Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 8
The Relationship between Breastfeeding and Autoimmune Diseases among Children in Makkah City
Amna Alotiby1*, Reem Bagadood2, Rawan Bazuhayr2, Lama Shabanah2, Nouf Qurbi2, Revan Mujahed2, Hana Halabi3 and Khariah Alsufyani42Faculty of Medicine, Umm Alqura University, Makkah, Saudi Arabia
3Department of Pediatric Gastroenterology, Maternity and Children Hospital, Makkah, Saudi Arabia
4Department of Pediatric Rheumatology, Maternity and Children Hospital, Makkah, Saudi Arabia
Amna Alotiby, Department of Hematology and Immunology, Faculty of Medicine, Umm Alqura University, Makkah, Saudi Arabia, Email: aamogaty@uqu.edu.sa
Received: 23-Jul-2021 Accepted Date: Aug 24, 2021 ; Published: 31-Aug-2021
Abstract
Background: Breast milk is an optimal nutrient source for, and mediates immune protection in, children. Further, it aids antibody production and shapes the mucosal immune response in children. Our study aimed to determine the relationship between breastfeeding and autoimmune diseases, particularly, Rheumatoid Arthritis (RA) and Inflammatory Bowel Disease (IBD). Methods: A cross-sectional study was performed at the Maternity and Children’s Hospital (MCH) in Makkah, Saudi Arabia (between February and August 2020). Data were collected through phone interviews; analysis was performed at 95% confidence intervals using the Statistical Package for the Social Sciences. Results: Of the 60 patients enrolled, 44 had RA and 16 had IBD; 31 of these 60 patients (51.7%) were female, and the rest were male. In terms of the feeding type, (28.3%) were breastfed, (21.7%) were formula-fed, and (50.0%) were mixed-fed. Compared with the IBD patients, a higher percentage of RA patients were formula-fed (92.3% vs. 7.7%) and mixed-fed (80% vs. 20%). In contrast, 52.9% and 47.1% of IBD and RA patients, respectively, were breastfed. This difference in the feeding type was statistically significant (p=0.011). Our results also indicated that the duration of breastfeeding (0-6, 6-24, and >24 months) was not associated with the incidence of RA or IBD (p=0.316). Conclusion: Formula feeding markedly increased the incidence of RA, but not IBD, in children. Hence, exclusive breastfeeding may reduce the risk of RA. Further studies across multiple medical centres in Saudi Arabia with large sample sizes are recommended.
Keywords
Breastfeeding, Inflammatory bowel disease, Ulcerative colitis, Crohn’s disease, Rheumatoid arthritis, Pediatric
Introduction
The immune system, which is designed to protect the body by attacking foreign antigens, is composed of collecting cells, tissues, and molecules that mediate resistance to infection. Once the immune system loses immunological tolerance, it attacks self-antigens, leading to the development of autoimmune diseases [1]. This usually happens in young populations with genetic susceptibility to such conditions, in combination with environmental factors [2].
Breastfeeding, which is the natural process of feeding infant breast milk to satisfy the child’s hunger, is considered a major factor influencing the development of a healthy immune system during the early stages of life; this process may affect a child’s susceptibility to diseases [3]. Apart from its nutritional value, breast milk provides many benefits to the infant. It contains antibodies (IgA) that help infants fight against viruses and bacteria. In addition, it plays a significant role in immunity development and the modulation of the infant’s intestinal microbiome [4]. Moreover, breast milk contains allergen-specific immunoglobulins, immune complexes, and immunosuppressive cytokines that are transferred through the milk and could modify the infant’s immune response to allergens and decrease susceptibility to immune-mediated disorders, such as asthma, celiac disease, and multiple sclerosis. Breastfeeding also plays a role in protecting the infant against chronic conditions, such as type 1 and type 2 diabetes, obesity, and hypertension [3].
