Research Article - International Journal of Medical Research & Health Sciences ( 2023) Volume 12, Issue 5
Need Assessment of the Patients and Caregivers Living with Atopic Dermatitis in India-A Qualitative Research Study
Ratna Devi, Tamanna Sachdeva and Rajat Jain*Rajat Jain, Department of Health and Education, Dakshayani and Amaravati Health and Education, Dwarka, New Delhi, India, Email: rajat.jain@dakshamahealth.org
Received: 27-Dec-2022, Manuscript No. IJMRHS-22-84820; Editor assigned: 29-Dec-2022, Pre QC No. IJMRHS-22-84820 (PQ); Reviewed: 12-Jan-2023, QC No. IJMRHS-22-84820; Revised: 20-Mar-2023, Manuscript No. IJMRHS-22-84820 (R); Published: 27-Mar-2023
Abstract
Background: Atopic Dermatitis (AD) is one of the most common types of eczema. In India, there is a scarcity of literature on the disease burden and challenges associated with the diagnosis and treatment of AD of patients and caregivers. Dakshama health (Dakshayani and Amaravati health and education) conducted a qualitative research study of patients suffering from AD to understand the unmet needs and challenges in India.
Methodology: A qualitative study was conducted on 24 AD patients. A structured questionnaire was used to collect the patients perspectives. In-depth interviews were carried out of the patients and caregivers living with AD. Patients’ challenges and unmet needs were transcribed and content analysis was carried out.
Results: Patients expressed a need for reliable information about AD. Due to lack of credible information, they develop misconceptions and experienced stigma and discrimination, leaving them depressed. Patients end up visiting multiple doctors before receiving a confirmed diagnosis of AD, which worsens their condition. Patients seek alternative treatments and discontinue medications, leading to complications. Embarrassment caused by visible symptoms has resulted in societal rejection, anxiety, depression and suicidal behavior.
Conclusion: AD is accompanied by a lifelong therapy that eventually drains one’s finances. High treatment cost makes it difficult for them to continue with the treatment, leaving them frustrated. Their perspectives must be acknowledged and brought to the policy table to develop standard treatment and management guidelines. AD recognition under national health policy can open the door for more affordable and accessible treatment for patients
Keywords
Atopic dermatitis, Patients, Dermatologist, Challenges, Quality of life
Introduction
Atopic Dermatitis (also known as AD) is the one of the most common types of eczema. Atopic dermatitis affects an estimated 2.5% of the world’s population. According to the International Study of Asthma and Allergies in Childhood (ISAAC), the prevalence of AD in India is 2.7% for children aged six to seven years and 3.6% for children aged thirteen to fourteen years. A few hospitals based and region specific studies have been conducted to determine the prevalence of AD in India [1]. The data may differ due to changing weather conditions. It typically manifests as a red, itchy rash on the cheeks, arms and legs. Atopic dermatitis usually begins in childhood, usually within the first six months of a baby’s life. It is a common type of eczema that can be severe and long lasting.
Atopic dermatitis tends to disappear as a child grows older, though some children will have flare-ups during their adulthood. Asthma and hay fever are two other allergic conditions that coexist (allergic rhinitis) [2].
The exact cause of atopic dermatitis is unknown. According to current evidence, AD is caused by a combination of genetics and environmental factors. Atopic dermatitis patients have a mutation in the gene that produces filaggrin. With the help of the protein filaggrin, our bodies maintain a healthy, protective barrier on the very top layer of skin. If there is insufficient filaggrin to create a sturdy skin barrier, moisture can escape and bacteria, viruses, and other organisms can enter.
Research objectives
The scope of this study is to determine the following objectives:
• To determine unmet needs of people living with AD and the impact of the disease on their quality of life.
• To understand the unmet needs and challenges of AD patients in India.
