Special Issue - International Journal of Medical Research & Health Sciences ( 2021) Volume 0, Issue 0
Optimizing return to play after anterior cruciate ligament reconstruction in soccer players: An evidence based approach
Florian Forelli1,2,3*, Clement Sansonnet1,3, Steeve Chiapolini3, Jean Mazeas1,2, Amaury Vandebrouck2, Pascal Duffiet2, Louis Ratte2 and Maude Traulle1,22Ramsay sante, Clinic of Domont, 85 route de Domont, Domont, France
3CDFAS, High performance sports medical center, 64, Rue des Bouquinvilles, Eaubonne, France
Florian Forelli, CDFAS, High performance sports medical center, 64, Rue des Bouquinvilles, Eaubonne, France, Tel: 01 34 27 28 50, Email: fforelli@capio.fr
Received: 04-Mar-2021 Accepted Date: Mar 19, 2021 ; Published: 29-Mar-2021, DOI: 0
Abstract
Background: Anterior Cruciate Ligament (ACL) tear is currently a main issue in all of sports communities. Although the number of ACL injuries in football remains low, it’s consequences on both professional and personal lives remain a major concern of rehabilitation.
Methods: If practitioners often require more time to bring athletes in the best condition, the fact remains that this concept of time before return to sport is nowadays considered as obsolete. Indeed, the better understanding of the mechanisms of lesion and the strains placed on the graft after reconstruction, allow us to establish a personalized program based on clinical criteria and the patient's objectives.
Results: The current scientific literature allows us today to optimize the return to play and performance by the use of neuromotor and neurocognitive approaches, muscle strengthening methods and a preventive program necessary to recover the previous level of the players while taking into account physiological and psychological changes due to ACL reconstruction. Indeed, it is important to have a systemic approach centered on the patient, the sports movement, as close as possible to the field in order to find an optimal function of the knee in interaction with its environment.
Conclusion: In order to reduce risk of reinjury and allow best performance for the player, it appears important to be able to identify the risk factors so that the player can return to play in optimal conditions.
Keywords
Injury mechanism, Muscle strengthening, Neuromotor, Neurocognitive, Injury prevention
Abbreviations
ACL : Anterior Cruciate Ligament; BFR: Blood Flow Restriction; CKC: Closed Kinetic Chain; NHE: Nordic Hamstring Exercises; OKC: Opened Kinetic Chain; H/Q: Hamstrings/Quadriceps
Introduction
The return to play after ACL reconstruction is the major goal of rehabilitation. According to several studies, ACL rupture accounts for 6%-14% [1,2] of injuries related to football, however this injury keeps the athlete away from the field for many months with significant social and economic impact associated with both physiological and psychological both which must be taken into account.
Walden et al. admits a prevalence of 0.309 per 1000 hours of play and 0.013 per 1000 hours of training [3]. These Figures show that ACL tear is only a small part of the injuries sustained by the musculoskeletal system in football but its repercussions and modifications mentioned above and the risk of re injury push therapists to adopt optimal rehabilitation strategies in order to overcome a new injury and complications as well as reduce time before return to play. In fact, the young athlete seems to be exposed to a considerable extent to relapse with a risk of recurrence of 25% [4,5].
In order to optimize the return to play for footballers, it seems necessary to understand the mechanisms, the loads applied to the graft and the associated physiological modifications.
Injury Mechanisms
In a research published by Villa et al. [6], several injury mechanisms appear linked to playing football. This parameter is important as it sets the starting point of the lesion and therefore the start of the physiological and psychological modifications that the footballer will undergo in his treatment path towards the resumption of play.
12% of injuries occur through direct contact, when the footballer tackles or gets tackled. In this type of mechanism, we find 81% of direct impact on the knee in a valgus position with the foot fixed to the ground. The remainder of the lesions occurring during a direct impact on the hyperextended knee. Della Villa et al. [6] found in this situation 56% lesions in the defensive phase and 44% in the offensive phase. However, despite these interesting Figures, this type of mechanism does not constitute the situations most often found in football during an ACL injury. The mechanisms responsible for most ACL injuries in football appear to be indirect contact (44%) and non-contact (44%). Indirect contact results from a shock between 2 players that doesn’t involve contact of the injured knee. Thus, the player causing the injury can pull the arm of the player undergoing contact or during a physical shock. This extrinsic destabilization causes a biomechanical disturbance in the lower limb leading to an ACL injury. This type of mechanism happens both on the offensive and on the defensive phase.
