Research - International Journal of Medical Research & Health Sciences ( 2020) Volume 9, Issue 11
Public Awareness of Hepatocellular Carcinoma and its Risk Factors Among General Population in Southern Region, Saudi Arabia, Cross Sectional Study
Abdullah Mohammed Albishi1*, Abdulaziz Alshahrani2, Ali Mohammed Alshahrani3, Dhafer Mohammed Alahmari4, Hussain Mesfer Alqibti4, Mohammed Ahmed Alsharif4, Saeed Mohammed Alshahrani4, Mohammed Saeed Alqahtani4 and Ibrahim Ayed Saad Alqahtani42Department of Medicine, Najran University, Najran, Saudi Arabia
3Armed Forces Medical Services General Directorate, Riyadh, Saudi Arabia
4King Khalid University, Abha, Saudi Arabia
Abdullah Mohammed Albishi, Armed Forces Hospital, Khamis Mushayt, Saudi Arabia, Email: dr.abdullah6975@gmail.com
Received: 21-Oct-2020 Accepted Date: Nov 23, 2020 ; Published: 30-Nov-2020
Abstract
Background: Globally, Hepatocellular carcinoma (HCC) is the third leading cause of cancer related mortality. There are many reported causes of HCC including chronic hepatitis B virus (HBV), hepatitis C virus (HCV) infection, primary autoimmune hepatitis, hemochromatosis, Budd-Chiari syndrome, and chronic alcohol consumption, which mostly result in liver cirrhosis. Fibrosis and cirrhosis are typically antecedents of HCC. Lack of population awareness may be by itself risk factors for disease and its sequalae. Aim: To assess the general population awareness regarding hepatocellular carcinoma and its risk factors in Southern region, southern of Saudi Arabia. Methodology: A descriptive cross-sectional survey was used targeting all population in Southern region, Saudi Arabia. The study was conducted during the period from February 2020 to May 2020. Data were collected using structured questionnaire included person’s socio-demographic data, Participants’ awareness regarding HCC. The questionnaire was uploaded online using social media platforms. Results: The study included a total of 956 participants whose ages ranged from 18 to 65 years old with mean age of 31.5 ± 8.6 years old. Exact of 149 (15.6%) participants had positive family history of liver cancer and 157 (16.4%) had family history of liver cirrhosis. Exact of 78.7% of the respondents reported that they know about liver cancer and 75.2% know about liver cirrhosis. In total, good awareness level regarding liver cirrhosis and cancer was low. Conclusions and recommendations: The study revealed that public awareness regarding HCC and its risk factors were low especially for signs and symptoms which are the early alarming noise for having liver disorder. Health care staff was not the main source of knowledge regarding HCC and liver cirrhosis.
Keywords
Hepatocellular carcinoma, Liver, cancer, Malignancy, Awareness, Population, Cirrhosis, Fibrosis
Background
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer with high incidence and mortality rate worldwide [1]. Globally, Hepatocellular carcinoma (HCC) is the third leading cause of cancer related mortality [2]. There are many reported causes of HCC including chronic Hepatitis B virus (HBV), Hepatitis C virus (HCV) infection, primary autoimmune hepatitis, hemochromatosis, Budd-Chiari syndrome, and chronic alcohol consumption, which mostly result in liver cirrhosis [3]. Fibrosis and cirrhosis are typically antecedents of HCC [4].
DM Considered as a significant risk factor with an approximately two-fold increase in the risk of developing HCC in comparison with non-diabetic individuals [5]. One of the causes to increase hepatocellular carcinoma is non-alcoholic fatty liver disease [6].
In Saudi Arabia, HCC represents 4.3% of all diagnosed cancers diagnosed in 2012 [7]. The incidence of liver cancer in Saudi Arabia recorded an increased incidence between 1990 and 2016 by about 3-folds [8]. Regarding treatment, liver transplantation is the only definitive treatment up till now. Resection of the tumour and other percutaneous therapies are more commonly used in practice, because most hepatocellular cancers are detected at an advanced stage and the prognosis is dependent on both the underlying liver function and the stage at which the tumour is diagnosed [9]. Liver transplant is contraindicated in case of Extrahepatic cancer or large sized HCC [10]. HCC is highly refractory to therapeutic interventions. Even after surgical resection or ablation, 70% of patients experience tumour recurrence within five years [11]. The prognosis of hepatocellular cancer depends on tumour stage and liver function [12].
