Research - International Journal of Medical Research & Health Sciences ( 2021) Volume 10, Issue 7
The Impact of Body Mass Index on Spirometric Parameters of Late Adolescents
Maram Walid1, Aaisha Mohammed1, Sareesh Naduvi1, Narayanan2* and Tarig Hakim Merghani22Department of Physiology, RAK College of Medical Sciences, RAK Medical and Health Sciences University, Ras Al Khaimah, United Arab Emirates
Narayanan, Department of Physiology, RAK College of Medical Sciences, RAK Medical and Health Sciences University, Ras Al Khaimah, United Arab Emirates, Email: sareeshnn@yahoo.co.in
Received: 02-Jun-2021 Accepted Date: Jul 23, 2021 ; Published: 30-Jul-2021
Abstract
Background: Overweight and obesity prevalence has been increased worldwide creating a true pandemic and it is now affecting younger age groups. Objective: To determine the impact of Body Mass Index (BMI) on pulmonary function of late adolescents. Methods: A cross-sectional study was carried out among 95 late adolescents aged 18 to 22 Years. Participants were categorized into normal weight, overweight and obese groups based on their BMI. Pulmonary function was measured by a digital spirometer (Spirolab, GIMA/ Italy) following the American Thoracic Society guidelines. Results: The lowest FEV1/FVC ratio was found in obese females. The influence of BMI on Forced Vital Capacity (FVC), Forced Expiratory Volume in one second (FEV1), and Peak Expiratory Flow (PEF), in both males and females, was statistically insignificant. The BMI has an insignificant effect on the small airway parameters (FEF 50%, FEF 75%, and FEF 25%-75%) of the two sexes. A significant negative correlation was observed between BMI and FEV1/FVC in both males and females. Furthermore, a significant negative correlation was found between BMI and forced expiratory flow 50% (FEF50%) in males but not in females. Conclusion: A high BMI has an insignificant impact on most of the lung function parameters of adolescents, except for the FEV1/FVC ratio.
Keywords
Body mass index, Obesity, Pulmonary function, Adolescents, Spirometry
Introduction
The Body Mass Index (BMI) is a person’s weight (in kilograms) divided by the square of height (in meters) [1]. A high BMI is an indicator of the increased fat content of the body. The BMI can be used as a screening test for weight categories that are associated with increased morbidity [2]. A recent report documented a high prevalence of obesity and associated non-communicable diseases among the UAE expatriates [3]. It is noticed that overweight and obesity are creating a true pandemic and now affecting younger age groups [4].
The major complications of increased weight include a heightened demand for ventilation, elevated work of breathing, respiratory muscle inefficiency, and diminished respiratory compliance. This is even worse in individuals who are obese [5]. Obesity is a chronic disease characterized by the excessive accumulation of body fat that is harmful to individuals and is also known to increase morbidity and decrease life expectancy in affected subjects [3]. Men with body fat above 25% and women with body fat above 30% are considered obese [6]. Obesity can alter lung function in several ways and the effect does not depend on the degree of obesity alone, it also depends on age and sites of fat distribution. It is reported that, in moderate obese humans, the reduced lung compliance added with the increased inspiratory threshold will elevate the work of breathing by three to four times compared with that in normal-weight individuals [6]. Additionally, decreased pulmonary gas exchange, lower control of breathing with limitations in exercise capacity is associated with the high-fat content in the bodies of obese people [3].
The Pulmonary Function Test (PFT) is one of the important tools for the assessment of pulmonary function [7]. Although the impact of obesity on lung function has been reported in many previous studies, controversies are still present in terms of which respiratory parameters are affected [8,9]. Reports on the relationship between BMI and respiratory parameters of the UAE adolescent population are rare.
Study Point
It is important to identify if there is an association between BMI and respiratory parameters in young adults and which parameter is affected. Results may help in the diagnosis of respiratory diseases in obese patients presenting with atypical lung function results. In this study, the impact of different degrees of body weight, as grouped by BMI, on lung function indicators was evaluated using spirometry.