Non-contact, however, seems to be the most interesting mechanism, since it involves understanding how a player can suffer an ACL injury alone and without any contact with another player. This is the most typical type of injury in football and is usually the result of a biomechanical disturbance that results from a major interaction with the environment.
Two parameters seem important to take into account: Biomechanical disturbance and neurocognitive disturbance. Indeed, the biomechanical disturbance is noticed by an ipsilateral inclination and contralateral rotation of the trunk, an abducting hip, a dynamic valgus of the knee and a lateral rotation of the foot flattening on the ground. The neurocognitive disturbance occurs between 200 ms and 400 ms before the foot makes contact with the ground. Associated with the biomechanical disturbance, the brain then makes a decision that is unsuitable for the situation and the environment, creating an ACL injury in footballers.
Thus, we can summarize by saying that 56% of ACL lesions occur during contact (direct or indirect) and 88% occur without contact at the knee [6].
When do ACL Injuries Happen?
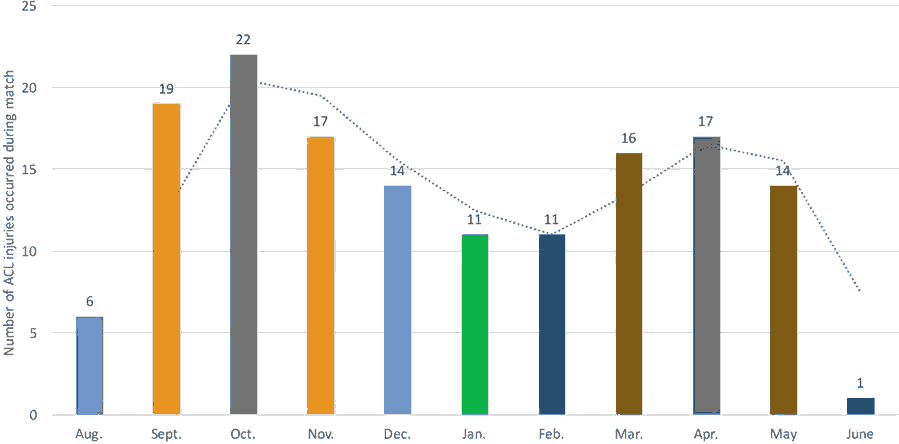
Much controversy exists over the reasons and times of occurrence of ACL. The scientific literature helps us better understand the risk periods for ACL lesions. Thus, Villa et al. retrospectively list the time to onset of ACL lesions during a match and during a season [6]. Thus, during a match, most ACL injuries occur during the first period and especially the first 15 minutes. This confirms the work of Bourne [7] in which he excludes muscle fatigue as a risk factor for ACL injury. Indeed, Villa et al. reports in total that 66.6% of injuries occur during the first period and only 33.4% during the second period of play (Figure 1). Muscle fatigue cannot therefore be an element to consider during an ACL injury, unlike the neurocognitive disturbance that can occur at any time during a match [6,7].
Likewise, if we study the occurrence of ACL lesions over the course of a season, we can notice that ACL ruptures occur at the start of the season (September and October) when the weather conditions are good and the terrain under optimal conditions (Figure 2) [6]. This calls into question the dogmas that ACL lesions occur on slippery, wet ground in cold weather. Likewise, as Howard points out, there is no significant difference between the risks of injury on artificial or natural grass [8].
Delay-Based Rehabilitation
Classically, rehabilitation after ACL reconstruction begins early with analytical work between D0 and D45 with the recovery of joint amplitudes and muscle awakening. Then comes the functional side between D45 and D90 with closed kinetic chain muscular work and obtaining good muscular control.
Between D90 and D120, sports rehabilitation begins with the return to running. However, this period remains unclear about rehabilitation, it focuses on the continuation of muscle strengthening and rehabilitation coach driving without protocol specific. The last stage focuses on the return to sport with a non-contact phase at first and non- contact in a second time.