Most people don’t show symptoms in the early stages of HCC. However, when signs and symptoms do appear, they might be related to cancer or to chronic liver disease [13].
Population awareness regarding HCC and its risk factors can help in early detection of suspected cases lowering the advance of the disease and its complications. The current study aimed to assess public awareness regarding liver cancer and its risk factors in Southern region, Saudi Arabia.
Methodology
A descriptive cross-sectional survey was used targeting all population in Southern region. The study was conducted during the period from February 2020 to May 2020. Data were collected using structured questionnaire which developed by the researchers after intensive literature review and expert’s consultation. The questionnaire data included person’s socio-demographic data such as age, gender, and education. Participants’ awareness regarding liver cirrhosis and cancer was assessed covering general awareness, signs and symptoms, risk factors, preventive and treatment methods, and precautions to avoid developing liver cancer. A panel of 3 experts reviewed the questionnaire independently for content validity and all suggested modifications were applied till the final tool achieved. The questionnaire was uploaded online using social media platforms by the researchers and their relatives and friends to be filled with all population in Southern region. A pilot study was conducted to assess tool applicability and reliability. The tool reliability coefficient (Alpha Cronbach’s) was assessed and equalled 0.86.
Data Analysis
After data were extracted, it was revised, coded and fed to statistical software IBM SPSS version 22 (SPSS, Inc. Chicago, IL). All statistical analysis was done using two tailed tests. P value less than 0.05 was considered to be statistically significant. For awareness items, each correct answer was scored one point and total summation of the discrete scores of the different items was calculated. A patient with score less than 60% (26 points) of the maximum score was considered to have poor awareness while good awareness was considered if he had score of 60% (27 points or more) of the maximum or more. Descriptive analysis based on frequency and percentage distribution was done for all variables including demographic data, awareness items and source of information. Cross tabluation was used to assess distribution of awareness according to participants’ personal data and source of information. Relations were tested using Pearson chi-square test.
Results
The study included a total of 956 participants whose ages ranged from 18 to 65 years old with mean age of 31.5 ± 8.6 years old. Majority of the participants were males (73.2%; 700) and were university graduated (71.4%; 683). Exact of 149 (15.6%) participants had positive family history of liver cancer and 157 (16.4%) had family history of liver cirrhosis. About 89.1% of the participants reported that they want to know more about liver cirrhosis and cancer (Table 1).
| Personal data | No. | Percentage (%) |
|---|---|---|
| Gender | ||
| Male | 700 | 73.20% |
| Female | 256 | 26.80% |
| Age in years | ||
| <20 years | 42 | 4.40% |
| 20-39 | 633 | 66.20% |
| 40-60 | 267 | 27.90% |
| >60 years | 14 | 1.50% |
| Level of education | ||
| Primary | 17 | 1.80% |
| Intermediate | 28 | 2.90% |
| Secondary | 228 | 23.80% |
| University | 683 | 71.40% |
| Had family history of liver cancer | ||
| Yes | 149 | 15.60% |
| No | 807 | 84.40% |
| Had family history of liver cirrhosis | ||
| Yes | 157 | 16.40% |
| No | 799 | 83.60% |
| Want to know more about liver cirrhosis and cancer | ||
| Yes | 852 | 89.10% |
| No | 104 | 10.90% |
Table 1: Personal data of study participants in Southern region, Saudi Arabia
Table 2 illustrates General population awareness regarding liver cirrhosis and cancer. Exact of 78.7% of the respondents reported that they know about liver cancer and 75.2% know about liver cirrhosis. Regarding causes of liver cancer and cirrhosis, 74.6% of the participants agreed on that drinking alcohol may increase your incidence of liver cancer by causing cirrhosis followed by Unsafe injection practices and unsafe blood transfusions can lead to hepatitis B and C transmission to healthy individuals (73.7%), Cirrhosis is one of the most important causes of liver cancer (66.1%), Sharing shavers, toothbrushes, etc. with Hepatitis B patients can spread the disease to healthy people (66.1%), and Hepatitis B (C) infection can lead to cirrhosis and then liver cancer (59.4%). Considering protective and treatment methods for liver cirrhosis and cancer, 86.2% of the respondents reported that Exercise is important to get rid of fatty deposits on the liver and then reduce the risk of cirrhosis and liver cancer later followed by quitting alcohol helps prevent cirrhosis and then liver cancer (83.2%), It is strictly prohibited to share shavers, toothbrushes, etc. with other individuals (83.1%), Eating healthy, fresh meals with fresh fruits and vegetables will prevent cirrhosis and liver cancer later on. (76.4%), and if there is a family history of liver cancer, then the other family members should see the doctor (73.1%).
