Case Report - International Journal of Medical Research & Health Sciences ( 2022) Volume 11, Issue 11
Plexiform Neurofibroma of the Occipital Scalp with Occipital Bone Defect and Neurofibromatosis Type 1- A Case Report in a Tertiary Care Center, AP, India
P. S. Raja Ravi kumar1, Bomidi Sudha Rani2*, K. Meghana Krishna3 and K. Sindhura42Department of Radiodiagnosis, Andhra medical college, KGH, Andhra Pradesh, India
3Medical student, Andhra medical college, KGH, Andhra Pradesh, India
4Postgraduate student, Andhra Medical College, AMC, Andhra Prsdesh,, India
Bomidi Sudha Rani, Department of Radiodiagnosis, Andhra medical college, KGH, Andhra Pradesh, India, Email: radiologysudha@gmail.com
Received: 20-Oct-2022, Manuscript No. ijmrhs-22-77876; Editor assigned: 26-Oct-2022, Pre QC No. ijmrhs-22-77876; Reviewed: 02-Nov-2022, QC No. ijmrhs-22-77876; Revised: 07-Nov-2022, Manuscript No. ijmrhs-22-77876; Published: 30-Nov-2022, DOI: 0
Abstract
Plexiform neurofibromas are virtually pathognomonic of NF-1. They are generally bulky tumours usually associated with major nerve trunks and plexuses. They are rope-like, diffusely, infiltrating, non-circumscribed lesions that resemble a bag of warms. The scalp and orbits are common sites. Most PNFs remain benign and only 10%-15% of deep-seated PNFs are at risk of developing into MPNSTs. Here we report a case of PNF of the occipital scalp in a 12-year-old male child with an occipital bone defect associated with NF-1.
Keywords
Neurofibromatosis type-1(NF1), Plexiform Neurofibroma (PNF), Occipital bone defect, Cafe-Au-Lait spots, Lisch nodules, Malignant Peripheral Nerve Sheath Tumor(MPNST)
Introduction
Neurofibromatosis is not a single entity, but a group of genetically and clinically distinct multisystem disorders with few overlapping features. They are the most common CNS tumour predisposition syndromes with both neoplastic and non-neoplastic manifestations. Two types of NF are widely recognized, NF1 and NF2 and 3rd related rare disorder is schwannomatosis. Neurofibromatosis type 1 (NF-1) is an autosomal dominant disorder [1]. It is one of the most common CNS single gene disorders affecting 1 in 3000 live births and is caused by mutation of the NF-1 gene on chromosome 17 [2]. Approximately half of all cases are familial. It has a penetrance of almost 100% and nearly 50% are sporadic and represent new mutations. There is no gender predilection. The Most common nonneoplastic CNS lesions are multiple waxing and waning dysplastic white matter lesions. Uncommon non-neoplastic CNS lesions include macrocephaly, subependymal glial nodules, hydrocephalus, and dural ectasia. Arteriopathy occurs in very few cases. CNS neoplastic lesions can be found in both the central and peripheral nervous systems. Benign neoplasms include Neurofibroma and Schwannoma. Malignant tumours include MPNSTs and gliomas [3]. Neurofibromas are the most prevalent benign predominantly peripheral nerve sheath tumours appearing as soft, skin-coloured papules or small subcutaneous nodules. They are composed of Schwann cells, fibroblasts, perineurial cells, and mast cells in a variably myxoid background. There are three main types of Neurofibromas: cutaneous, subcutaneous/diffuse cutaneous, and plexiform [4]. The term “Plexiform Neurofibroma” is applied to neurofibromatosis of nerve trunks that expands a nerve into a large tortuous mass of fibres that has a“ bag of worms” appearance [5]. Plexiform neurofibromas are the least common variants and are essentially pathognomonic of Neurofibromatosis type 1 (NF-1) [6 ]. Neurofibromatosis type 1 (NF-1) is characterized by cutaneous lesions like Cafe-Au-Lait macules, axillary/inguinal freckling; eye abnormalities like Lisch nodules and optic gliomas and bone signs like sphenoid dysplasia's [2]. We report a case of Plexiform Neurofibroma of the occipital scalp with an underlying bone defect in a 12-year-old male child associated with NF-1.