Materials and Methods
A qualitative study was conducted in respect to understand the unmet needs of AD patients in India. Virtual in-depth interviews and mini focus groups discussion were chosen as a method to secure the essences of this study. A detailed and structured questionnaire was used as a tool under this method to capture the answers given by the interviewees [3]. The answers were transcribed and content analysis was conducted to get a better picture of the major problems being faced by the patients. Ethical considerations and informed consent for patients and caregivers were considered (Table 1).
| Bifurcation of sample and methods | ||
| In person in-depth interview | Virtual in-depth interview | Focus group discussions |
|---|---|---|
| Twenty four AD patients (twenty one moderate and three severe cases). | Ten virtual in-depth interviews (eight patients, two caregivers), one virtual paired in-depth interview. | Three virtual mini focused group discussions (two female and one male group) with four patients (twelve) each was conducted. |
| Seventeen adults more than or equal to eighteen years of age and seven caregivers for patients equal to or less than sixteen years of age. | ||
Parameters
Interviewed patients were analysed on the following parameters (Table 2).
| Awareness | The level of atopic dermatitis awareness among patients and caregivers. |
| Patient journey | The patient’s journey from the onset of symptoms to life long management. |
| Diagnosis | Challenges in diagnosing the disease. |
| Treatment | The challenges encountered in treating and managing the disease. |
| Impact on quality of life | AD’s impact on patient’s life in terms of social, mental and productivity. |
Results and Discussion
Awareness
Patient’s lack of awareness about atopic dermatitis causes a delay in diagnosis and identifying the relevant specialist at the right time. In the first instance, they did not see a dermatologist; instead, they preferred family doctors. The initial symptoms are sometimes identified as vernacular terminologies such as ‘Dadar’ in Gujrathi and Kharish in Hindi/Punjabi, allergy or a fungal infection [4].
I don’t know anything about this condition; I don’t know the name so cannot find anything. I don’t talk to anyone about the skin problem I have (patient atopic dermatitis).
They have no idea what causes the disease and associate it with various skin conditions. They end up searching online or relying on close family members for their management.
I saw on YouTube and went to Safdarjung hospital and AIIMS, showed myself to a skin specialist. All the doctors were saying that the redness and allergy was there and it will be fine if you apply medicines on it. On YouTube I searched all the reasons for infants getting an itch. It showed home remedies for it like use oil or Multani Miti paste (bentonite clay paste) (caregiver atopic dermatitis).
They end up seeing multiple doctors, which irritates them because of the disease not being cured. Absence of authentic information also leads to misconceptions and they opt for non-clinically defined treatments or remedies, which sometimes make their condition worse. Patients would rather use home remedies such as oil and camphor, soframycin, other skin creams, dettol (antiseptic liquid) to clean the skin, talcum powder and so on. They become frustrated by their own condition and avoid social gatherings due to the embarrassment and stigma resulting from lack of awareness.
In our family we never faced such issue. Name was something different and we knew it as infection or allergy. I used Johnson and Johnson baby soap, but I felt the soap did not suit my condition. I googled about it as others had no knowledge about it. I just took care of my skin and applied the medicines. It is long term problem and there is no remedy for it. It is not permanent solution as to what to do. One gets lot of irritation due to this (patient atopic dermatitis) [5].
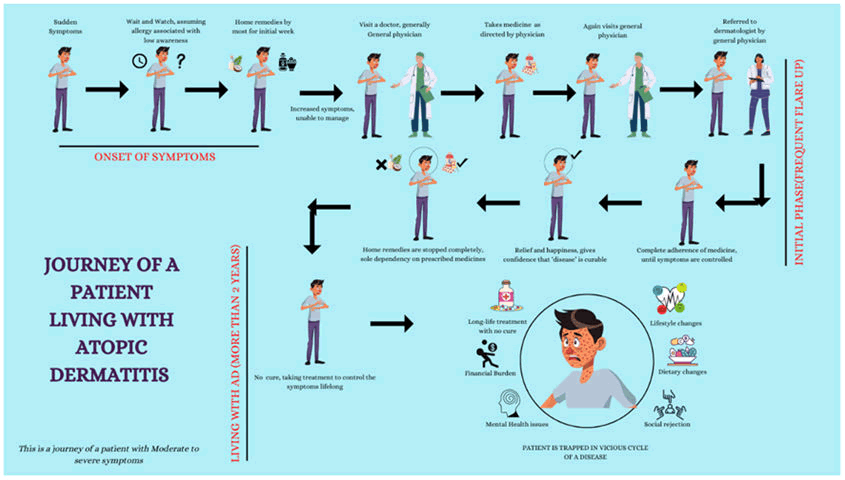
Patient journey
Onset of the symptoms: Sudden onset of symptoms comes with itching, dryness and redness. Patients overlook their symptoms because they believe they are caused by an allergic reaction or a weather change. Compared to moderate and severe atopic dermatitis, patients with mild atopic dermatitis have less itching. As a result, they frequently choose home remedies to help them manage their symptoms. Mild to moderate patients were also observed investigating the problem online and using home cures till the effects of the condition got worse. Patient journey is similar for the patients with moderate and severe symptoms.