However, this type of standardized rehabilitation does not take into account the specificities linked to a sport such as football but above all does not acknowledge the uniqueness of the patient. Today, and with the knowledge of recent data in the literature, the clinical aspect seems the most interesting in order to optimize the return to competition. It seems necessary to be based on the progress of the patient and his goals in order to optimize rehabilitation and return to the field in optimal conditions.
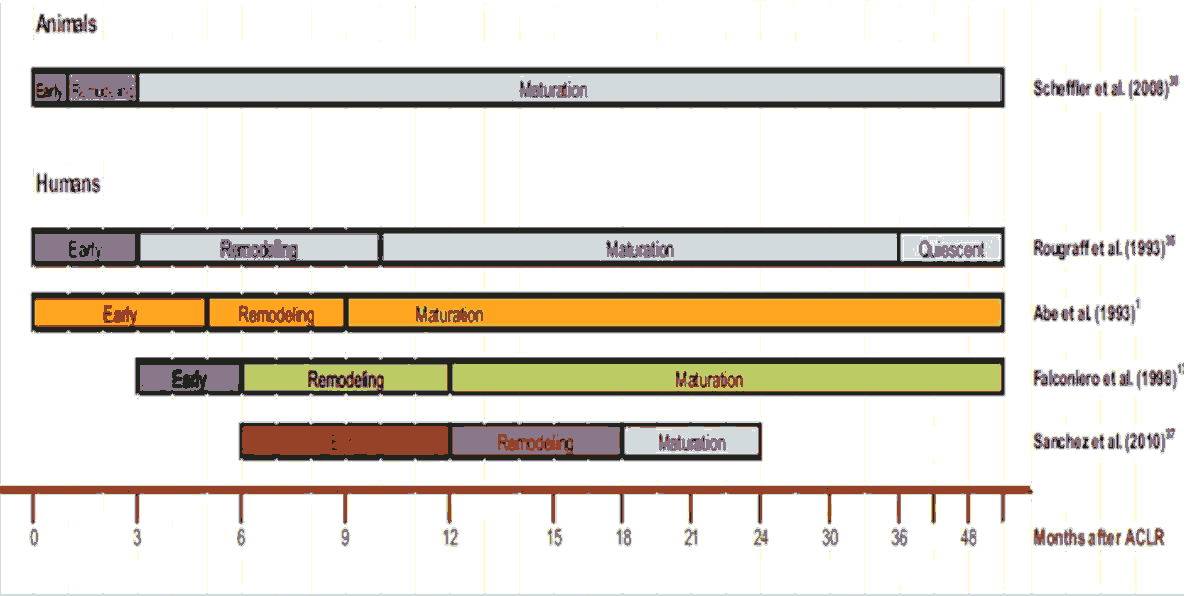
The Ligamentization and Constraints
The scientific literature agrees that the graft undergoes physiological modifications in order to acquire the mechanical strength of a healthy ACL. It is on this basis of ligamentization process that rehabilitation saw its progress over time. However, many authors who have thought about the question cannot find a consensus on the duration of the ligamentization phases (Figure 3) [9]. Thus, without any scientific consensus achieved, it seems today impossible to base oneself on this type of criterion for the progression of rehabilitation and the resumption of sport in football and in sport in general.
Likewise, due to this ligamentization, many illogisms are created in rehabilitation. We then considered the graft fragile from 3 months; however we allowed the resumption of the race and muscle strengthening in OKC which are supposed to apply to the graft the greatest stress.