Case Presentation
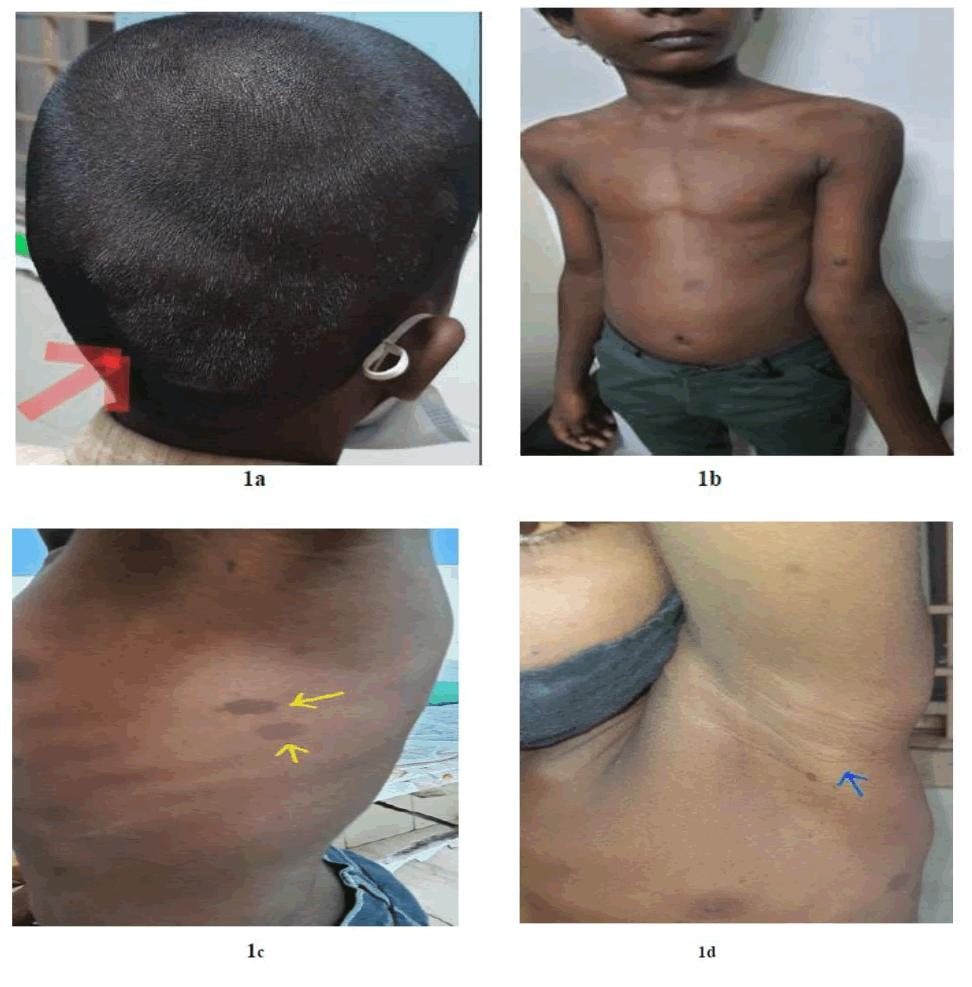
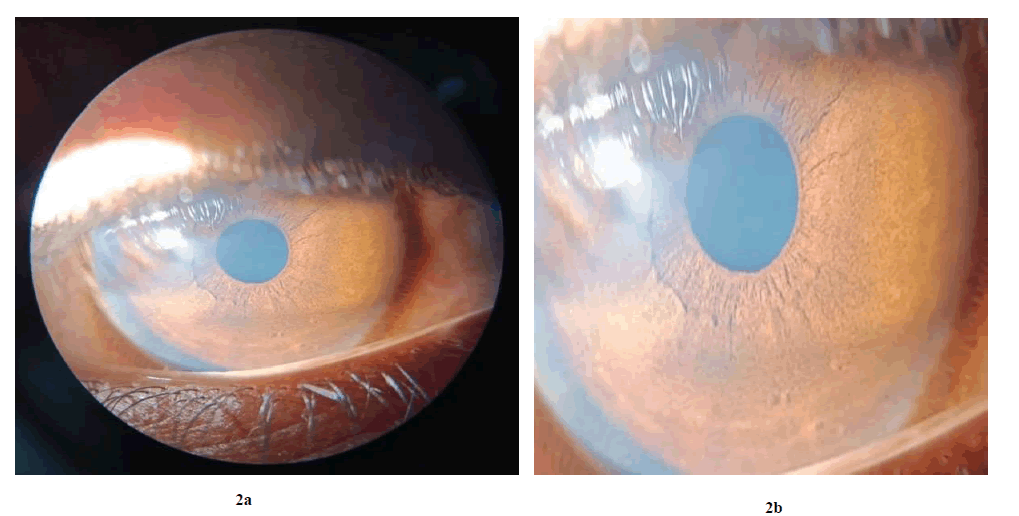
A 12- year- old, male child presented with a 2- year history of gradually progressive painful swelling over the right side of the scalp involving the Occipito-cervical region. No h/o fall from height and scalp trauma. Clinical examination showed a diffuse swelling over the right Occipito-cervical region of a size of 8 cm x 6cm approximately (Figure 1a). It was soft to firm, compressible, tender and non fluctuant on palpation. The skin over swelling was normal and no bruit was auscultated. There were no palpable adjacent lymph nodes. Multiple cutaneous neurofibromas are present all over the body Multiple (more than 6) café-au-lait