Rheumatoid Arthritis (RA) is one of the most common autoimmune inflammatory disorders; it leads to persistent synovitis and rheumatoid factor formation [3]. It has been shown that 50% of the risk for the development of RA can be attributed to genetic and environmental factors, such as smoking [5]. Uncontrolled active RA causes joint damage, decreased quality of life, and other comorbidities. Furthermore, the results of a 2015 study, based on data acquired from clinical assessments and cross-sectional surveys, stated that the prevalence of RA in Saudi Arabia is similar to the estimated prevalence on a global scale [6]. Unfortunately, at present, there is a lack of studies to identify the most common autoimmune disease in Saudi Arabia among pediatric populations. However, the authors of the present study have observed that in recent years, there has been an increase in the number of orders placed by laboratory pediatric clinics in Makkah city for rheumatoid factor tests, along with a concomitant increase in the frequency of positive results.
Inflammatory Bowel Disease (IBD) represents a group of chronic inflammatory gastrointestinal tract diseases, including Ulcerative Colitis (UC) and Crohn’s Disease (CD). While UC affects the colonic mucosal layer, the CD can involve any component of the gastrointestinal tract and is characterized by transmural inflammation [7]. Although the etiology of IBD remains unknown, it has been found that multiple co-factors, including immunological, environmental, and genetic factors, such as the mutation of the NOD2 (Nucleotide-binding Oligomerization Domain-containing protein 2) gene and influence of the HLA-B27 (Human Leukocyte Antigen-B27) gene, play an essential role in the development of IBD. In addition, increased fat intake, previous intestinal infection, and nicotine consumption are risk factors for CD and protective factors for UC and host immunity dysregulation [8]. An article published in JAMA Pediatrics in 2015 showed that IBD most commonly occurs during adolescence and young adulthood [9]. The incidence of pediatric IBD in the United States and Canada is approximately 10 per 100,000 children; this number continues to rise [9].
If the risk of developing autoimmune diseases, such as RA and IBD, can be reduced, the complications associated with, and the side effects of, long-term therapies may be ameliorated [10,11]. In addition to the previously mentioned data regarding the importance of breastfeeding and how it helps develop the immune system, the global World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommend exclusive breastfeeding for the first six months of an infant’s life, as it is necessary to maintain an optimal healthy immune system [4,12-14]. While several studies have focused on breastfeeding, the mechanisms underlying the protective effects of breastfeeding against RA and IBD remain controversial. Therefore, this study aimed to evaluate the relationship between breastfeeding and the development of autoimmune diseases, including RA and IBD, in children at the Maternity and Children’s Hospital (MCH) in Makkah city, Saudi Arabia. In addition, we compared the onset of these diseases among breastfed and nonbreastfed children and children fed with both breast milk and formula (mixed-fed children).
Materials and Methods
Ethical Approval
This cross-sectional study was approved by the Research and Ethics Committee of the Ministry of Health (Approval No. H-02-K-076-0320-267) and by the Biomedical Ethics Committee, Faculty of Medicine, Umm Alqura University (Approval No. HAPO-02-K-012-2019-11-334). The study was conducted by the Declaration of Helsinki, and all participants provided informed consent before the start of data collection. This study was conducted between February 2020 and March 2020 at the MCH in Makkah City, Saudi Arabia. Although data collection was halted because of the COVID-19 pandemic, it was resumed from July 15 to August 15, 2020.
Study Participants
Participants were recruited from the MCH, the main hospital in Makkah, which included pediatric Gastrointestinal Tract (GIT) and rheumatology clinics; patients referred to these clinics were also considered for enrolment. A total of 39 patients diagnosed with IBD and 114 patients with RA were enrolled in the study. To answer the study questionnaire, the phone numbers of the patients’ parents were obtained from hospital files.
The required sample size for the study was determined using the OpenEpi software (version 3.0 26) [15]. However, when the number of hospital admissions of pediatric patients with RA and IBD was considered, we found out that to achieve a 95% confidence interval and a 5% margin of error, 89 participants with RA and 39 with IBD were needed. Only 58 patients with RA and 22 patients with IBD completed our questionnaire; the remaining subjects did not answer our questionnaire. Of these, 20 patients were excluded based on the study exclusion criteria. Therefore, the remaining 60 patients were included in this study.
The parents and/or guardians of all the participants were aware of all the study objectives; consent was obtained from the parents and/or guardians of all the participants of this study. The mothers were asked to fill out a questionnaire detailing their child’s history, gender, age at diagnosis, type, duration, and feeding frequency.