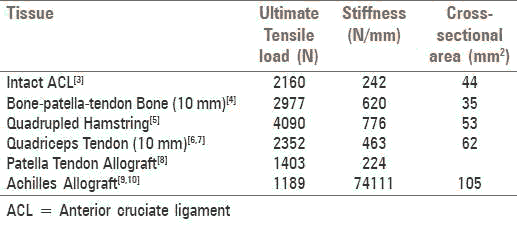
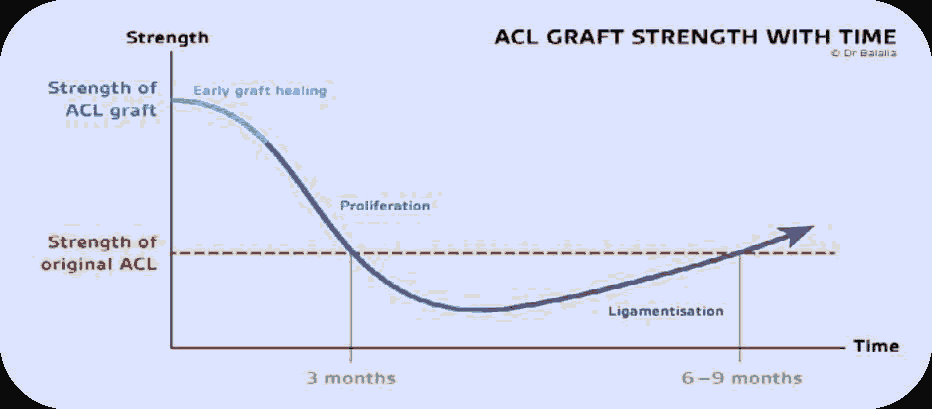
However, when we study the work of Ranjan et al. Balla la and Jansen et al. [10-12], we can realize that the graft becomes more “fragile” at the 3-month stage but that it is nonetheless "solid". In fact, when we observe the work of Ranjan [10], the primary strength of the graft allows progressive stressing in order to ensure its mechanization while relying on the patient's clinic (Figure 4). Likewise, Ballala [11], shows that the strength of the graft during its most “fragile” phase corresponds to 50% of the initial resistance of a healthy ACL, i.e. 1000 N (Figure 5). This allows us to perform a number of exercises aimed at optimizing the patient's rehabilitation.
In addition, the biomechanical studies of Escamilla et al. Taylor et al. and Beynnon et al. [13-15] show that equivalent stresses on the ACL during a Lachmann test, a squat and a dynamic extension of the knee against resistance corresponded to a 3.8% elongation of the graft when walking causes 14% [14]. This confirms the recent work of Noheren et al. and Belloir et al. [16,17] on the non-hazardous aspect of ORC if it is applied with reasoning.
Rehabilitation in Phases
As we mentioned previously, optimization seems to have gone through the clinical progress of the patient and not through a time delay which can waste time for some in the ability to return to sport and competition.
Hughes and Cooper [18] therefore draw from the international scientific literature in order to develop objective criteria for rehabilitation and evaluation to optimize the rehabilitation of patients with ACL reconstruction.
• Phase 1: Recovery from surgery with the important objectives of recovering full extension, fighting against inflammatory phenomena and muscle awakening of the quadriceps
• Phase 2: Neuromuscular Strength and Control with the main objectives of unipodal balance, peripheral muscle strength at the knee and dynamic control of the knee (unipodal squat)
• Phase 3: Race, Agility and Landing
• Phase 4: Return to sport
• Phase 5: Prevention of iterative injury
The progression and the upgrade from one phase to another are conditioned by objective clinical elements and allow an appropriate follow-up with the objective of the return to play, in particular among footballers.
However, in order to optimize the return to competition of footballers as much as possible, we can go further and imagine that the phases can be concomitant with each other. Thus, the therapist can adapt the exercises to his patient in a reasoned way and in connection with the scientific literature in order to allow a return to optimal competition.
For example, including a cardiovascular reconditioning program in an athlete’s early rehabilitation may improve progress throughout the difference stages, as well as keep the athlete himself more engaged in his own rehabilitation.
Inclusion of OKC
Muscle strength is always a primary goal after ACL reconstruction. Thus, as soon as full extension is reached, OKC exercises can complement the CKC exercises as suggested by the work of Jewiss et al. [19]. Noehren et al. [16] suggest that it is necessary to apply a resistance equivalent to 60% of the RM with a fast concentric phase and a slow eccentric phase. Likewise, the early inclusion of isokinetic strengthening can be of tremendous benefit in building muscle. Although sometimes considered aggressive for the graft, the work of Belloir et al. [17] shows that open isokinetic training has no negative effect on the graft’s distension and could even act as a protective factor of the graft during muscle strengthening.