Methods
A cross-sectional study was carried out among 95 students aged 18 to 22 years old. The study was approved by the institutional Research Ethics Committee (No. REC-041-2018). All the participants gave their informed consent before taking part in the study. A self-administered questionnaire requesting information about age, gender, height, weight, current respiratory symptoms, and past medical history was used for data collection. Participants with respiratory symptoms, chronic medical illness including asthma and COPD, or cigarette smokers were excluded from the study. Standardized weight and height scales were used to measure the weight and height of each participant. The calculated BMI (weight in kg/ height in m2) was used to group the participants into three groups as follows, a) BMI between 18.5 kg/m2-24.9 kg/m2 were included in-Group 1 (Healthy adolescents-Normal), b) Individuals with BMI between 25 kg/m2-29.9 kg/m2 were included in-Group 2 (Overweight) c) Individuals with BMI ≥ 30 kg/m2 were included in- Group 3 (Obese). A digital spirometer (Spirolab, GIMA/Italy) was used for the measurement of lung function of each participant as per the guidelines of the American Thoracic Society (ATS) [10].
The best of three acceptable and reproducible spirometry readings was recorded for each participant. Differences between the groups were determined using the one-way Analysis of Variance test (ANOVA). Post-hoc Tukey Test was used for multiple comparisons. The association between the BMI and the respiratory parameters was determined with Pearson’s correlation. The GraphPad Prism software (version 5.0) was used for analysis. A p-value of less than 0.05 was considered significant.
Results
Demographic Characteristics of the Study Group
A total of 41 participants (18 males and 23 females) had normal BMI between 18.5 kg/m2 and 24.9 kg/m2 and were included in Group 1. Those with higher BMI were classified as overweight or Group 2 (BMI between 25 kg/m2 and 29.9 kg/m2) and obese or Group 3 (BMI ≥ 30 kg/m2). Table 1 shows the mean age, height, weight, and BMI of the three groups.
| Parameters | Males | Females | ||||||
|---|---|---|---|---|---|---|---|---|
| Normal n=18 |
Overweight n=11 |
Obese n=11 |
p-value | Normal n=23 |
Overweight n=16 |
Obese n=16 |
p-value | |
| Age (Years) | 19.89 ± 0.44 | 19.73 ± 0.54 | 20.36 ± 0.47 | ≤ 0.67 | 19.52 ± 0.37 | 18.94 ± 0.44 | 19.31 ± 0.51 | ≤ 0.63 |
| Height (cm) | 165.3 ± 9.45 | 174.8 ± 1.91 | 176.3 ± 1.34 | ≤ 0.50 | 160.4 ± 1.36 | 163.1 ± 0.99 | 159.5 ± 1.18 | ≤ 0.15 |
| Weight (kg) | 65.72 ± 2.38 | 81.73 ± 2.20 | 113.4 ± 7.61* | <0.0001 | 56.39 ± 1.67 | 70.56 ± 1.08 | 93.50 ± 2.68* | <0.0001 |
| BMI (kgm2) | 21.53 ± 0.57 | 26.72 ± 0.50 | 34.41 ± 1.13* | <0.0001 | 21.98 ± 0.46 | 26.54 ± 0.32 | 36.79 ± 1.08* | <0.0001 |
The Impact of BMI on Pulmonary Function
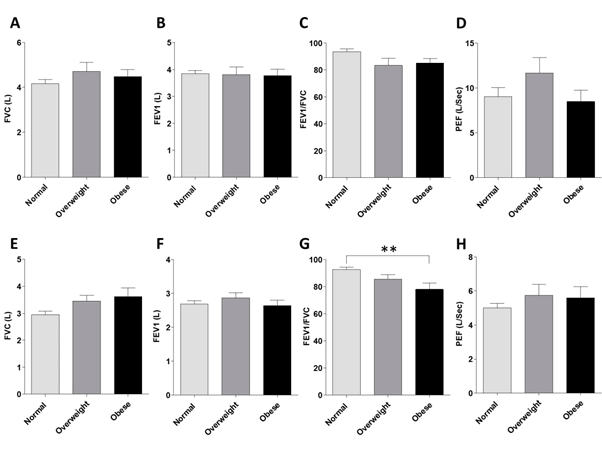
The FVC was 4.16 ± 0.19 L in normal-weight males. However, it was 4.70 ± 0.39 L and 4.48 ± 0.30 L in overweight and obese males, respectively (Figure 1A). In females, the FVC was 2.94 ± 0.12 L, 3.45± 0.21 L, and 3.61 ± 0.32 L in normal, overweight, and obese individuals, respectively (Figure 1E). The differences between the three groups were statistically insignificant.