spots of size greater than 0.5 cm were present all over the body (Figures 1b and 1c). Axillary freckling was present in the left axilla (Figure 1d). Lisch nodules are present in both eyes (Figures 2A and 2B). A family history of NF-1 is present. The boy had no neurological deficits/hearing loss/cognitive impairment. The patient was referred to our dept for USG evaluation, CT, MRI, and guided procedure
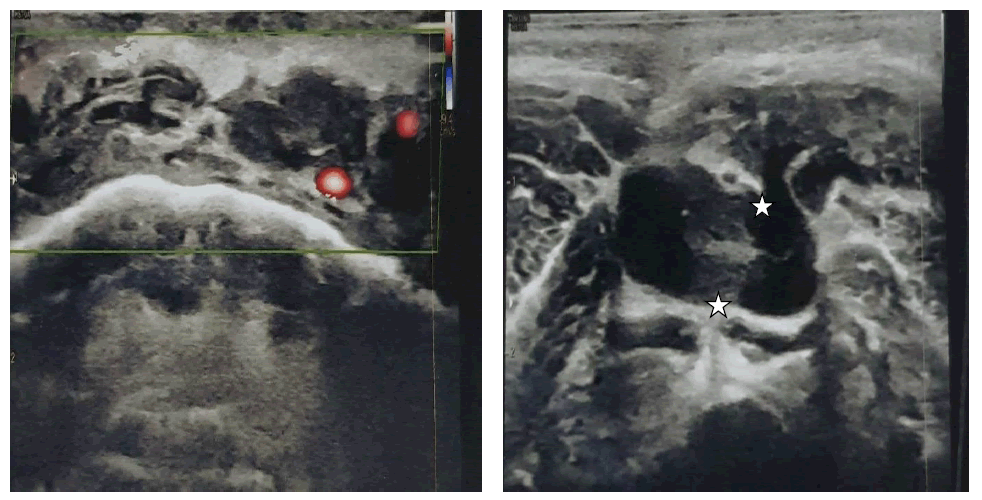
On USG ill-defined hypoechoic lesion (approximately 54 mm x 34 mm x 45mm) in the scalp at the right parietooccipital region extending into the inter and intramuscular planes of the posterior aspect of the neck (Figure 3). On colour Doppler no abnormal significant colour uptake.
