Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 9
Preventing Transfer of Asymptomatic COVID-19 Positive Postnatal Women to COVID-19 Negative Zone: A QI Report
Vidhi Chaudhary1*, Manju Puri1, Swati Aggarwal1, Shilpi Nain1, Anima Ghosh1, Pushpa Dilhan1, Nishtha Jaiswal1 and Srishti Goel22Department of Neonatology, Kalawati Saran Children’s Hospital, New Delhi, India
Vidhi Chaudhary, Department of Obstetrics and Gynaecology, Lady Hardinge Medical College, New Delhi, India, Email: drvidh@gmail.com
Received: 25-Aug-2021 Accepted Date: Sep 23, 2021 ; Published: 30-Sep-2021
Abstract
Background: Asymptomatic cases of COVID-19 infection are a key contributor to the spread of coronavirus disease. Despite following the national guidelines for the prevention of the COVID-19 infection, a considerable number of asymptomatic COVID-19 positive postnatal women were found admitted in the COVID-19 non-suspect postnatal wards (green zone) at our facility. We undertook a Quality Improvement (QI) initiative starting from 1st July 2020 to admit 100% Postnatal Women (PNW) with a COVID-19 negative report in the green zone by the end of 4 weeks. Method: A fishbone analysis of the problem was done. The Point of Care Quality Improvement (POCQI) methodology was used. There were two COVID-19 non-suspect postnatal wards in the facility out of which one ward was designated as the holding zone for PNW awaiting reports and the other as a green zone for COVID-19 negative PNW. Result: The percentage of COVID-19 positive women of the total number of women admitted to green postnatal wards decreased from 9.1% to 0% at the end of the 4 weeks after 4 PDSA cycles and was sustained over subsequent months. Conclusion: The success of the QI project was attributable to effective communication and the dynamic adoption of solutions to problems encountered during the project.
Keywords
COVID-19, Postnatal women, QI, PDSA cycle, Infection
Introduction
A worldwide outbreak of Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-COV-2) infection also known as COVID-19 disease led to the isolation of COVID-19 infected patients in dedicated COVID-19 zones to contain the spread of the virus [1]. COVID-19 suspects were defined as those belonging to hotspot or containment areas, those with symptoms, or close contacts of COVID-19 positive cases; as described in clinical criteria laid down by the Ministry of Health (MOH) [2]. All pregnant women, who required admission in our obstetric unit were triaged at the entry by casualty residents and admitted to various dedicated zones as per their COVID-19 status. Universal screening of all admissions by nasopharyngeal swab the RTPCR-COVID-19 test was conducted. Pregnant COVID-19 nonsuspects after delivery were shifted to the non-suspect postnatal ward (green zone). A high number of asymptomatic COVID-19 positive cases were seen (10%) among green zone Postnatal Women (PNW) despite interventions like universal testing, limited admissions, and the creation of three coded zones. There were three labor zones: red zone, orange zone, and green zone for COVID-19 positive, COVID-19 suspect, and COVID non-suspect laboring women, respectively. The COVID positive postnatal mothers were shifted to the red zone ward whereas suspect PNW were either discharged from the orange zone labor room itself or transferred out only after they received a negative report of COVID-19. The non-suspects were shifted to green postnatal wards without waiting for their reports for accommodating waiting for non-suspect laboring patients. The obstetric unit has two Postnatal (PN) wards on two separate floors with a bed strength of thirty-three in each, to which COVID-19 non-suspects Postnatal Women (PNW) are transferred. However, despite all the measures being in place, a considerable number of asymptomatic non-suspect women shifted to the green postnatal wards were later found to be positive for the COVID-19 infection based on their initial screening test, causing concern among fellow patients as well as the Health Care Workers (HCWs) involved in their management. Knowing that the virus spreads through close contact and droplets, an urgent need was felt for preventing the transfer of these asymptomatic COVID positive postnatal women awaiting reports to green zones.