My daughter had rashes for the first time when she was a year old. Honestly, I wasn’t much concerned about it as I thought it will go in some time and will not worsen in future. Symptoms were very mild and mostly in the joints. I never discussed it with my family as I never felt it was a big problem. I just changed normal milk to soya milk (severe patient caregiver atopic dermatitis).
Initial phase (frequent flare ups): Patients with moderate to severe itching visits a doctor as soon as the itch or management gets out of hand. In most cases, a family physician was chosen as the initial point of contact. While some of them continued to receive care from their family physicians as their diseases worsened, some were referred to a dermatologist. Up until the symptoms disappeared, there was complete adherence to the prescription. When the symptoms vanished, some patients began to discontinue taking their medications [6]. They gain confidence that the “illness’’ is treatable because of the relief and satisfaction when the discomfort and itching were subsided. Home remedies were completely discontinued and only dependence on prescribed medications was observed.
“When she was about 6.5 years old then her skin started deteriorating. We travelled to Rajasthan and the dry weather made it even worse. That was major flare up she had. It was not only on joints, but rashes were all over the body” (severe patient caregiver atopic dermatitis).
Living with AD (more than 2 years): Patients with mild symptoms get relief both at the symptomatic and emotional level. Patients with moderate symptoms adapt lifestyle changes (using gloves while doing any work, avoiding skin contact with detergents, washing clothes separately) etc. Associated stress, anxiety, embarrassment continued for patients and caregivers suffering with severe symptoms [7].
Like all the creams that are available in the market, we had applied on her and we had done wet trapping and UV therapy and all the therapies we could. None of it could control the deterioration and all the steroids we did till 2012 June when her skin became all raw all over. Her face was only partly okay. Finally, the doctor said to give oral steroids or there could be the need to hospitalize, else she will catch infection. We started her on oral steroids at that time. That was the only thing we could do and then she was on medication for the next 5 years, so that’s how medication started one after the other. She switched to other medicines after a month because you cannot be on steroids for a very long time. Cyclosporin was the first one and then methotrexate, so these two we started and it was mostly cyclosporin at that time so yes that’s how it started. We took her to UK and showed her to the top allergy specialist and dermatologist and he recommended another immunosuppressant. It is a chronic condition, it affects you every day, it’s not something that happens occasionally. Every single day it affects all aspects of your life. Unless you have the right mind set to deal with it (patient caregiver atopic dermatitis) (Figure 1) [8].
Diagnosis
Family/general physicians were seen as the patients’ first point of contact during the early phase, which is the onset of symptoms. For patients with mild to severe conditions, this results in a delay in diagnosis and treatment until the symptoms worsen. Until the patients’ family doctor recommended a dermatologist, diagnosis was a significant challenge for them.
I wasn’t aware of the skin condition. Earlier, it was just itching and redness on skin. I went to my family physician but the medicine he gave never worked so I went to dermatologist. He told me it’s called atopic dermatitis (patient atopic dermatitis).
