxygen will be added to the blood, carbon dioxide will be removed and then the blood is warmed and returned back to the right side of the heart through the cannula. The child’s heart pumps the oxygenated blood to the body, so that the lungs have time to rest and recover.
Veno-Arterial (VA): VA ECMO provides support for both the lungs and the heart. Two cannulas are placed in large vessels on the side of the neck, directly into the chest (while the chest is covered with a sterile protector) or into the groin vessels. The ECMO machine will drain the blood from the vein, add the oxygen and remove the carbon dioxide, warm the blood and then return the blood to the artery and “pump” the blood through the body (Figure 10). This method allows the blood to “bypass” the heart and lungs, allowing them to rest and get better.
Procedure
Being placed on ECMO requires a surgical procedure but it is usually done in a patient’s room. The patient is sedated and given pain medication and an anti-coagulant to minimize blood clotting. A surgeon, assisted by an operating room team, inserts the ECMO catheters into either an artery or veins. An X-ray is then taken to ensure the tubes are in the right place. Usually a patient on the ECMO pump will also be on a ventilator, which helps the lungs to heal. While on ECMO, the patient will be monitored by specially trained nurses and respiratory therapists, as well as the surgeon and surgical team. Since you will be sedated and have a breathing tube in place, supplemental nutrition will be provided either intravenously or through a nasal gastric tube. Nutrition is delivered either intravenously or through a nasal gastric tube while on ECMO, you may be given certain medications including: Heparin to prevent blood clots; antibiotics to prevent infections; sedatives to minimize movement and improve sleep; diuretics to help the kidney get rid of fluids; electrolytes to maintain the proper balance of salts and sugars and blood products to replace blood loss. Discontinuing ECMO requires a surgical procedure to remove the tubes. Multiple tests are usually done prior to the discontinuation of ECMO therapy to confirm that your heart and lungs are ready. Once the ECMO cannulas are removed, the vessels will need to be repaired. This can be done either at the bedside or in the operating room. The doctor will use small stitches to close the spot where the tubes were placed. You will be asleep and monitored for this process. Even though you are off the ECMO, you may still need to be on a ventilator.
What are the risks of being on ECMO?
The healthcare team always aim to avoid any complications that may occur from being on ECMO. Some of the more serious problems that may occur when a patient is on ECMO include:
Bleeding: Because of the blood thinning medication that patients need while on ECMO, they can start bleeding in different parts of their body. This can be a very serious problem if the bleeding happens in their brain, lungs, insertion sites of cannulae or from their stomach. The healthcare team monitors patients very carefully by frequent physical exams and lab tests to make sure there is no bleeding. If there is bleeding, then medications can be given to help the blood to clot. Sometimes, surgery is needed to stop the bleeding. Blood and other blood products (such as platelets) may also need to be given if blood counts drop too low.
Kidney failure: Patients who are on ECMO sometimes do not get enough blood flow to their kidneys. This can cause their kidneys to stop working, known as “acute renal failure”. If the kidneys stop working, then a patient may need to be connected to a machine that does the work of the kidneys. This is called dialysis. The kidney damage may get better. However, in some cases, patients may need dialysis for the rest of their life.
Infection: The tubes from the ECMO machine go from outside the patient’s body directly into their bloodstream. This increases the risk for infection, because the tubes are a way for germs to enter the body. The infection can reach the lungs or any other part of the body. Infections in patients on ECMO can usually be treated with antibiotics. However, some patients who develop infections while on ECMO can get sicker and suffer organ damage.
Leg damage: Some patients are connected to the ECMO machine through a vein or artery in the groin (top of the leg). In some cases, this can impair the blood flow down that leg and the tissue in the leg can die. If this happens, doctors will try to get blood flowing back down the leg. This usually means changing the ECMO tubing to another part of the body. Rarely, the damage is so bad that the person needs surgery to correct the problem, which may include amputation (removal of part of the leg).
Stroke: In patients on ECMO, certain areas of the brain may not get as much blood flow as they need because of small blood clots. This can cause a stroke, and parts of the brain may be permanently damaged. The area of the brain that is damaged will determine what problems a person has from a stroke. A stroke may limit one’s ability to move certain parts of their body, see, remember, speak, read or write. Sometimes a person will recover some function after a stroke, but that is not always the case. Fortunately, strokes are very rare and happen less than 5% of the time to people on ECMO.
Results and Discussion
How does a person get taken off ECMO?