Available Knowledge
The new coronavirus also known as COVID-19 was first discovered in a cluster of patients with symptoms of pneumonia of unknown cause in Wuhan, Hubei Province, China in early December 2019 [3]. It is primarily transmitted by inhalation or contact with infected droplets. Most of those infected are asymptomatic [4]. There are no recommended medical treatments available and supportive measures are the mainstay of management. The isolation of those infected with the virus to a dedicated COVID-19 zone for care, and contact tracing is crucial in the prevention of transmission of the virus in medical facilities. WHO recommended methods such as maintaining social distancing, hand hygiene with alcohol-based hand rubs, wearing personal protective equipment such as surgical face masks (FFP2) or N95 respirators, and avoiding close contact with patients or suspected patients [5,6].
Rationale concept and reasons why the intervention(s) was expected to work: Universal testing of all the pregnant and non-suspect Postnatal Women (PNW) requiring admission in the green zone was done as per department policy. However, minimal time for reporting was 3 days, so there was a subsequent risk of infection to other mothers till the report was available. We realized that though non-suspect obstetric women were triaged to the green zone after initial screening as per MOH criteria, they may have been asymptomatic COVID-19 positive at the time of presentation. They delivered and were transferred to green postnatal wards. Reports of some would be available but quite often the reports would arrive after their transfer to the ward. They had the potential to spread the infection to others who tested negative. Hence, creating a holding postnatal zone for separating the PNW with COVID-19 negative reports from positives in non-suspect postnatal women awaiting reports was expected to reduce the positivity in the green zone.
Materials and Methods
Our obstetric unit is a heavy load facility with an average of more than one thousand deliveries per month and constraints of space and beds often resulting in sharing of beds with patients in non-COVID-19 times. During COVID-19 times, we followed a policy of one bed, one patient to maintain social distancing. The load of the facility was reduced during the COVID-19 pandemic initially due to the lockdown, and then by policy decision of deferring admissions of lowrisk antenatal women till these were in advanced labor. The patients were segregated into various designated zones as per the guidelines, but it was noted that several asymptomatic COVID-19 positive postnatal women were found among non-suspect PNW in the non-suspect green postnatal wards despite multiple interventions such as universal testing, limited admissions, and the creation of three coded zones.
Specific Aims
The SMART aim was to admit 100% postnatal women with COVID-19 negative reports to the green PNW by the end of 4 weeks starting from 1st July 2020 weeks and to maintain sustained results in subsequent months.
Interventions
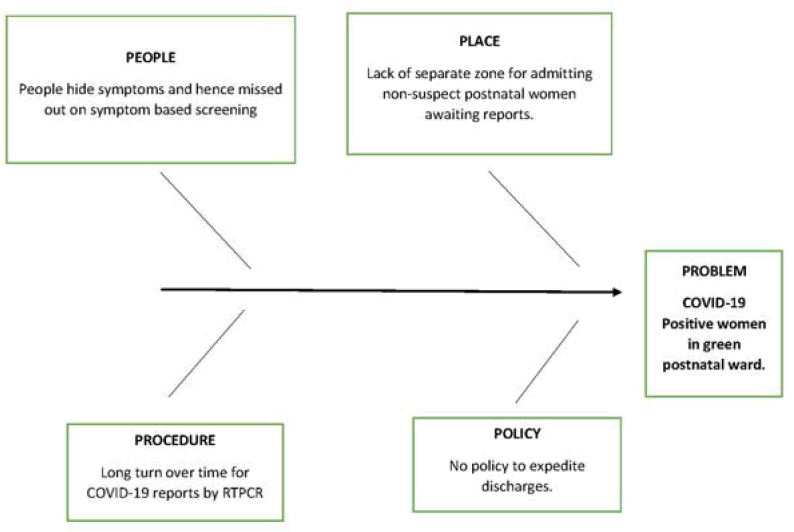
A Quality Improvement (QI) team was made, including the head of the department, consultant in charge of postnatal wards, Nursing Officers (NO) of postnatal wards and labor rooms, residents, and Neonatology consultant. As an initial action, a joint meeting with all QI members was held. The problem was analysed using Fishbone analysis (Figure 1) and change ideas were listed. We had three options. The first was to hold all postnatal women awaiting reports in the labor room till the reports were available. It was not found feasible due to a constant need for vacant beds, for waiting for laboring women due to heavy patient load. The second option was to admit all women awaiting reports in the orange zone but due to limited availability of beds and increased requirement of the workforce, PPEs in these areas due to shorter duty hours and mandatory quarantine after 2-week duty in these areas, the QI team decided against this option. The third option was to create a holding zone where all non-suspect PNW awaiting COVID-19 reports can be transferred which seemed achievable.