| Domain | Items | No. | Percentage (%) |
|---|---|---|---|
| General awareness | Know about cancer liver | 752 | 78.70% |
| Know about liver cirrhosis and its causes | 719 | 75.20% | |
| Hepatitis B (C) infection can lead to cirrhosis and then liver cancer | 568 | 59.40% | |
| Causes of liver cirrhosis and cancer |
Cirrhosis is one of the most important causes of liver cancer | 632 | 66.10% |
| Non-alcoholic fatty liver disease (fatty acid deposition in the liver) is a cause of cirrhosis and hence later liver cancer | 422 | 44.10% | |
| Diabetes is one of the causes of cirrhosis and liver cancer | 259 | 27.10% | |
| Cirrhosis and liver cancer can be linked to obesity | 391 | 40.90% | |
| Drinking alcohol may increase your incidence of liver cancer by causing cirrhosis | 713 | 74.60% | |
| Smoking is not associated with an increased risk of liver cancer | 126 | 13.20% | |
| Patients with high blood pressure are at risk of developing cirrhosis and should see their doctors to control blood pressure | 348 | 36.40% | |
| Family history of liver cancer is not considered a factor in the future of liver cancer | 131 | 13.70% | |
| There is no vaccine against hepatitis C virus | 242 | 25.30% | |
| Unsafe injection practices and unsafe blood transfusions can lead to hepatitis B and C transmission to healthy individuals | 705 | 73.70% | |
| Epidemic hepatitis B can be transmitted from the mother to her child, and she must inform the gynaecologist of her HBV infection on the first visit of pregnancy | 532 | 55.60% | |
| Sharing shavers, toothbrushes, etc. with Hepatitis B patients can spread the disease to healthy people | 631 | 66.10% | |
| If there is a family history of liver cancer, then the other family members should see the doctor | 699 | 73.10% | |
| Protective and treatment measures | No need to quit smoking in order to prevent cirrhosis and then liver cancer | 73 | 7.60% |
| Quitting alcohol helps prevent cirrhosis and then liver cancer | 795 | 83.20% | |
| Eating healthy, fresh meals with fresh fruits and vegetables will prevent cirrhosis and liver cancer later on | 730 | 76.40% | |
| Exercise is important to get rid of fatty deposits on the liver and then reduce the risk of cirrhosis and liver cancer later | 824 | 86.20% | |
| It is strictly prohibited to share shavers, toothbrushes, etc. with other individuals | 794 | 83.10% | |
| Control of diabetes and high blood pressure can prevent cirrhosis and later liver cancer | 616 | 64.40% | |
| The hepatitis B virus vaccine is important for people at risk of infection (such as doctors and the family of a patient with HIV) | 625 | 65.40% | |
| The hepatitis B virus vaccine is available for newborn | 478 | 50.00% | |
| Hepatitis B can be transmitted through the marital relationship, so the healthy partner should receive the hepatitis B vaccine | 417 | 43.60% | |
| Most patients at risk of developing liver cancer, such as patients with cirrhosis or who have a family history of liver cancer, should have an ultrasound examination of the liver every 6 months | 520 | 54.40% | |
| There is no treatment for liver cancer yet | 258 | 27.00% | |
| Liver transplant is the first option for treating liver cancer if the disease is detected early and the patient meets the criteria for transplantation | 591 | 61.80% |
Table 2: General population awareness regarding liver cirrhosis and cancer in Southern region, Saudi Arabia
Table 3 illustrates continued population awareness level. As for signs and symptoms, jaundice was the most reported by the participants (16.3%; 156) followed by loss of appetite with nausea (13.9%; 133), hematemesis (10.7%; 102), weight loss (9.9%; 95), and malaise (7%; 67). Considering required precaution to minimize having liver cirrhosis and cancer, stopping smoking and alcohol intake was the most reported by the participants (65.9%; 630), followed by having HBV vaccine (65.4%; 625), practice exercise and weight loss (64.1%; 613), periodic check-up for viral hepatitis (64%; 612), Periodic abdominal ultrasound for patient with positive family history of HCC (56%; 535), and control of diabetes and hypertension (55.3%; 529). In total, good awareness level regarding liver cirrhosis and cancer was recorded among 336 participants (35.1%).