Role of BFR
The BFR is both a tool and a method of rehabilitation that aims to partially restrict the arterial flow and completely restrict venous flow during the exercise muscle [20]. Muscular atrophy and loss of muscle strength are postoperative consequences after ACL reconstruction [21]. These muscle deficits persist several months after operation thus slowing down the progress and optimization of the return to competition and performance for the athlete [22]. These innovative approaches in the early management of postoperative consequences helps fight against these consequences and may help restore knee function [23].
The met analysis of Hughes et al. in 2017 [24] concluded that low-load BFR (30% of Maximum Resistance) may provide an effective approach to early strength and hypertrophy training in individuals who do not tolerate rehabilitation at high load. It therefore helps to develop these muscular qualities just a few days after the operation. They observe similar benefits to high load work with regard to hypertrophy while minimizing joint and tissue stress [25].
Optimize Proximal Control
As we have seen previously, the trunk plays a major role in ACL injury. It appears important to be able to take this parameter into account during rehabilitation. As Dischiavi et al. [26], this is an essential step towards a correct return to performance. Muscle strengthening and proprioceptive exercises focused on the trunk and the placement of the knee in its environment should be undertaken early. The aim is to control the dynamic valgus of the knee during a movement specific to football or another sport. Likewise, programs to strengthen the trunk and hips by strengthening the muscles responsible for the hip abductor moment appear to improve performance during jumps and are an important component of dynamic control of the lower limb [27].
Neurocognitive and Neuromotor
Recent scientific literature highlights the neurocognitive disorders associated with ACL injury. Thus, if the work of Burland et al. [28] speaks of the physiological modifications acquired by reconstruction of the ACL, Linard et al. [29] highlights a disturbance of the balance and a significant visual dependence after reconstruction of the ACL from the earlier phases of rehabilitation. Other studies corroborate these results and highlight alterations in the quality of movement which can be detrimental for the return to competition [30-33]. Therefore, exercises with strobe glasses and/or exercises based on a knee control with external focus seem most effective to recover optimal knee function [33-37].
Sport-Specific Movements and on Field Rehabilitation
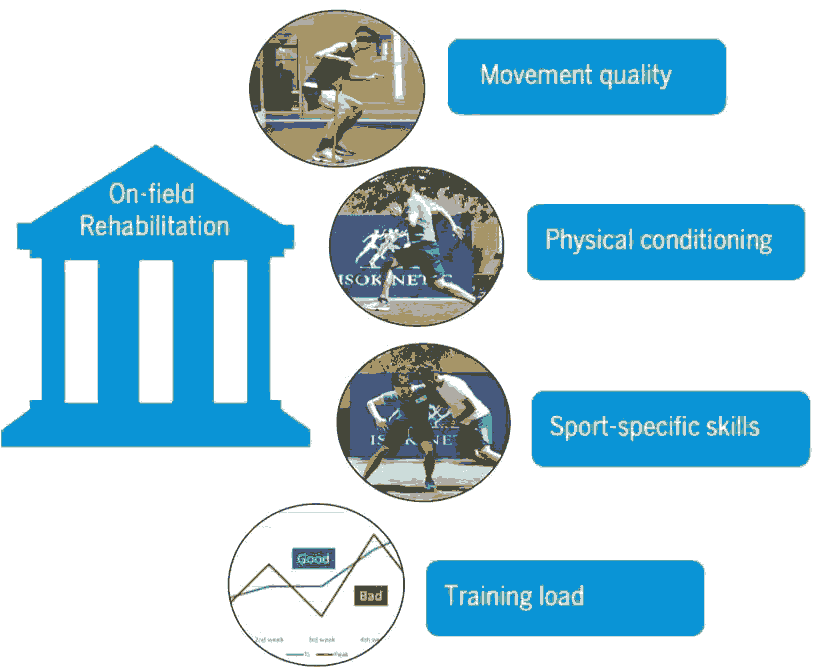
One of the main causes of non-return to sport is movement alterations associated with fear [38,39]. Therefore Bukthorpe et al proposes a design based on four pillars to optimize the rehabilitation of patients: quality of movement, specific movements in sports, physical condition and progressive physical training (Figure 6) [40]. In another article, he reveals 5 stages to work on with an emphasis on changes of direction and football-related skills [41]. Thus, it seems interesting in rehabilitation to work on the movements inherent in football and if possible on field. As a result, the gesture is reintegrated, trained and makes it possible to optimize the return to competition.