Statistical Analysis
Descriptive statistics were used to present categorical variables as frequencies and percentages. Numerical data are presented as the means ± standard deviations. Association between categorical variables, such as gender and autoimmune disease, type of feeding and autoimmune disease, risk of autoimmune disease, and frequency of breastfeeding were determined using the Chi-square test. Numerical data were checked for normality using the Shapiro-Wilk and Kolmogorov tests. Since all numerical data were non-normally distributed according to these tests, non-parametric tests were used to assess the relationship between the categorical and numerical data. The Mann- Whitney U test was used to assess the relationship between the risk of autoimmune disease and the duration of breastfeeding. The same test was used to assess the relationship between the mean age of the patients with RA and that of the patients with IBD. The Kruskal-Wallis test was used to compare the mean age at diagnosis for patients subjected to each type of feeding. The analysis was performed with a 95% confidence interval using the Statistical Package for Social Science (SPSS) (version 23.0; IBM, Armonk, NY, USA) software.
Results
This study included 60 subjects, of which 44 had Rheumatoid Arthritis (RA) and 16 had Inflammatory Bowel Disease (IBD). Among these 60 patients, 31 (51.7%) were women and 29 (%) were men. About the feeding type, 17 (28.3%) patients were breastfed, 13 (21.7%) were formula-fed, and 30 (50.0%) were mixed-fed; there were 17 (28.3%) patients who were breastfed for two years (Table 1).
| Characteristics | Attributes | N | % |
|---|---|---|---|
| Gender | Male | 29 | 48.3 |
| Female | 31 | 51.7 | |
| Age | 1-4 years old | 4 | 6.7 |
| 5-8 years old | 20 | 33.3 | |
| 9-12 years old | 19 | 31.7 | |
| 13-16 years old | 17 | 28.3 | |
| Disease | RA | 44 | 73.3 |
| IBD | 16 | 26.7 | |
| Type of feeding | Breastfeeding | 17 | 28.3 |
| Formula | 13 | 21.7 | |
| Mixed | 30 | 50.0 | |
| Two years of breastfeeding | Yes | 17 | 28.3 |
| No | 30 | 50.0 |
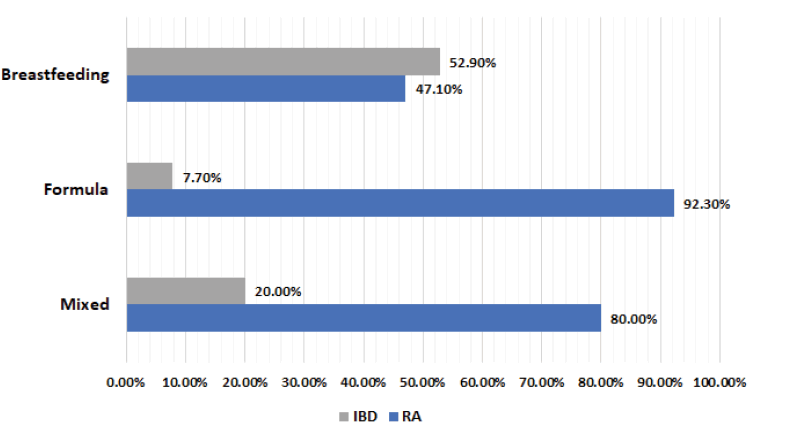
A higher percentage of patients with RA (than that of those with IBD) were formula-fed (92.3% vs. 7.7%) and mixedfed (80% vs. 20%). In contrast, 52.9% of patients with IBD and just 47.1% of patients with RA were breastfed (Figure 1). This difference in the type of feeding between the RA and IBD cases was statistically significant (p=0.011).