| Domain | Items | No. | Percentage (%) |
|---|---|---|---|
| Sign and symptoms of liver cirrohsis | Mostly no signs and symptoms | 649 | 67.60% |
| Jaundice | 156 | 16.30% | |
| Loss of appetite with nausea | 133 | 13.90% | |
| Hematemesis | 102 | 10.70% | |
| Weight loss | 95 | 9.90% | |
| Malaise | 67 | 7.00% | |
| Abdominal pain | 60 | 6.30% | |
| Abdominal distention | 14 | 1.50% | |
| Ascites | 1 | 0.10% | |
| Abdominal mass | 1 | 0.10% | |
| Precautions to cirrohsis and liver cancer | Stop smoking and alcohol intake | 630 | 65.90% |
| Have HBV vaccine | 625 | 65.4% | |
| Weight loss and practice exercise | 613 | 64.10% | |
| Periodic check-up for viral hepatitis | 612 | 64.00% | |
| Periodic U/S for patient with positive family history | 535 | 56.0% | |
| Control of DM and HTN | 529 | 55.30% | |
| Proper treatment of viral hepatitis | 503 | 52.60% | |
| Follow-up with hepatology specialist | 496 | 51.90% | |
| Overall awareness level | Poor (0-26) | 620 | 64.90% |
| Good (27-42) | 336 | 35.10% |
Table 3: General population awareness regarding liver cirrhosis and cancer
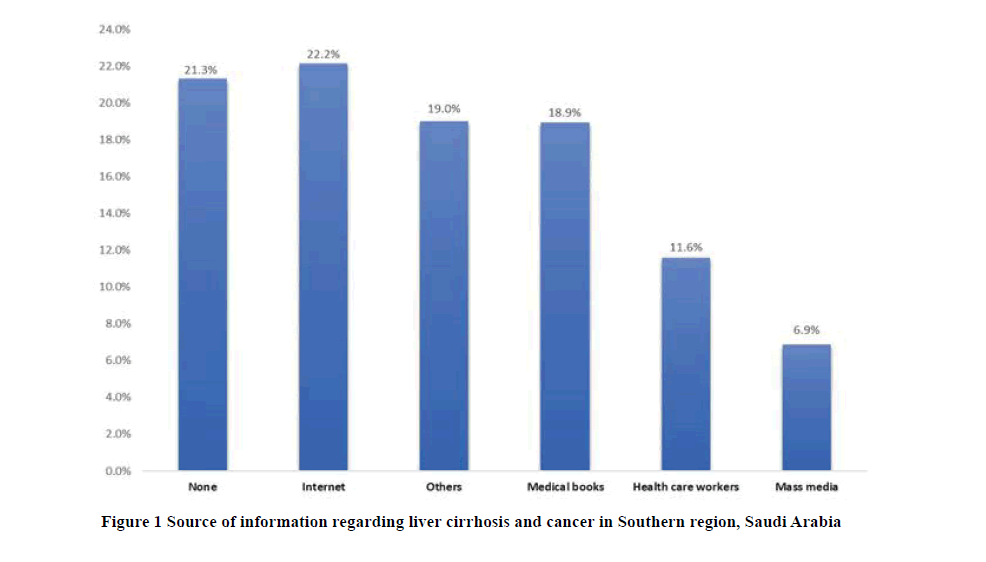
About source of information, Figure 1 demonstrates that the most reported source was internet and social media (22.2%) followed by medical books (18.9%), health care workers (11.6%), and mass media (6.9%). Exact of 21.3% of the participants had no source regarding their information.