Since there is no known treatment for the condition, individuals frequently visit multiple dermatologists till they are satisfied with their treatment. This causes people to try variety of therapy options in a hit and trial manner, which either makes their diseases worse or temporarily, relieves the symptoms. Patients have also become afraid of other kind of conditions, including skin cancer, as a result of this. Some patients have raised concern of becoming frustrated over the unknown cause of the disease, resulting them to question themselves and give up on their prospects of a cure.
I went to the doctor and told him that it was a small pimple, but it has spread all over my face and later it starts paining as well. I could not sleep the whole night and felt itching. Doctor told me that it is a skin condition and it called daag khaj khujli (itchy rash and itching). It happens mostly on the corner parts of our body; I got scared while seeing it because I have heard a lot about skin cancer. The doctor told me there is nothing to worry about. It is “daag khaj khujli (itchy rash and itching) only” (patient atopic dermatitis).
After taking medicines, rashes go away for some time but appear again. Medicine is lifelong. No one knows about the disease (patient atopic dermatitis).
Treatment
First line of treatment: Understanding the underlying causes and course of the condition can take patients and caregivers up to three to four months. The first step is to see a family doctor and begin using medications, which are typically applied topically in most situations. Visiting dermatologist to get exact diagnosis and relief from pain and itch is a key milestone.
Second line of treatment: Patients anticipate instant relief once their medications have been started. They see dermatologists if there are continuous flare ups or if the pain does not go away. Duration of treatment varies depending on how severe and how quickly the symptoms spread to other body areas. Once the symptoms were under control, maintaining adherence to the treatment was considered as a challenge.
Third line treatment: The ideal outcome for the patient would be to get fully recovered, but for many, treatment lasts a lifetime. The main goal of current treatment is to provide the optimum quality of life while living with the condition.
Once a patient thinks that they continue to experience flare ups even after taking medicine, alternative therapies and home remedies are explored. Patients see their current treatment options as a complete cure for their disease. However, there is currently no cure for the disease, and the treatments given to patients are meant to control symptoms and provide temporary relief.
This is not a major condition that you must take three to four opinions, so the question is that we generally go to one doctor and they would prescribe the medicines, they wait for five days, it doesn’t work then you go to a general surgeon. It’s not like you would like to get multiple opinions for this. I haven’t found a solution for it yet and I am leaning more towards Ayurveda or other alternatives, today which I see works better on me than I would think of Allopathy, being honest that it is not something that I am even considering going to another doctor for treatment as they wouldn’t understand it and I don’t know whether there is understanding of what it is, so I am looking more at Ayurveda (patient atopic dermatitis).
Impact on quality of life
Lack of knowledge: Patients are confused about how their disease is progressing. Due to a lack of knowledge, they struggle to gather information on social media. Low disease awareness traps them in a vicious cycle of social stigma, fear of spreading to other parts of the body, being contagious to others, and sometimes confusing it with other diseases such as skin cancer. Additionally, they have a tough time finding the appropriate medical professional to treat them due to this.
Initially, there was only one white patch on my nose. No pain or anything, just a light coloured patch so I ignored that. It started spreading on my face but there were no other symptoms. We never felt like showing this to doctor. On TV, we see this kind of ‘daag, khaj and khujli (itchy rash and itching)’ advertisement, I thought it’s like that (patient atopic dermatitis).
Lifestyle: Due to social stigma, restricted socialization and isolation were seen. Patients live a limited and compromised life because they are unable to perform their daily tasks, which makes them dependent on their careers. It makes it challenging for the patients to carry out daily tasks. Winter requires them to pay special attention to their skin’s health and they often find it difficult to keep it moisturized. Lack of sleep spurred on by constant itching and dietary restrictions like consuming fermented or sour food. Maintaining a stress free lifestyle was viewed as a never ending challenge.
In our language we call it kharish (itch) but doctor told me some skin allergy. 8 months ago, I had this. I first noticed that I got itching feeling in the legs. I felt that dirty rainwater could be the cause of it. I felt that it is normal thing and slight itching started. I applied coconut oil and mustard oil but did not feel better from it. Day by day it increased.
Earlier normal itching was there and then slowly it increased. I used comb or spoon for itching on my leg. Itching was so bad that I did it continuously. I used to feel relief, but my hand never went away from that area (patient atopic dermatitis).