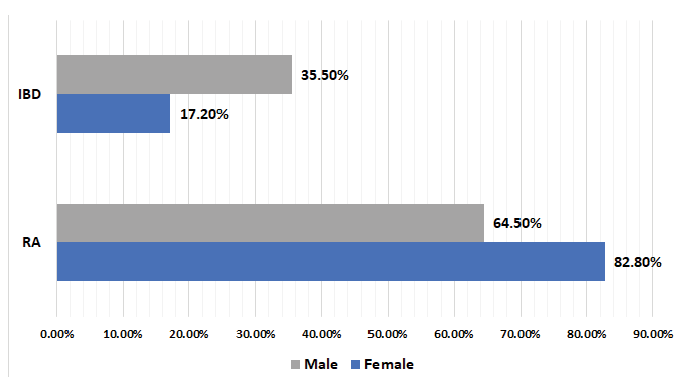
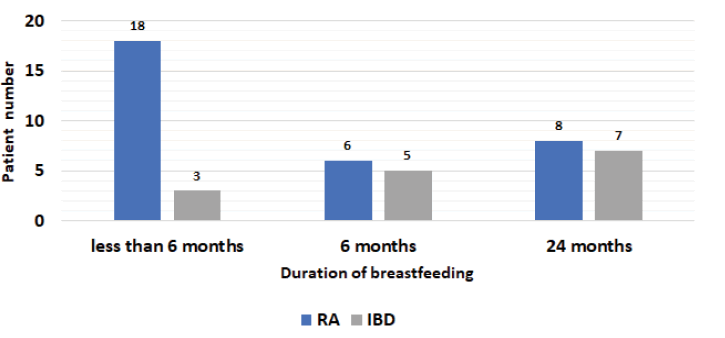
The relationships between gender and autoimmune disease (p=0.110) (Figure 2) were assessed and found to be not statistically significant. Moreover, the duration of breastfeeding (0-6, 6-24, and >24 months) was not associated with any particular autoimmune disease (RA or IBD; p=0.316) (Figure 3).
Discussion
The World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommend exclusive breastfeeding for the first six months after childbirth; then, other complementary foods can be introduced with continued breastfeeding for up to two years or at least for one year [12,14,16]. It has been reported that breastfeeding can reduce the pediatric mortality rate from 13% to 11.6% by improving child survival and protecting them against life-threatening and chronic illnesses, especially during the critical window from birth to the age of 2 years [17]. Breastfeeding also supports brain development and results in high performance in intelligence tests [14,16,17]. However, breastfeeding does not benefit only the infants; it also benefits the mother [16]. It protects the mother against postpartum haemorrhage, postpartum depression, ovarian and breast cancer, heart disease, and type 2 diabetes [14,16,17]. Unfortunately, according to UNICEF, globally, only two in five infants aged 0-5 months are exclusively breastfed. In the Middle East, the prevalence of exclusive breastfeeding is approximately 30%, with minimal improvement [16]. Additionally, a study conducted in Riyadh and Dammam, Saudi Arabia, in 2018 reported that the prevalence of breastfeeding practices in the study population is 76% at birth. However, it decreases to 37% after 6 months [18]. Consequently, in 2014, the global WHO and UNICEF recommended increasing the exclusive breastfeeding rate to 50% by 2025 [14,16,17]. Therefore, the current study aimed to clarify the role of breastfeeding in reducing the incidence and development of two autoimmune diseases, IBD and RA, and compare the onset of these diseases between breastfed, non-breastfed, and mixed-fed children in Makkah, Saudi Arabia.
Concerning the type of feeding and the risk of RA, the current study found that among RA patients, the percentages of formula-fed (92.3%) and mixed-fed (80%) patients were higher than the percentage of patients who were exclusively breastfed (49.10%). This indicates that formula feeding may increase the incidence of RA in children; hence, exclusive breastfeeding may reduce the risk of RA. This finding is in agreement with a previous study that demonstrated that exclusive breastfeeding reduces the risk of RA in children [19]. Additionally, a similar result was reported by Kindgren in 2017; these authors found that early introduction of formula milk (<4 months of age) is associated with an increased risk of Juvenile Idiopathic Arthritis (JIA) [20]. In contrast, a meta-analysis of RA patients, in which six studies were included, showed a relationship between breastfeeding and a reduced risk of RA in white people, regardless of whether the breastfeeding time was longer or shorter than 12 months [19]. However, the authors of this meta-analysis suggested that more studies on Asian and African populations are needed to validate these findings, because of the genetic differences among various populations; thus, the findings of this meta-analysis cannot be considered accurate because of such genetic differences and the bias associated with study selection, given that only studies published in English were selected [19].