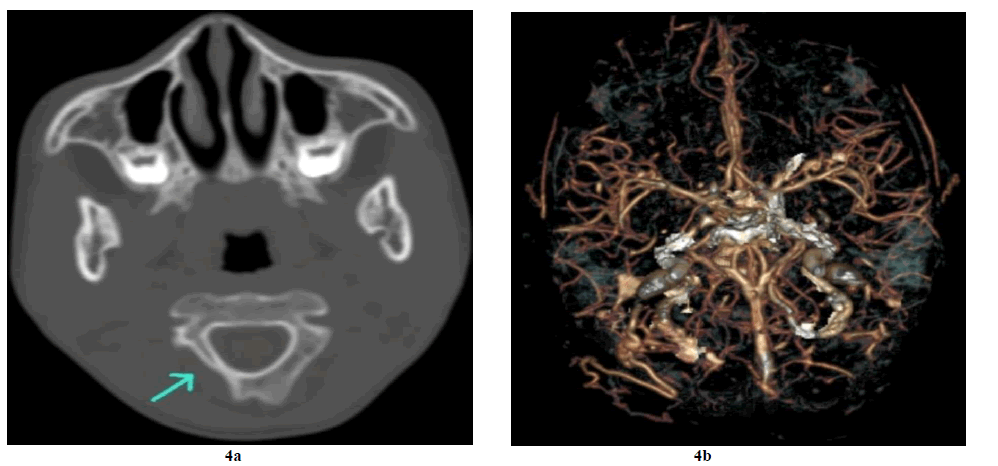
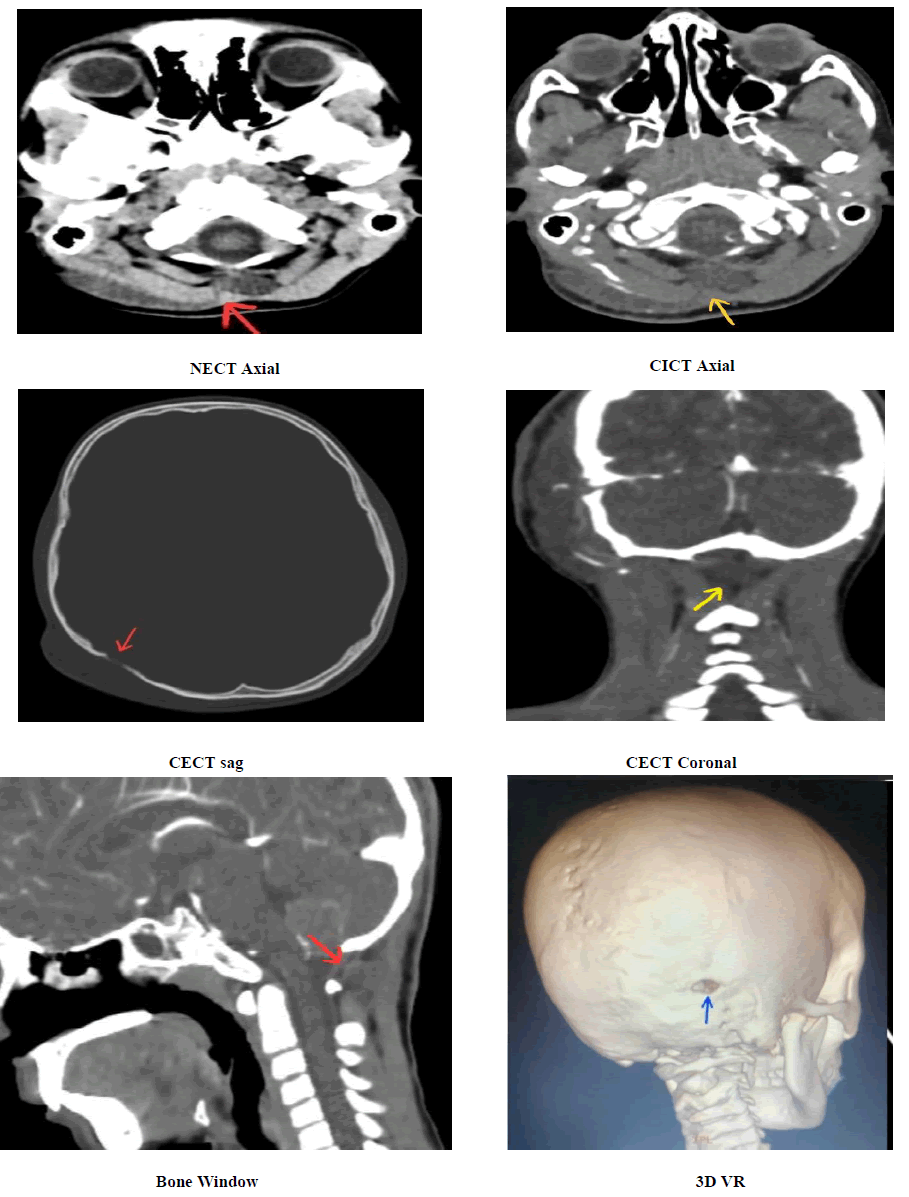
NECT shows a soft tissue attenuation mass lesion of size 7 x 2.2 cm x 1.3 cm in the occipital scalp region on the right side and is seen extending up to the nape of the neck, the ligament nuchae at the spinous process of C1/ C2. The above mass lesion is not showing any significant enhancement in contrast and no e/o intracranial extension on CECT. On the bone window, there is underlying bone erosion and a hypoplastic posterior arch of C1 on the right side (Figure 4a). Rt posterior occipital artery and venous plexus are prominent on CTA (Figure 4b and Figure 5).
Figure 5. Non-Contrast Computed Tomography (NCCT) of the head revealed a soft tissue density mass lesion involving the right occipital region extending posteromedially towards the spinous process of C1 through the inter & intramuscular planes of