One of the two postnatal wards was designated as a holding zone for transferring PNW who awaited COVID-19 reports and the other as the green zone where PNW with negative reports were transferred. COVID appropriate precautions as outlined by the Ministry of Health, Government of India were followed by the HCW while attending PNW [7].
The HCWs were required to wear level 2 PPE (Personal Protective Equipment) in the holding zones as only asymptomatic PNW were shifted there who were anyways less infectious than symptomatic women even if they came positive [8]. Thus, the investment in the holding zone in terms of manpower (due to the quarantine policy in orange zones), as well as infrastructure (requirement of PPEs), was much lower than in the orange zones [2,7]. PNW from the holding areas were transferred to green or red zones once their reports were received. Any positive case was informed to the nursing officer of the ward for rapid transfer of that woman to the designated red zone, followed by contact tracing and sanitization of the area and those tested negatives were either discharged from the holding area or transferred to the green ward with all tested negative PNW. Data were collected twice every week, followed by every week by the NO of the holding area for the number of positives among the non-suspects PNW in green and holding zones to assess the trends.
Study of Interventions
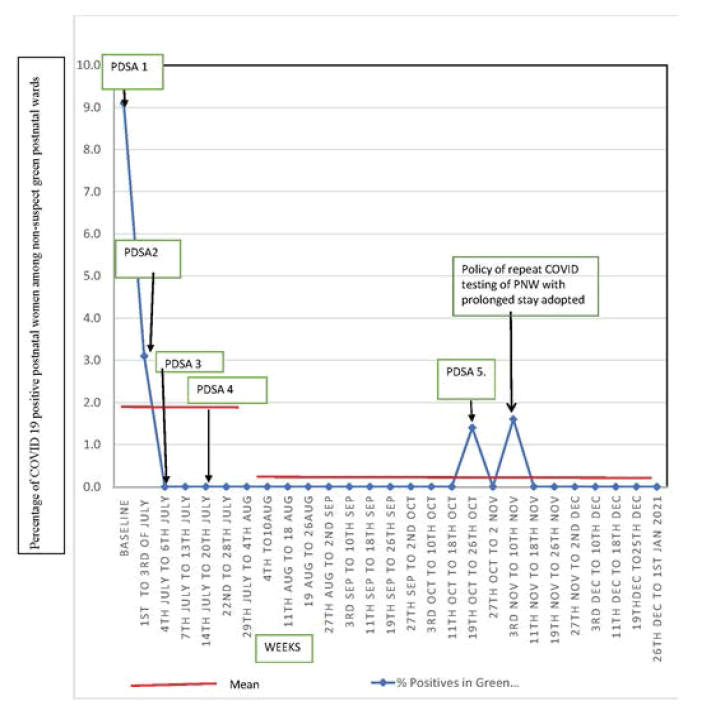
Baseline data was collected from 1st to 30th of June 2020 from designated green postnatal wards which received only COVID-19 non-suspect, postnatal women, from COVID-19 non-suspect labor room. The total number of deliveries in June 2020 was 484 out of which 220 were COVID-19 non-suspects pregnant women who delivered in the green zone labor room, and 264 COVID-19 suspect pregnant women delivered in the orange zone labor room. The total number of transfers of non-suspect postnatal women in green postnatal wards was 198 of which 18 later were found COVID-19 positive based on their screening test at admission. Hence positivity rate for COVID-19 infection was 9.1%. This was 20% of total COVID-19 patients (n=89) admitted in our obstetric unit during this period. The Point of Care Quality Improvement (POCQI) methodology using multiple Plan-Do-Study-Act (PDSA) cycles as shown in Table 1 was adopted [9,10].