Herein, we found no statistically significant relationship between breastfeeding and IBD development, as 52.1% of the IBD patients were exclusively breastfed. This is in contrast with previous studies that have demonstrated that breastfeeding is a protective factor against IBD development [7]. Likewise, a systematic review reported the same findings, but these data may have been associated with a selection bias and are insufficient to address the primary idea [21]. Of note, like our study, other studies found no significant relationship between breastfeeding and protection against IBD [3].
A study conducted in April 2017 by Strisciuglio and her co-authors showed that the short- and long-term benefits of breastfeeding override the increased risk of IBD [22]. In comparison, in November 2017, a systemic review with meta-analysis, which included 14 studies, concluded that increasing the duration of breastfeeding is associated with a more notable reduction in the risk of both CD and UC [7]. Likewise, per a systematic review conducted in 2019, limited case-control evidence suggests that feeding human milk for short durations or not feeding children with breast milk at all is associated with a higher risk of diagnosed IBD and celiac disease [23]. Additionally, Francisco Rocha (2019) reported a similar result regarding JIA: breastfeeding for more than 6 months tended to lower disease activity. The shorter the duration of exclusive breastfeeding, the greater was the risk of JIA [24].
Conclusion
In conclusion, the results of the current showed that breastfeeding may reduce the risk of RA, whereas no significant relationship between breastfeeding and IBD risk reduction was found. These findings are critical and interesting, but further data are required to validate these outcomes. The main limitation of this study was the small sample size. Consequently, to confirm the relationship between breastfeeding and the development of RA and IBD in children, determine the association between the duration of breastfeeding and the development of the disease, and identify the prevalence of RA and IBD in the Makkah region by involving all pediatric clinics, we recommend that more studies across multiple pediatric centres in the Makkah city be performed, with larger sample sizes.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
Authors’ Contributions
Qurbi, N. and Bagadood, R. contributed to the conception and design of the study. Bazuhayr, R., Shabanah, L., and Mujahed, R. contributed to the acquisition, analysis, and interpretation of the data. All authors participated in drafting the article and the critical revision of this article for important intellectual content. Alotiby, A. contributed to the design and implementation of the research, revised the study’s design, performed the data analysis and interpretation, and drafted this manuscript. Halabi, H, and Alsufyani, K contributed to the data collection. All authors have approved the final version of the manuscript.
Acknowledgements
The authors would like to express their sincere appreciation to the head of the Education and Training Center at the Maternity and Children’s Hospital, Dr. Mohammed Salim AL-Khayat, for his invaluable assistance, support, and help in obtaining institutional approval to gain access to the hospital database. We express our heartfelt gratitude to the parents of all the participants of this study for making this research study possible.
Funding
The authors declare that no funding was received for this research
References
- Smith, Dorinda A., and Dori R. Germolec. "Introduction to immunology and autoimmunity." Environmental Health Perspectives, Vol. 107, No. suppl 5, 1999, pp. 661-65.
- Rosenblum, Michael D., Kelly A. Remedios, and Abul K. Abbas. "Mechanisms of human autoimmunity." The Journal of Clinical Investigation, Vol. 125, No. 6, 2015, pp. 2228-33.
- Vieira Borba, Vânia, Kassem Sharif, and Yehuda Shoenfeld. "Breastfeeding and autoimmunity: Programing health from the beginning." American Journal of Reproductive Immunology, Vol. 79, No. 1, 2018, p. e12778.
- Plaza-Díaz, Julio, Luis Fontana, and Angel Gil. "Human milk oligosaccharides and immune system development." Nutrients, Vol. 10, No. 8, 2018, pp. 1038.
- Scott, David L., Frederick Wolfe, and Tom WJ Huizinga. "Rheumatoid arthritis." Lancet (London, England), Vol. 376, No. 9746, 2010, pp. 1094-108.