Rectus Capitus Post Major (RCPM), Obliqus Capitis Inferior(OCI), Semispinalis Capitis (SSC), Spenius Capitis (SC) and trapezius. There is a small bony defect in the right occipital bone
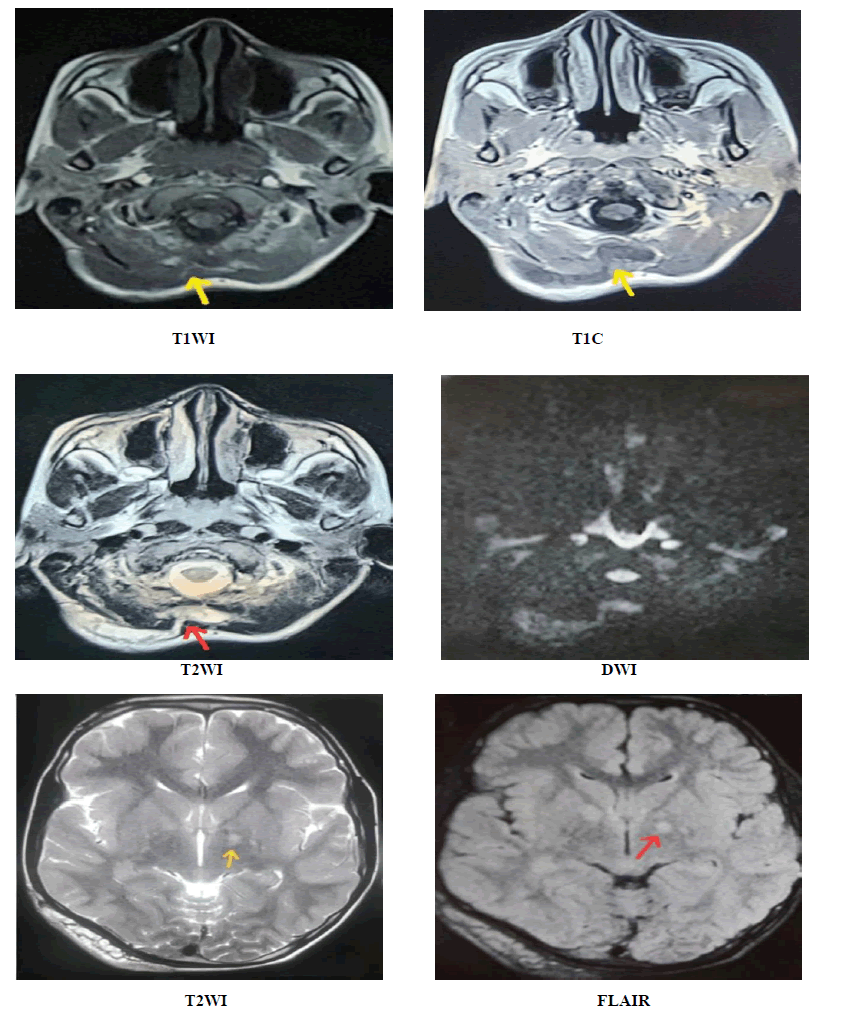
MRI showed a multinodular confluent mass lesion with some flow voids seen in the right occiput region in the subcutaneous planes insinuating into intramuscular planes till the base of the skull in the midline nuchal region. The lesion is iso to hypointense on T1 and heterogeneously hyperintense on T2WI demonstrating multiple target signs. The above lesion is showing some mass effect on surrounding structures with no perilesional oedema, and no intralesional cystic areas. No diffusion restriction. The underlying occipital bone is thinned out and eroded. T1C shows minimal post-contrast enhancement. The above findings are in favour of plexiform neurofibroma probably arising from the major nerve trunk which is the greater occipital nerve. MRI brain also revealed few T2/FLAIR hyperintense foci in bilateral basal ganglia midbrain and cerebellum with no contrast enhancement (Figure 6). Finally, the above MRI findings were suggestive of plexiform neurofibroma associated with NF1.
Figure 6. MRI Multinodular confluent mass lesion with some flow voids within seen in the right occiput region in the subcutaneous planes insinuating into inter and intramuscular planes till the base of the skull in the midline. The lesion is hypointense on T1 and hyperintense on T2WI demonstrating multiple target signs. The above lesion is showing some mass effect on surrounding structures. T1C shows minimal enhancement but no cystic areas within or no perilesional oedema. MRI brain also revealed few T2/FLAIR hyperintense foci in bilateral basal ganglia midbrain and cerebellum.