Depending on the clinical assessment of the patient, it seems relevant to rework in an appropriate way contact situations, passes, shoots while focusing on the position of the knee during specific movements on the ground. Similarly, this type of work could make it possible to reduce apprehension when resuming competition and thus avoid a sudden transition from rehabilitation to the field.
Prevention
If the prevention programs for injuries have proved their worth in football with the FIFA 11+ program for example, the fact remains that in order to prevent ACL injuries it seems insufficient. As reported by the study by Silvers- Granelli et al. there is no significant difference between a FIFA 11+group and a control group either in terms of positioning on the posture and the placement of the limb in action [42]. However, in a study by Séquier et al, our attention is focused on another type of injury well known to football players: hamstring injury [43]. Indeed, as shown in this study, the muscle activity of the biceps femoris appears to be significantly increased after ACL reconstruction. This is an important note because the biceps femoris remains the most affected during hamstring injuries [44]. Thus, in football, a strong provider of hamstring injuries, it would then be necessary to work on the prevention of this type of injury especially after ACL reconstruction.
To date, there is no therapeutic consensus on the implementation of a hamstring injury prevention protocol. Nevertheless, the study by Mendiguchia et al. shows that a prevention protocol focused on high speed training and sprinting gives more effective results in terms of performance than simple eccentric reinforcement [45]. However, according to Bukthorpe et al. this type of injury being multifactorial, it is necessary to work on other aspects such as obtaining a good Hamstring/Quadriceps strength ratio, intermuscular coordination, hamstring flexibility as well as lumbopelvic stability [46]. However, it seems interesting to us to also work on exercises such as the Nordic Hamstring (NHE), as it has been shown to reduce the risk of hamstring injury by 65%-70%, while noting that only 11% of elite football clubs adopt a training or prevention program including NHE.
Conclusion
The rehabilitation of footballers after ACL reconstruction aims to take several parameters into account. Indeed, the injury mechanisms are the basis of any treatment in order to identify the biomechanical and neurocognitive disturbances affecting the player, which could lead to lack of performance or re-injury. Thus, the therapeutic strategy put in place must ensure that these parameters are taken into account in order to optimize the return to competition by integrating the specific movements and the environment linked to the player and his sport. Therapists must also respect the stages of progression in order to avoid the appearance of any possible complications. Optimization of rehabilitation should lead to a return to competition in optimal conditions but also to reduce the risk factors for recurrence. Finally, each therapist should make his patient evolve on objective criteria of progression as well as objective criteria to resume running and return to sport.
References
- Tamalet, B., Rochcongar, P. “Epidemiology and prevention of anterior cruciate ligament rupture of the knee.” Rev Rum Monogr 83.2 (2016): 103-107.
- Gilchrist, Julie., et al. “A randomized controlled trial to prevent noncontact anterior cruciate ligament injury in female collegiate soccer players.” Am J Sports Med 36.8 (2008): 1476-1483.
- Waldén, Markus., et al. “ACL injuries in men's professional football: a 15-year prospective study on time trends and return-to-play rates reveals only 65% of players still play at the top level 3 years after ACL breaking.” Br J Sports Med 50.12 (2016): 744-750.
- Toole, Allison., et al. “Young athletes after anterior cruciate ligament reconstruction cleared for sports participation: How many actually meet recommended return-to-sport criteria cutoffs?” J Orthop Sports Phys Ther 47.11 (2017): 1-27.
- Wiggins J, Amelia., et al. “Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis.” Am J Sports Med 44.7 (2016): 1861-1876.
- Della Villa, Francesco., et al. “Systematic video analysis of ACL injuries in professional male football (soccer): injury mechanisms, situational patterns and biomechanics study on 134 consecutive cases.” Br J Sports Med 54 (2020): 1423-1432.
- Bourne N, Matthew., Webster E, Kate., and Hewett E, Timothy. “Is fatigue a risk factor for anterior cruciate ligament rupture?” Sports Med 49.11 (2019): 1629-1635.