Table 4 shows distribution of participant’s awareness level regarding liver cancer by their personal data. Good awareness level was recorded for 50% of old age participants (>60 years) compared to 16.7% of those who aged below 20 years with recorded statically significance (p=0.009). Also, 39.8% of university graduated participants had good awareness level compared to 23.5% of primary educated respondents (p=0.001). Exact of 63.5% of participants who had their information from health care staff had good awareness level compared to 8.3% of those who had no specific source for their information (p=0.001).
| Personal data | Awareness level | p-value | ||||
|---|---|---|---|---|---|---|
| Poor | Good | |||||
| No. | Percentage (%) | No. | Percentage (%) | |||
| Gender | Male | 462 | 66.00% | 238 | 34.00% | 0.22 |
| Female | 158 | 61.70% | 98 | 38.30% | ||
| <20 years | 35 | 83.30% | 7 | 16.70% | ||
| 20-39 | 394 | 62.20% | 239 | 37.80% | ||
| Age in years | 40-60 | 184 | 68.90% | 83 | 31.10% | 0.009* |
| >60 years | 7 | 50.00% | 7 | 50.00% | ||
| Primary | 13 | 76.50% | 4 | 23.50% | ||
| Intermediate | 18 | 64.30% | 10 | 35.70% | ||
| Level of education | Secondary | 178 | 78.10% | 50 | 21.90% | 0.001* |
| University | 411 | 60.20% | 272 | 39.80% | ||
| Had family history of liver cancer | Yes | 101 | 67.80% | 48 | 32.20% | 0.42 |
| No | 519 | 64.30% | 288 | 35.70% | ||
| Had family history of liver cirrhosis | Yes | 99 | 63.10% | 58 | 36.90% | 0.61 |
| No | 521 | 65.20% | 278 | 34.80% | ||
| Want to know more about liver cirrhosis and cancer | Yes | 544 | 63.80% | 308 | 36.20% | 0.06 |
| No | 76 | 73.10% | 28 | 26.90% | ||
| None | 187 | 91.70% | 17 | 8.30% | ||
| Internet | 137 | 64.60% | 75 | 35.40% | ||
| Mass media | 47 | 71.20% | 19 | 28.80% | ||
| Source of information | Health care workers | 53 | 47.70% | 58 | 52.30% | 0.001* |
| Medical books | 66 | 36.50% | 115 | 63.50% | ||
| Others | 130 | 71.40% | 52 | 28.60% | ||
P: Pearson X2 test; *p<0.05 (significant)
Table 4: Distribution of participants awareness level regarding liver cancer by their personal data
Discussion
The current study target was to assess the awareness of general population for HCC and its risk factors, some of these risk factors can be preventable. Hepatitis B vaccines and lifestyle modification is important to decrease the exposure of primary liver cancer [14]. Periodic Ultrasound screening of liver every 6 months should be done for patients with high likelihood to have Hepatocellular carcinoma (HCC) like cirrhotic patient or family history of HCC or Hepatitis B [15]. The American Association for the Study of Liver Diseases (AASLD) recommends surveillance of adults with cirrhosis because it improves overall survival [16].