The recorded FEV1 values were 3.84 ± 0.11 L, 3.80 ± 0.29 L, and 3.76 ± 0.2 4L in normal, overweight, and obese males, respectively (Figure 1B). In females, the three groups showed mean FEV1 values of 2.68 ± 0.09 L, 2.87 ± 0.14 L, and 2.64 ± 0.15 L, respectively (Figure 1F). The one-way ANOVA test revealed an insignificant statistical difference.
The FEV1/FVC% values were 93.52 ± 2.03 in normal-weight males, 83.32 ± 5.49 in the overweight, and 85.17 ± 3.39 in the obese ones (Figure 1C, p>0.05). A significant reduction in the FEV1/FVC% was found in females. The ratio values were reduced from 92.60 ± 1.61 in the normal-weight to 85.38 ± 3.53% in the overweight and 78.02 ± 4.56% in the obese females (Figure 1G, p<0.05).
The PEF did not show any statistically significant difference between the three groups in both males (Figure 1D) and females (Figure 1H).
The Influence of BMI on the Small Airway Parameters
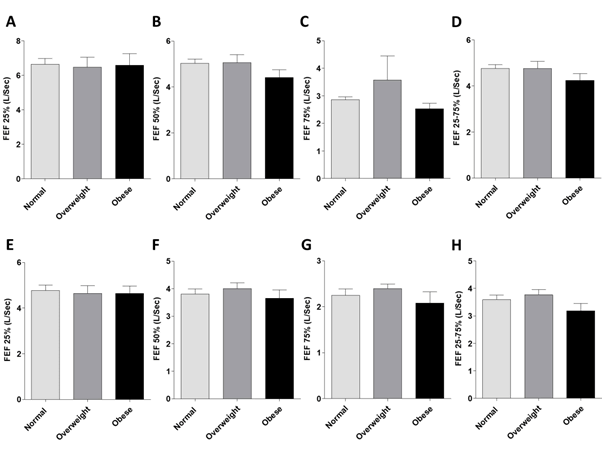
The FEF 25% values across the three groups were found to be the same in both males (Figure 2A) as well as in females (Figure 2E). ANOVA test revealed an insignificant difference in both males and females (p=0.97).
The mean expiratory flow rates (FEF50%) were lower in obese males compared to normal and overweight participants of the same gender (Figure 2B, p=0.21). The same pattern was also observed in the FEF50% of females (Figure 2F, p=0.59) and FEF75% of both males (Figure 2C, p=0.30) and females (Figure 2G, p=0.44).
The FEF 25%-75% reached up to 5L in normal and overweight individuals. However, it was less in obese individuals (Figure 2D, p=0.25). Similarly, in normal or overweight females the FEF-25%-75% value reached nearly 3.75L, but only 3L in obese females (Figure 2H, p=0.15).