- Howard, Mark., et al. “Epidemiology of anterior cruciate ligament injury on natural grass versus artificial turf in soccer: 10-year data from the national collegiate athletic association injury surveillance system.” Orthop J Sports Med 8.7 (2020).
- Claes, Steven., et al. “The ligamentization process in anterior cruciate ligament reconstruction: what happens to the human graft: A systematic review of the literature.” Am J Sports Med 39.11 (2011): 2476-2483.
- Rahul, Ranjan., and Naiyer, Asif. “Choices of graft for anterior cruciate ligament reconstruction.” Saudi J Sports Med 16.1 (2016): 7-14.
- Janssen, Rob P., and Scheffler, Sven U. “Intra-articular remodeling of hamstring tendon grafts after anterior cruciate ligament reconstruction.” Knee Surg Sports Traumatol Arthrosc 22.9 (2014): 2102-2108.
- Escamilla, Rafael F., et al. “Anterior cruciate ligament strain and tensile forces for weight-bearing and non- weight-exercises bearing: A guide to exercise selection.” J Orthop Sports Phys Ther 42.3 (2012): 208-220.
- Taylor, KA., et al. “In vivo measurement of ACL length and relative strain during walking.” J Biomech 46.3 (2013): 478-483.
- Beynnon, BD., and Fleming, BC. “Anterior cruciate ligament strain in-vivo: A review of previous work.” J Biomech 31.6 (1998): 519-525.
- Noehren, Brian., and Snyder- Mackler, Lynn. “Who's afraid of the big bad wolf? Open-chain exercises after anterior cruciate ligament reconstruction.” J Orthop Sports Phys Ther 50.9 (2020): 473-475.
- Belloir, Morgan., et al. “Influence of the open kinetic chain on the distension of the graft after anterior cruciate ligament surgery with hamstring graft: Search for risk factors.” Preprints 7.6 (2020).
- Jewiss, Daniel., Ostman, Cecilia and Smart, Neil. “Open vs closed kinetic chain exercises following an anterior cruciate ligament reconstruction: a systematic review and meta-analysis.” J Sports Med 2017 (2017): 4721548.
- Scott, BR., et al. “Exercise with blood flow restriction: An updated evidence-based approach for enhanced muscular development.” Sports Med 45.3 (2015): 313-325.
- Grapar, Žargi T., et al. “Factors predicting quadriceps femoris muscle atrophy during the first 12 weeks following anterior cruciate ligament reconstruction.” Knee 24.2 (2017): 319-328.
- Kılınç, Bekir Eray., et al. “Isokinetic dynamometer evaluation of the effects of early thigh diameter difference on thigh muscle strength in patients undergoing anterior cruciate ligament reconstruction with hamstring tendon graft.” J Exerc Rehabil 11.2 (2015): 95-100.
- Yudai, Takarada., Yoshiaki, Sato and Naokata, Ishii. “Effects of resistance exercise combined with vascular occlusion on muscle function in athlete.” Eur J Appl Physiol 86.4 (2002): 308-314.
- Hughes, Luke., et al. “Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis.” Br J Sports Med 51.13 (2017): 1003-1011.
- Hughes, Luke., et al. “Comparing the effectiveness of blood flow restriction and traditional heavy load resistance training in the post-surgery rehabilitation of anterior cruciate ligament reconstruction patients: A UK national health service randomized controlled trial.” Sports Med 49.11 (2019): 1787-1805.
- Dischiavi, Steven L., et al. “Framework for optimizing ACL rehabilitation utilizing a global systems approach.” Int J Sports Phys Ther 15.3 (2020): 478-485.
- Ferri-Caruana, Ana., Prades-Insa, Beatriz and Serra-Añó, Pilar.“Effects of pelvic and core strength training on biomechanical risk factors for anterior cruciate ligament injuries.” J Sports Med Phys Fitness 60.8 (2020): 1128-1136.
- Burland, Julie P., et al. “Examining the relationship between neuroplasticity and learned helplessness after ACLR: Early vs late recovery.” J Sport Rehabil (2020): 1-8.