| Cycle | Plan | Do | Study | Act |
|---|---|---|---|---|
| PDSA 1 | To create a holding zone in the non-suspect postnatal ward (1/7/20-3/7/20) | A Meeting of the QI team with concerned stakeholders was held. One of the two postnatal wards was converted to a holding zone for non-suspect PNW awaiting reports and the other as a green zone for negative women. The concerned Nursing Officers (NO) and residents were informed | The data was initially reviewed on daily basis. %positive in green zone=1/32=3.1% %positive in holding zone=3/35-8.5% A non-suspect PNW awaiting report was found admitted in the green postnatal ward that subsequently came out positive. We realized that there was a lack of communication among health care workers regarding transfer policy due to changes in staff in some shifts. | Adapt: Need to strengthen the check at the entry to designated green and holding at the time of receiving admission. Lessons learned: Communication is essential for any change idea to work. |
| PDSA 2 | Dissemination of information about the creation of holding and green postnatal wards to all residents and NOs of the department. (4/7/20- 6/7/20) | Online meeting with all concerned residents and NOs was held and a written circular was generated which was also circulated on social media groups. The NO’s of the green postnatal ward was requested to receive PNW only after checking the negative COVID-19 report. (There were no positives in the obstetric unit) | Marked improvement was observed from 4th July to 6h July with no woman coming positive from green postnatal wards. %positive in green zone-0/24=0 %positive in holding zone=0/32=0 However, it was observed that it was difficult to ensure the availability of beds in the postnatal green wards at all times due to an increase in several deliveries. | Adapt: A need was felt to expedite the discharges of PNW from green wards and reduce their hospital stay. Lesson learned: Continuous monitoring helps in the early identification of problems. |
| PDSA 3 | Decongestion of the postnatal wards by timely discharges to prevent overcrowding. (7/7/20-14/7/20) | A meeting was held with concerned neonatology consultants and obstetric consultants to expedite the discharges of mothers with babies promptly. The patients from the holding zone were discharged soon after their COVID report was available. The neonatal consultant was telephonically informed about the report so that baby’s immunization and baseline check was completed timely and discharge was expedited. Daily census of occupied and vacant beds was posted on departmental social media groups so that discharges were triggered whenever occupancy of wards exceeded 75%. This involved daily communication by QI team members to the ward residents to discharge PNW. | There were no positive cases in the green zone at the end of next week. %positive in green zone-0/32=0 %positive in holding zone=0/45=0 | Adapt Lesson learned: Solutions to problems are available if all concerned are in the team |
| 15/7/20-21/7/20 | The same interventions were continued. | %positive in green zone-0/29=0% %positive in holding zone=2/54=3.7% At the end of 3 weeks, a problem of shortage of beds in the holding zone was encountered due to delay in reports consequent to malfunction in the lab | Adapt: It was realized that there is a need to reduce the turnover time for discharges in the holding zone as well. | |
| PDSA 4 | Change in discharge policy in holding zone. (22/7/20- 28/7/20) | A QI meeting was held and the decision was taken to discharge PNW awaiting reports after informed consent for home isolation after 48 hours of delivery. The patients were followed up via telemedicine and notified if found to be positive. Also, buffer rooms were created in both the zones to accommodate patients in case any of the zones were full. | There were no positive cases in the green zone in the next week. %positive in green zone-0/30=0% %positive in holding zone=2/52=3.8% We achieved 100% admission of COVID-19 negative PNW in the green zone. Further weekly monitoring continued for sustainability. There was 1 positive PNW in October (26/10/20) from the green postnatal ward. The woman was initially COVID negative but when she was retested before undergoing resuturing of her abdominal wound, she came out to be positive. It was found that the woman had a prolonged stay in the hospital due to a wound infection. | Adapt: It was realized that there was a need to segregate mothers requiring prolonged stay as they were at high risk to acquire COVID-19 infection during their stay and there was no policy of routine repeat testing for them. |
| PDSA 5 | To segregate PNW requiring prolonged admission in a separate dedicated room in the green postnatal ward. (27/10/20-2/11/20) | QI team Communicated to NO of respective wards and a room for PNW with prolonged stay was created in the green zone. | Reduction in positives in the green postnatal ward to 0% again. | Adapt: Continue to refine ideas. |
Measures
The data was collected by the nursing officer of the postnatal ward who was also a QI member, from the admission registers maintained by the Nursing Officers (NOs) of the respective wards. In addition, a social media group was made by the QI team leader including all the concerned stakeholders, where a daily morning census of transfers to postnatal wards along with any COVID-19 positive case was posted. This ensured the completeness and accuracy of data. The data were collected daily and analysed twice weekly followed by a weekly basis for 4 weeks for a percentage of positives in each zone. The monitoring is still being continued.