- Albishri, Jamal, et al. "Prevalence of RA and SLE in Saudi Arabia." Scholars Journal of Applied Medical Sciences, Vol. 3, Vol. 5, 2015, pp. 2096-99.
- Xu, Luyi, et al. "Systematic review with meta‐analysis: Breastfeeding and the risk of Crohn's disease and ulcerative colitis." Alimentary Pharmacology & Therapeutics, Vol. 46, No. 9, 2017 780-89.
- Feuerstein, Joseph D., and Adam S. Cheifetz. "Crohn disease: Epidemiology, diagnosis, and management." Mayo Clinic Proceedings, Vol. 92, No. 7, 2017, pp. 1088-103.
- Rosen, Michael J., Ashish Dhawan, and Shehzad A. Saeed. "Inflammatory bowel disease in children and adolescents." JAMA Pediatrics, Vol. 169, No. 11, 2015, pp. 1053-60.
- Farhi, David, et al. "Significance of erythema nodosum and pyoderma gangrenosum in inflammatory bowel diseases: A cohort study of 2402 patients." Medicine, Vol. 87, No. 5, 2008, pp. 281-93.
- Puechal, Xavier, et al. "Peripheral neuropathy with necrotizing vasculitis in rheumatoid arthritis." Arthritis & Rheumatism: Official Journal of the American College of Rheumatology, Vol. 38, No. 11, 1995, pp. 1618-29.
- World Health Organization. "Global strategy for infant and young child feeding." World Health Organization, 2003.
- UNICEF. "Infant and young child feeding" https://data.unicef.org/topic/nutrition/infant-and-young-child-feeding/
- World Health Organization. "Breastfeeding" https://www.who.int/health-topics/breastfeeding#tab=tab_1
- Sullivan, Kevin M., Andrew Dean, and Minn Minn Soe. "On academics: OpenEpi: A web-based epidemiologic and statistical calculator for public health." Public Health Reports, Vol. 124, No. 3, 2009, pp. 471-74.
- Dean AG, Sullivan KM, Soe MM. "OpenEpi: Open source epidemiologic statistics for public health." 2013. http://openepi.com/Menu/OE_Menu.htm
- Al-Nuaimi, Nisreen, Godfrey Katende, and Judie Arulappan. "Breastfeeding trends and determinants: Implications and recommendations for gulf cooperation council countries." Sultan Qaboos University Medical Journal, Vol. 17, No. 2, 2017, pp. e155-61.
- Raheel, Hafsa, and Shabana Tharkar. "Why mothers are not exclusively breast feeding their babies till 6 months of age? Knowledge and practices data from two large cities of the Kingdom of Saudi Arabia." Sudanese Journal of Paediatrics, Vol. 18, No. 1, 2018, pp. 28-38.
- Chen, Haiyan, et al. "Breastfeeding and risk of rheumatoid arthritis: A systematic review and metaanalysis." The Journal of Rheumatology, Vol. 42, No. 9, 2015, pp. 1563-69.
- Kindgren, Erik, Mats Fredrikson, and Johnny Ludvigsson. "Early feeding and risk of juvenile idiopathic arthritis: A case control study in a prospective birth cohort." Pediatric Rheumatology, Vol. 15, No. 1, 2017, pp. 1-9.
- Barclay, Andrew R., et al. "Systematic review: The role of breastfeeding in the development of pediatric inflammatory bowel disease." The Journal of Pediatrics, Vol. 155, No. 3, 2009, pp. 421-26.
- Strisciuglio, Caterina, et al. "Impact of environmental and familial factors in a cohort of pediatric patients with inflammatory bowel disease." Journal of Pediatric Gastroenterology and Nutrition, Vol. 64, No. 4, 2017, pp. 569-74.
- Gungor, Darcy, et al. "Infant milk-feeding practices and cardiovascular disease outcomes in offspring: A systematic review." The American Journal of Clinical Nutrition, Vol. 109, No. Supplement_1, 2019, pp. 800S-16S.
- Rocha, Francisco Airton Castro, et al. "Long-term breastfeeding influences disease activity in a low-income juvenile idiopathic arthritis cohort." Clinical Rheumatology, Vol. 38, No. 8, 2019, pp. 2227-31.