The current study revealed that family history of liver cirrhosis and HCC among study participants was not high (less than one quarter). Regarding public awareness, nearly one out of each three participants were aware regarding HCC (One third had good awareness). In more details, generally, more than three quarters of the study population heard about liver cirrhosis and HCC. As for causes of HCC, drinking alcohol, unsafe blood transfusion and injections, and sharing instruments with cirrhosis were the most reported causes by the participants. Regarding protective and treatment methods, more than 80% of the participants reported for getting rid of body fats through exercise and activity. Also, stop alcohol intake, avoid sharing instruments with others will minimize getting infectious hepatitis and liver cirrhosis which are the main predisposing factors for HCC. Periodic check-up for those with positive family history of cancers in general and liver cancer in private was also recommended by nearly three quarters of the respondents. Nearly two thirds of the participants reported liver transplantation as the most appropriate treatment method in cases of early detection of HCC. Considering signs and symptoms, the surprising finding was that about two thirds of the participants reported that mostly HCC and liver cirrhosis had no signs or symptoms which are an important conclusion and recommendation for health care providers. Lack of awareness regarding signs and symptoms will be the main barrier against early detection of cases causing advanced stages diagnosis with irreversible changes. Jaundice, loss of appetite, hematemesis was the most recorded signs and symptoms among those who know. Only one participant told about abdominal mass with pain. The study also revealed that stopping smoking and alcohol intake with periodic check-up for viral hepatitis with receiving the proper management will prevent developing HCC.
As for source of information, internet was the most reported source followed by medical books, and health care providers but about 20% had no specific source mentioned. The most significant predictors for awareness level were old age (p=0.009), higher education (p=0.001), and health care staff as a source of knowledge with medical books (p=0.001).
Public Awareness of the Link between Alcohol and Cancer in England was studied by Buykx, et al. [17]. The study revealed that the awareness of general population in England about the relation between hepatic cancer and alcohol consumption was low. He, et al. [18], assessed inpatients’ knowledge about primary liver cancer and hepatitis. The study revealed that The mean knowledge scores were: 6.47 ± 3.03 (maximum possible score=14) for risk factors of HCC and HBV, 5.21 ± 3.38 (maximum possible score=11) for symptoms and signs of HCC, 5.21 ± 3.38 (maximum possible score=11) for preventive strategies of HCC, 1.73 ± 1.25 ( maximum possible score=5) for management of liver cancer, 2.68 ± 1.25 (maximum possible score=5) for transmission mode of hepatitis B, and 3.70 ± 1.41 (maximum possible score=5) for prevention of hepatitis. Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco BayArea, California were assessed by Charlotte, et al. [19]. The researcher reported that knowledge regarding HBV transmission, prevention, symptoms, risks, and occurrence was low. Fewer than 60% reported having been tested for HBV, only 31% reported having been vaccinated against HBV, and only 44% reported having had their children vaccinated. Asians, especially those born in China or Southeast Asia, had significantly poorer knowledge regarding HBV and liver cancer than non-Asians. In Saudi Arabia, Alshammari, et al. [20], conducted a cross-sectional study was conducted in North Saudi Arabia (Hail Region). Data was collected as a part of a community-based cancer’s awareness movement that covered an area inhibited with approximately 500,000 individuals. In conclusion, the study revealed that about 79.3% and 80.7% believed that tobacco smoking and smokeless are not a risk of cancer development. Also, (87.2% of the study population believe that exposure to diverse occupational or non-occupational chemicals has no role in cancer development. Furthermore, about 59% of the study participants believed that repeated exposure to insecticidal chemicals does not influence the risk of cancer [20].
Conclusion and Recommendations
The study revealed that public awareness regarding liver cirrhosis and HCC were low especially for signs and symptoms which are the early alarming noise for having liver disorder. Health care staff were not the main source of knowledge regarding HCC and liver cirrhosis. There is an urgent need for awareness educational programs and preventive measures towards lifestyle modification that can modulate the overall risk of cancer among Saudi population. Widening viral hepatitis screening and liver cancer prevention programs among all public health programs is a vital step in decreasing liver cancer rates in the Saudi population.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Adams, Leon A., et al. "The natural history of nonalcoholic fatty liver disease: A population-based cohort study." Gastroenterology, Vol. 129, No. 1, 2005, pp. 113-21.
- Ferlay, Jacques, et al. "Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012." International Journal of Cancer, Vol. 136, No. 5, 2015, pp. E359-86.