Analysis
All data were recorded on a Microsoft Excel sheet daily for several positives in the non-suspect postpartum ward (holding and green zones). The total number of transfers in the PN ward at the end of each week was also recorded. Quantitative data were reported as mean and percentages. To understand trends within the data, time-series charts were used. We decided to use the percentage of COVID-19 positive women out of the total number of women admitted to postnatal green wards as our outcome indicator to assess the effectiveness of our interventions.
Results
Our main outcome measure was the percentage of COVID-19 positive women out of a total number of women admitted to green postnatal wards which decreased from 9.1% to 0% at the end of the 4 weeks after 4 PDSA cycles, thereby achieving 100% admissions of COVID-19 negative PNW in the green zone. The total number of deliveries in the month starting 1st July 2020 to 28th July was 574 out of which 324 COVID non-suspects, women delivered in the green zone labor room, and 256 COVID-19 suspects delivered in the orange zone labor room. There were 147 transfers of COVID-19 negative postnatal women in the green postnatal ward and 218 transfers of non-suspect PNW is awaiting reports to holding postnatal ward. The positivity rate of the holding zone at the end of 4 weeks was 3.2% (7/218). A time-series chart was plotted from the collected data (Figure 2). Another PDSA cycle was undertaken in October when a positive case was found in the green ward after a prolonged stay. Though the positivity rate remained 0% in the green zone for most of the subsequent week, there was one case of COVID-19 positive PNW in November despite QI measures. This PNW had a prolonged hospital stay due to her newborn being in the neonatal intensive care unit. A policy decision to test all PNW is requiring prolonged admission every week was made and implemented through communication via written circular and social media group. The overall percentage of positives over 6 months (1/7/20 at 01.01.21) in the green zone was 0.20% (3/1485) and in the holding zone, 20% (40/1810). Though in the second wave which began in the first week of April there was an increase in the percentage of positives in the holding zone no positive case has been identified in the green postnatal zone till the submission of this article.
Discussion
Universal COVID-19 testing, use of appropriate personal protective equipment, and isolation of patients according to their COVID-19 status are all recommended strategies to cope with the COVID-19 pandemic in healthcare facilities [6,7]. However, all these strategies were not enough to prevent the admission of asymptomatic non-suspect COVID-19 positive women in the green postnatal wards in our facility. The creation of a holding zone was the most effective strategy in preventing the transfer of asymptomatic COVID-19 positive PNW to the green zone. This was a costeffective method as it required lesser resources in terms of PPEs and workforce than expanding the orange zone. However, the smooth functioning of the postnatal wards after its creation was a challenge that was tackled in a systematic matter using PDSA cycles. We observed that there was a decrease in the percentage of COVID-19 positive in the holding zone from baseline data. We managed to keep our green zone almost free of COVID-19 positive PNW after multiple efforts and a few failures. The present study shows that the segregation of known COVID-19 negative PNW from potential asymptomatic COVID-19 positive among COVID non-suspect PNW awaiting reports is possible in a busy facility. This isolation is imperative in control of the spread of infection as shown in the study by Wong, et al. [11]. This was achieved by the creation of a holding zone within the non-suspect postnatal wards which led to early separation of possible positive asymptomatic cases from true negatives. The most challenging in achieving we aimed to maintain bed availability all the time. An essential element in achieving this was effective communication via social media groups regarding bed occupancy daily and the creation of buffer rooms within the same zones to accommodate the spill over from one of the zones which were fully occupied to the other in designated rooms through multiple PDSA cycles. This led to timely discharges of the PNW, ensured minimal hospital stay of non-suspects PNW, and availability of beds despite the increase in the number of deliveries. We were able to maintain the 100% transfer of COVID-19 negative PNW in the green zone.