- Marc, Linard., et al. “Influence of anterior cruciate ligament surgery with semitendinous and gracilis graft on static postural balance at 3 months postoperatively: randomized controlled study.” Int J Physiother 6.6 (2019): 256-262.
- Gokeler, Alli., et al. “Principles of motor learning to support neuroplasticity after acl injury: implications for optimizing performance and reducing risk of second acl injury.” Sports Med 49.6 (2019): 853-865.
- Neto, T., et al. “Functional brain plasticity associated with ACL injury: A scoping review of current evidence.” Neural Plast 2019 (2019): 1-18.
- Kakavas, George., et al. “Neuroplasticity and anterior cruciate ligament injury.” Indian J Orthop 54.3 (2020): 275-280.
- Faltus, John., et al. “Shifting focus: A clinician's guide to understanding neuroplasticity for anterior cruciate ligament rehabilitation.” Curr Sports Med Rep 19.2 (2020): 76-83.
- Gokeler, Alli., et al. “The effects of attentional focus on jump performance and knee joint kinematics in patients after ACL reconstruction.” Phys Ther Sport 16.2 (2015): 114-20.
- Gokeler, Alli., et al. “Feedback techniques to target functional deficits following anterior cruciate ligament reconstruction: implications for motor control and reduction of second injury risk.” Sports Med 43.11(2013): 1065-1074.
- Gokeler, Alli., et al. “Clinical course and recommendations for patients after anterior cruciate ligament injury and subsequent reconstruction: A narrative review.” EFORT Open Rev 2.10 (2017): 410-420.
- Benjaminse, Anne., et al. “Optimization of the anterior cruciate ligament injury prevention paradigm: novel feedback techniques to enhance motor learning and reduce injury risk.” J Orthop Sports Phys Ther 45.3 (2015): 170-182.
- Lee, Dave Y., Sarina, Abdul Karim and Chang, Chang Haw. “Return to sports after anterior cruciate ligament reconstruction - a review of patients with minimum 5-year follow-up.” Ann Acad Med Singap 37.4 (2008): 273-278.
- Kvist, Joanna., et al. “Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction.” Knee Surg Sports Traumatol Arthrosc 13.5 (2005): 393-397.
- Buckthorpe, Matthew., et al. “On-field rehabilitation part 1: 4 pillars of high-quality on-field rehabilitation are restoring movement quality, physical conditioning, restoring sport-specific skills, and progressively developing chronic training load.” J Orthop Sports Phys Ther 49.8 (2019): 565-569.
- Buckthorpe, Matthew., et al. “On-field rehabilitation part 2: A 5-stage program for the soccer player focused on linear movements, multidirectional movements, soccer-specific skills, soccer-specific movements, and modified practice.” J Orthop Sports Phys Ther 49.8 (2019): 570-575.
- Silvers- Granelli, Holly J., et al. “Does the FIFA 11+ injury prevention program reduce the incidence of ACL injury in male soccer players?.” Clin Orthop Relat Res Oct 475.10 (2017): 2447-2455.
- Crema, Michel D., et al. “Acute hamstring injury in football players: Association between anatomical location and extent of injury-A large single-center MRI report.” J Sci Med Sport 19.4 (2016): 317-322.
- Mendiguchia, Jurdan., et al. “Sprint versus isolated eccentric training: Comparative effects on hamstring architecture and performance in soccer players.” PLoS One 15.2 (2020): 1-19.
- Buckthorpe, Matthew., et al. “Recommendations for hamstring injury prevention in elite football: translating research into practice.” Br J Sports Med 53.7 (2019): 449-456.
- Goode, Adam, P., et al. “Eccentric training for prevention of hamstring injuries may depend on intervention compliance: a systematic review and meta-analysis.” Br J Sports Med 49.6 (2015): 349-356.
- Petersen, Jesper., et al. “Preventive effect of eccentric training on acute hamstring injuries in men's soccer: a cluster-randomized controlled trial.” Am J Sports Med 39.11 (2011): 2296-2303.
- Bahr, Roald., Thorborg, Kristian and Ekstrand, Jan. “Evidence-based hamstring injury prevention is not adopted by the majority of champions league or norwegian premier league football teams: The nordic hamstring survey.” Br J Sports Med 49.22 (2015): 1466-1471.