- Parkin, D. Maxwell, et al. "Estimating the world cancer burden: Globocan 2000." International Journal of Cancer, Vol. 94, No. 2, 2001, pp. 153-6.
- Fuchs, Bryan C., et al. "Epidermal growth factor receptor inhibition attenuates liver fibrosis and development of hepatocellular carcinoma." Hepatology, Vol. 59, No. 4, 2014, pp. 1577-90.
- Zheng, Ze, et al. "Diabetes mellitus is associated with hepatocellular carcinoma: A retrospective case-control study in hepatitis endemic area." PloS one, Vol. 8, No. 12, 2013, p. e84776.
- Piñero, Federico, et al. "A changing etiologic scenario in liver transplantation for hepatocellular carcinoma in a multicenter cohort study from Latin America." Clinics and Research in Hepatology and Gastroenterology, Vol. 42, No. 5, 2018, pp. 443-52.
- Bazarbashi, Shouki, Haya Al Eid, and Joan Minguet. "Cancer incidence in Saudi Arabia: 2012 data from the Saudi cancer registry." Asian Pacific Journal of Cancer Prevention: APJCP, Vol. 18, No. 9, 2017, p. 2437.
- Althubiti, Mohammad A., and Mohamed M. Nour Eldein. "Trends in the incidence and mortality of cancer in Saudi Arabia." Saudi Medical Journal, Vol. 39, No. 12, 2018, p. 1259.
- Parikh, Sameer, and David Hyman. "Hepatocellular cancer: A guide for the internist." The American Journal of Medicine, Vol. 120, No. 3, 2007, pp. 194-202.
- Serrano, Oscar K., et al. "Clinical significance of pulmonary nodules in the pretransplant evaluation of liver transplant recipients with hepatocellular carcinoma." Experimental and Clinical Transplantation: Official Journal of the Middle East Society for Organ Transplantation, Vol. 16, No. 3, 2018, pp. 314-20.
- Nakagawa, Shigeki, et al. "Molecular liver cancer prevention in cirrhosis by organ transcriptome analysis and lysophosphatidic acid pathway inhibition." Cancer Cell, Vol. 30, No. 6, 2016, pp. 879-90.
- Bruix, Jordi, et al. "Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: analysis of two phase III studies." Journal of Hepatology, Vol. 67, No. 5, 2017, pp. 999-1008.
- Munishi, Oresto Michael, et al. "Awareness of cancer risk factors and its signs and symptoms in Northern Tanzania: A cross-sectional survey in the general population and in people living with HIV." Journal of Cancer Education, Vol. 35, 2019, pp. 1-9.
- El‐Serag, Hashem B. "Epidemiology of hepatocellular carcinoma." The Liver: Biology and Pathobiology, Vol. 59, 2020, pp. 758-72.
- Miller, Zoe A., and Kyungmouk Steve Lee. "Screening for hepatocellular carcinoma in high-risk populations." Clinical Imaging, Vol. 40, No. 2, 2016, pp. 311-4.
- Heimbach, Julie K., et al. "AASLD guidelines for the treatment of hepatocellular carcinoma." Hepatology, Vol. 67, No. 1, 2018, pp. 358-80.
- Buykx, Penny, et al. "Public awareness of the link between alcohol and cancer in England in 2015: a population-based survey." BMC Public Health, Vol. 16, No. 1, 2016, p. 1194.
- He, Wen-Jing, et al. "Inpatients' knowledge about primary liver cancer and hepatitis." Asian Pacific Journal of Cancer Prevention, Vol. 14, No. 8, 2013, pp. 4913-8.
- Charlotte, A., et al. "Hepatitis B and liver cancer knowledge and preventive practices among Asian Americans in the San Francisco Bay Area, California." Asian Pacific Journal of Cancer Prevention, Vol. 8, 2007, pp. 127-34.
- Alshammari, Fawaz Dabea, et al. "Population insight of the relationship between lifestyle and cancer: A population-based survey." AIMS Public Health, Vol. 6, No. 1, 2019, p. 34.