Emotional and financial: Less tolerance for stress and anger because of embarrassment and visible physical symptoms. Because they are unable to express their thoughts and feelings, they become more anxious, depressed and isolated. Financial burden occurs when the cost of the therapy and doctor visits makes it tough for them to manage monthly budgets. Since there is no cure, patients need to pay out of pocket for the medications. They are not supported by any insurance policies in terms of paying for their medical care and consultation costs.
On average four to five thousand Indian rupees, that includes doctor consultation and medicines. This is a lifelong skin disease so that adds to financial burden. GPs are not able to diagnose this, so we have to go to dermatologists, their charges are very high (patient atopic dermatitis).
Five hundred Indian rupees doctor’s fees and 1000 for medicines every month. We are a middle class family cannot afford the medical bills, but we have to do it for our kids (caregiver atopic dermatitis).
Conclusion
The main aspects of a patient’s journey coping with atopic dermatitis are highlighted in this study. Their trip reveals various problems that can be addressed by taking the lead on a few strategic measures that will benefit not only the patients and caregivers, but also the other stakeholders who may be involved along the way. One of the game changers in this disease area may be standard treatment procedure along with strong research backed data. When developing any kind of recommendations, patient expectations and experiences must be considered. Patients have expressed a need for patient support groups, specialized counseling on their condition from specialists, readily available medicines at affordable prices, authentic awareness material and most importantly, a cure for the disease. Simultaneously, it becomes critical that we not only discuss the patient burden of management of the disease, but also consider caregiver perspectives. Patients expectations can be met if multiple stakeholders from across the field work together to overcome these problems. We must all work together to address this issue and advocate for changes that will benefit patients and caregivers so that they do not perceive this disease as a burden. There is a lack of literature in India on the disease burden, epidemiology and significant delay in the diagnosis and management of AD.
References
- Xu X, et al. Factors influencing quality of life in children with atopic dermatitis and their caregivers: A cross sectional study. Scientific Reports, Vol. 9, No. 1, 2019, pp. 15990.
[Crossref] [Google Scholar] [PubMed]
- Ali F, et al. Counting the burden: Atopic dermatitis and health related quality of life. Acta Dermato Venereologica, Vol. 100, No. 12, 2020, pp. 330-340.
[Crossref] [Google Scholar] [PubMed]
- Kelly KA, et al. Skin disease in children: Effects on quality of life, stigmatization, bullying, suicide risk in pediatric acne, atopic dermatitis and psoriasis patients. Children, Vol. 8, No. 11, 2021, pp. 1057.
[Crossref] [Google Scholar] [PubMed]
- Howells LM, et al. Development and initial testing of a new instrument to measure the experience of eczema control in adults and children: Recap of atopic eczema (RECAP). British Journal of Dermatology, Vol. 183, No. 3, 2020, pp. 524-536.
[Crossref] [Google Scholar] [PubMed]
- Ferrucci SM, et al. Factors associated with affective symptoms and quality of life in patients with atopic dermatitis. Acta Dermato Venereologica, Vol. 101, No. 11, 2021, pp. 00590.
[Crossref] [Google Scholar] [PubMed]
- Leong K, et al. Multidisciplinary management of chronic atopic dermatitis in children and adolescents: A prospective pilot study. Journal of Dermatological Treatment, Vol. 33, No. 2, 2022, pp. 822-828.
[Crossref] [Google Scholar] [PubMed]
- Xu X, et al. Concordance between physician rated and caregiver perceived disease severity in children with atopic dermatitis: A cross sectional study. Acta Dermato Venereologica, Vol. 100, No. 18, 2020, pp. 1-7.
[Crossref] [Google Scholar] [PubMed]
- Olsson M, et al. The cost of childhood atopic dermatitis in a multi-ethnic Asian population: A cost of illness study. British Journal of Dermatology, Vol. 182, No. 5, 2020, 1245-1252.
[Crossref] [Google Scholar] [PubMed]