The ECMO machine supports the person while he or she tries to overcome a disease or injury. If the disease or injury improves, the patient may not need the support of the ECMO machine anymore. The healthcare providers will slowly reduce the amount of support the ECMO machine is providing to see if the patient will be okay without it, just like they do with a ventilator (see ATS patient education fact sheet on mechanical ventilation). If the person remains stable or improves as this is being done, the ECMO tubes are removed and surgeons stitch the entry spots up to close them (Figure 11).
What happens if a person cannot be taken off ECMO?
ECMO is only a “life sustaining treatment.” It does not cure or treat the disease or injury that led to heart and/or lung failure. This means it is a treatment that can prolong life to allow for more time to try to fix the problem. Sometimes patients do not get better while they are on ECMO because their disease or injury cannot be fixed. A decision about whether there is benefit to continuing ECMO can be hard and some people will not want to stay on ECMO if they are not improving. If the healthcare providers believe that the patient’s disease or illness is very severe and will not get better, they will discuss this carefully with the person and family members and help to make decisions about the end of life and removing the person from ECMO support. If the patient cannot talk or communicate his or her decision, the healthcare providers will talk with the patient’s legally authorized representative (usually a spouse, parent or next of kin). While patients can die even though they are connected to ECMO, sometimes ECMO seems to prolong the dying process. It is important to talk to your family members and your healthcare providers about your wishes regarding end of life and what you would like to happen in different situations. The more you clearly explain your values and choices to your loved ones and healthcare providers, the easier they will be able to follow your wishes if and when you are unable to make decisions for yourself. An advanced directive (or a “living will”) is a way to put your wishes in writing to share with others. In the hospital, nurses, doctors and social workers can provide information about how to complete an advanced directive form (Figures 12 and 13).
ECMO does carry risks including
• Bleeding, due to the medication that’s given to prevent blood from clotting in the tubing.
• Infection at the sites where the tubes enter the body.
• Transfusion problems, since a person on ECMO is given blood products.
• Small clots or air bubbles forming in the tubing.
• Increased chance of stroke.
Care of patients with ECMO
The patient requiring Extracorporeal Membrane Oxygenation (ECMO) for any etiology is almost always managed in the Intensive Care Unit (ICU) and requires care around the clock, which is delivered by a collaboration of physicians, nurses (RNs), respiratory therapists, perfusionists and many others. Close collaboration between care providers is crucial, particularly between the RN managing hemodynamic medication infusions and the ECMO specialist managing the pump.
• Nursing implications for cannula site management.
• Skin integrity implications in ECMO patients.
• Early mobility in ECMO.
• Nursing implications for detection and prevention of systemic complications related to ECMO.
• Renal and other intraabdominal complications.
• H infectious complications.
• Cardiopulmonary complications.
• Hematological complications.
• Neurological complications.
• Nursing implications in ethics and ECMO withdrawal.
Conclusion
The ECMO patient is often the most critically ill within the hospital at any given moment, prompting highly trained bedside RNs as well as other healthcare providers, familiar with the therapy, to be readily available to provide the multifaceted care this population requires. In addition to routine ICU care, the ECMO patient necessitates additional monitoring due to associated risk factors assumed when being placed on pump. Medical, ethical and emotional considerations exist and must be addressed regularly in order to provide the best care of this unique patient population.
References
- Clements L, et al. Reducing skin breakdown in patients receiving extracorporeal membranous oxygenation. Nursing Clinics of North America, Vol. 49, No. 1, 2014, pp. 61-68.
[Crossref] [Google Scholar] PubMed]
- Combes A, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. The New England Journal of Medicine, Vol. 378, No. 21, 2018, pp. 1965-1975.
[Crossref] [Google Scholar] [PubMed]
- Daly K, et al. An international survey: The role of specialist nurses in adult respiratory extracorporeal membrane oxygenation. Nursing in Critical Care, Vol. 22, No. 5, 2017, pp. 305-311.
[Crossref] [Google Scholar] [PubMed]
- Driscoll A, et al. The effect of nurse to patient ratios on nurse sensitive patient outcomes in acute specialist units: A systematic review and meta-analysis. European Journal of Cardiovascular Nursing, Vol. 17, No. 1, 2018, pp. 6-22.
[Crossref] [Google Scholar] [PubMed]
- Esper SA, et al. Extracorporeal membrane oxygenation in the adult: A review of anticoagulation monitoring and transfusion. Anesthesia and Analgesia, Vol. 118, No. 4, 2014, pp. 731-743.
[Crossref] [Google Scholar] [PubMed]
- Hamdi T and Palmer BF. Review of extracorporeal membrane oxygenation and dialysis based liver support devices for the use of nephrologists. American Journal of Nephrology, Vol. 46, No. 2, 2017, pp. 139-149.
[Crossref] [Google Scholar] [PubMed]