Strengths
The strength of this project was that it only involved the re-organization of existing infrastructure without incurring extra cost and workforce. There was effective communication between the team members daily, which strengthened the bond between them as well helped in identifying the gaps timely. The creation of a 100% COVID-19 negative green zone is possible in busy and resource constraint facilities. This will improve the quality-of-care delivery by relocating more workforce and resources in holding COVID-19 suspects and COVID-19 positive zones. The attitude of adopting a systematic problem-solving approach to achieve the desired results despite constraints in resources can be imbibed and emulated by most of the facilities in developing countries.
Limitations
The limitation of the study was that social interaction of the PNW with other women as well as the visitors could not be restricted as it is human nature to be socially active despite following COVID-19 appropriate behaviour [11,12]. Another limitation is that the change ideas suggested in the study may not apply to all the facilities worldwide due to differences in the infrastructure and layout plan.
Conclusion
Using QI methodology, the project team was able to achieve near 100% transfer of COVID-19 negative PNW in the green zone. The authors suggest that similar holding zones can be created across all the health facilities so that nonsuspect COVID-19 positive PNW can be isolated early, thereby preventing the horizontal spread of the virus. This simple and cost-effective measure is achievable, sustainable, and is the most valuable tool in halting the pandemic.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Hellewell, Joel, et al. "Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts." The Lancet Global Health, Vol. 8, No. 4, 2020, pp. e488-96.
- "Clinical Management Protocol: COVID‐19." Government of India Ministry of Health and Family Welfare Directorate General of Health Services (EMR Division), 2020.
- Zhu, Na, et al. "A novel coronavirus from patients with pneumonia in China, 2019." New England Journal of Medicine, Vol. 382, 2020, pp. 727-33.
- Adhikari, Sasmita Poudel, et al. "Epidemiology, causes, clinical manifestation and diagnosis, prevention and control of Coronavirus Disease (COVID-19) during the early outbreak period: A scoping review." Infectious Diseases of Poverty, Vol. 9, No. 1, 2020, pp. 1-12.
- Verbeek, Jos H., et al. "Personal protective equipment for preventing highly infectious diseases due to exposure to contaminated body fluids in healthcare staff." Cochrane Database of Systematic Reviews, Vol. 4, 2020.
- World Health Organisation. "Public health and social measures for COVID-19 preparedness and response in low capacity and humanitarian settings." 2020. who.int/publications/m/item/public-health-and-social-measures-for-covid-19-preparedness-and-response-in-low-capacity-and-humanitarian-settings
- "Novel Coronavirus Disease 2019 (COVID-19): Guidelines on rational use of Personal Protective Equipment." Government of India Ministry of Health and Family Welfare Directorate General of Health Services (EMR Division), 2020. mohfw.gov.in/pdf/GuidelinesonrationaluseofPersonalProtectiveEquipment.pdf
- Sayampanathan, Andrew A., et al. "Infectivity of asymptomatic versus symptomatic COVID-19." The Lancet, Vol. 397, No. 10269, 2021, pp. 93-94.
- Cooke, Molly, Pamela M. Ironside, and Gregory S. Ogrinc. "Mainstreaming quality and safety: A reformulation of quality and safety education for health professions students." BMJ Quality & Safety, Vol. 20, No. Suppl 1, 2011, pp. 79-82.
- Taylor, Michael J., et al. "Systematic review of the application of the plan-do-study-act method to improve quality in healthcare." BMJ Quality & Safety, Vol. 23, No. 4, 2014, pp. 290-98.
- Wong, Shuk-Ching, et al. "Infection control challenges in setting up community isolation and treatment facilities for patients with coronavirus disease 2019 (COVID-19): Implementation of directly observed environmental disinfection." Infection Control & Hospital Epidemiology, Vol. 42, No. 9, 2020, pp. 1037-45.
- Kucharski, Adam J., et al. "Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-CoV-2 in different settings: A mathematical modelling study." The Lancet Infectious Diseases, Vol. 20, No. 10, 2020, pp. 1151-60.