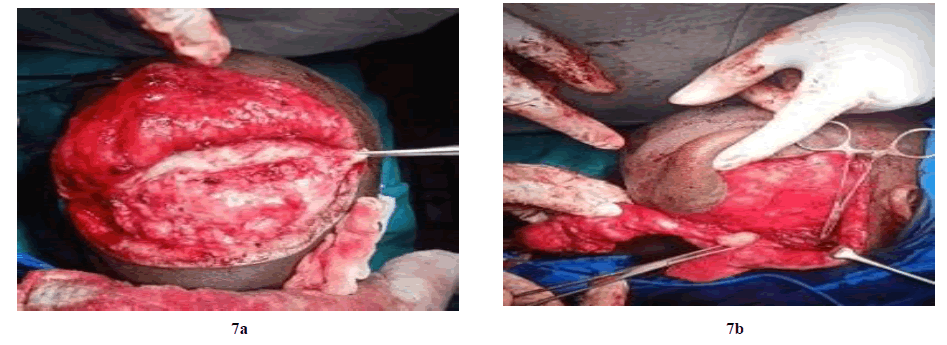
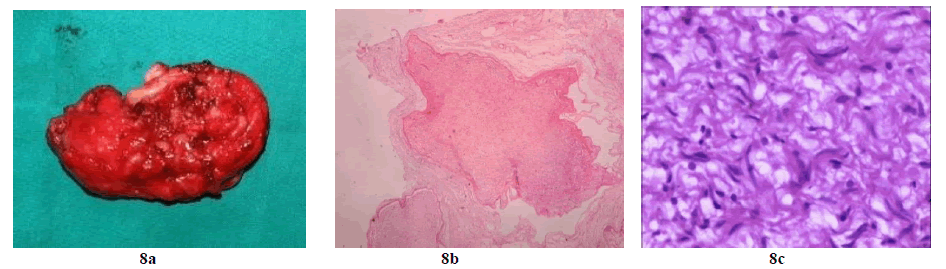
After a complete evaluation, the patient was planned for surgical excision of the lesion. Intra-operatively, there was a mass of size 8x6x3cm extending superiorly from the base of the skull in the midline at the nape of the neck to the occipital scalp region through the inter and intramuscular planes (Figure 7a and 7b). Excision of swelling done and good hemostasis achieved. Suturing was done with Ethilon. Postoperatively the patient was uneventful and he was discharged from the hospital on the eighth day. The operative site healed by primary intention. The Specimen was sent for histopathological examination (Figure 8a). Microscopic examination revealed an unencapsulated lesion composed of fascicles of proliferating benign neural cells separated by fibromyxoid stroma giving the nodular appearance, and wavy hyperchromatic nuclei with no evidence of increased mitotic activity or necrosis (Figure 8b and 8c). These features are suggestive of Neurofibroma-Plexiform Neurofibroma.
Discussion
Plexiform neurofibromas are usually diagnosed in early childhood. They are found in approximately 30% of patients with NF1 and mostly are solitary lesions (91%) [6,7]. Scalp plexiform neurofibromatosis was first reported by Scott in 1906 [8]. The term "plexiform" is derived from the Latin verb "plex", which means to interweave or braid or plait together and it denotes a complex network of interlacing or interwoven blood vessels or nerves, as exists in this entity. These entities consist of multiple, twisted masses that grow along the axis of a large nerve, infiltrating and separating normal nerve fascicles. They are 2 types, nodular and diffuse. Diffuse plexiform neurofibroma is also called elephantiasis neurofibromatosis which shows overgrowth of epidermal and subcutaneous tissue along with a wrinkled and pendulous appearance. The major cause of mortality in NF1 patients is the transformation of plexiform neurofibroma into MPNSTs.
Neurofibromatosis type-1(NF1), also known previously as von Recklinghausen’s disease, is a multisystem neurocutaneous genetic disorder the most common phakomatosis, and a RASopathy. Involving the cutaneous, Ocular, musculoskeletal, central, and peripheral nervous systems, CVS/haematological, vascular, endocrine systems, Pulmonary, and GIT [9]. The National Institute of Health (NIH) developed the seven main criteria for the diagnosis of NF-1. Two or more of the following criteria are required for the diagnosis of NF-1:
• Six or more café-au-lait spots of size greater than 0.5cm in children or greater than 1.5 cm in adults,
• Axillary or groin freckling,
• Two or more cutaneous neurofibromas or one plexiform neurofibroma,
• Optic glioma,
• Two or more iris Lisch nodules,
• Bony dysplasias (sphenoid wing dysplasia, pseudoarthrosis, other distinctive bone lesions), and
• A first-degree relative with NF-1 [10].
In our case, 6 criteria are fulfilled to diagnose it as NF
Ultrasound, Computed Tomography (CT), and Magnetic Resonance Imaging (MRI) are useful in the diagnosis and characterization of Plexiform neurofibromas. MRI is the most useful imaging modality to determine tumour size, extent, and neurogenic origin due to its high contrast resolution [11]. In our case, based on the above imaging features, the neurogenic origin is probably from the greater occipital nerve trunk. The Greater Occipital Nerve (GON) is the medial branch of the dorsal ramus of the second Spinal Nerve (C2); It emerges below the posterior arch of the atlas, curls around the lower border of the Obliquus Capitis Inferior muscle (OCI) and passes cranially superficial to this muscle across the roof of the suboccipital triangle. Clinical management for the PNF requires a multidisciplinary approach. PNFs are difficult to manage surgically as they are extensively infiltrative, highly vascularized, and tend to recur. However Surgical intervention is the current treatment option for PNF when it causes disfigurement, compromises functionality, and the risk of malignant transformation. Complete resection is often difficult because of the extensive and infiltrative nature of these lesions. Common complications are excessive bleeding and infection.
Conclusion
We report a proven case of plexiform neurofibroma of the occipital scalp associated with NF1 which is a rare condition and to the best of our knowledge, only very few cases had been reported in the literature in the past. In this case report, we highlighted the role of the multimodality approach in diagnosing NF-1.
Declarations
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Kankane, Kumar V., Gaurav Jaiswal, and Tarun K. Gupta. "Congenital extra calvarial plexiform neurofibroma in occipito-cervical region with Occipital bone defect with neurofibromatosis type 1 and segmental neurofibromatosis: Case report and review of literature." Journal of Pediatric Neurosciences, Vol. 11, No. 4, 2016, p. 295.
Google Scholar Crossref - Rafik, Amine, et al. "Unusual evolution of plexiform neurofibroma in the scalp: a case report." World Journal of Plastic Surgery, Vol. 7, No. 1, 2018, p 128.
Google Scholar - Dawe, Gemma. "Anne G. Osborn Osborn's Brain: Imaging, Pathology, and Anatomy Amirsys, Salt Lake City, UT, 2012. 1300 Pages. Price£ 194.65 (hardcover, Amazon)." 2014, pp 663-63.
Google Scholar Crossref - Messersmith, Lynn, and Kevin Krauland. "Neurofibroma." StatPearls [Internet]. StatPearls Publishing, 2022.
Google Scholar - Pukar, Mahesh M., Rishabh H. Gadhavi, and Sohank G. Mewada. "Plexiform neurofibroma of the scalp a rare entity–a case report and review." International Journal of Research in Health Sciences, Vol. 2, No. 2, 2014, pp. 711-14.
Google Scholar - Korf, Bruce R. "Plexiform neurofibromas." American journal of medical genetics, Vol. 89, No. 1, 1999, pp. 31-37.
Google Scholar Crossref - Singh, Ram J., et al. "Plexiform neurofibroma of the scalp with a bony defect: A case report and review of literature." Journal of Pediatric Surgery Case Reports Vol. 85, 2022.
Google Scholar Crossref - Júnior, Sérgio F.A., et al. "Neurofibromatosis type 1: State-of-the-art review with emphasis on pulmonary involvement." Respiratory Medicine Vol. 149, 2019, pp. 9-15.
Google Scholar Crossref - McVeigh, Terri P., et al. "A pilot study investigating the feasibility of mainstreaming germline BRCA1 and BRCA2 testing in high-risk patients with breast and/or ovarian cancer in three tertiary Cancer Centres in Ireland." Familial Cancer, 2022, pp. 1-15.
Google Scholar - Rallis, Efstathios, and Dimitra Ragiadakou. "Giant plexiform neurofibroma in a patient with neurofibromatosis type I." Dermatology Online Journal, Vol. 15, No. 5, 2009.
Google Scholar Crossref - Ahn, Min S., Robert K. Jackler, and Lawrence R. Lustig. "The early history of the neurofibromatoses: Evolution of the concept of neurofibromatosis type 2." Archives of Otolaryngology-Head & Neck Surgery Vol. 122, No. 11, 1996, pp. 1240-49.
Google Scholar Crossref