Correlation of BMI vs. FVC, FEV1 and FEV1/FVC in Males and Female
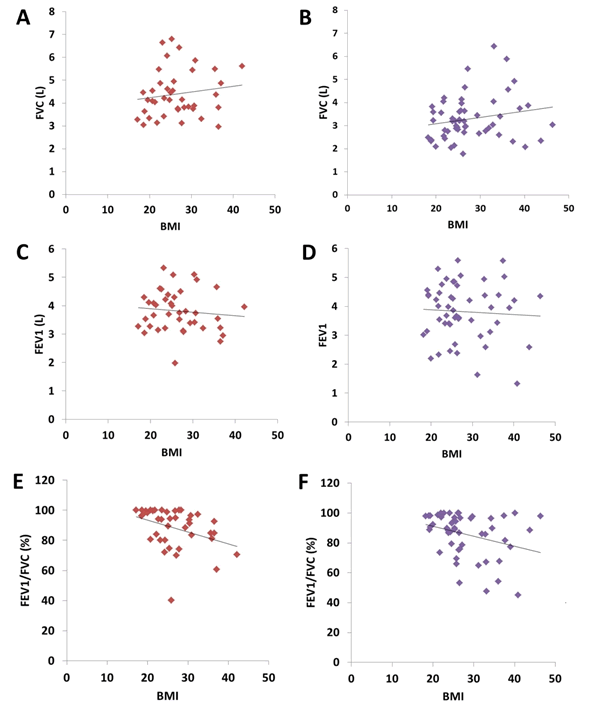
correlation between BMI and FVC shows that as the BMI increases the FVC seems to increase. This pattern was observed to be the same in both males (Figure 3A; r=0.14, p=0.36) and females (Figure 3B; r= -0.19, p=0.14). The relation is statistically insignificant within the BMI range of our participants. In contrast, a correlation between BMI and FEV1 demonstrates a progressive reduction in FEV1 with the increase in BMI. However, this was statistically insignificant in both males (Figure 3C; r= -0.10, p=0.52) and females (Figure 3D; r= -0.08, p=0.56). Nonetheless, a correlation between BMI and FEV1/FVC revealed a strong negative correlation between these parameters. As evident from the results, as the BMI increases, the FEV1/FVC seems to be reduced. This pattern was observed to be the same among males (Figure 3E; r= -0.36, p*= 0.02) and females (Figure 3F; r= -0.31, p*= 0.02).
Correlation of BMI vs. FEF25%, FEF50% and FEF75% in Males and Female
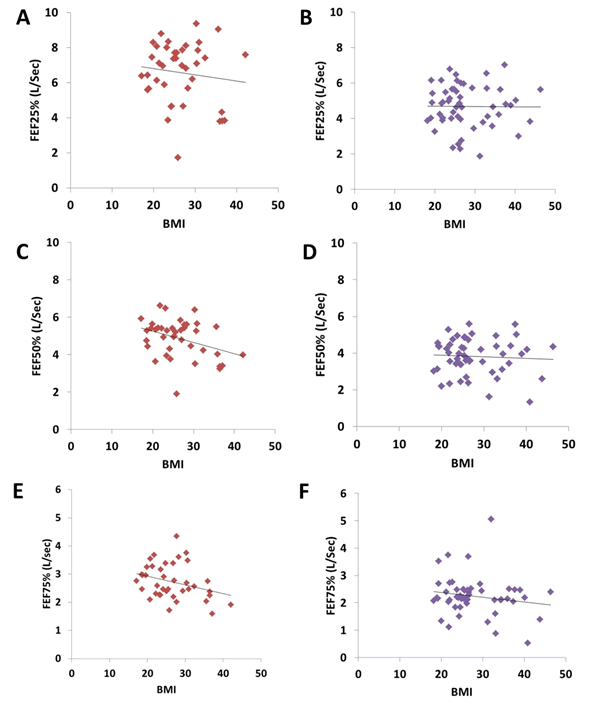
A correlation between BMI and forced expiratory flow parameters (FEF25%, FEF50%, and FEF75%) showed the effect of increasing BMI on the small airways of the lungs. The results showed that as the BMI increases the forced expiratory flow rates decrease. This pattern was significant for FEF50% in males (Figure 4C; r= -0.36, p*=0.02) but insignificant in females (Figure 4D; r= -0.05, p=0.67). Although there was a weak negative correlation observed between BMI and FEF25% in both males (Figure 4A; r= -0.12, p=0.44) and females (Figure 4B; r= -0.007; p=0.95),the correlation was statistically insignificant. The same pattern was observed with BMI and FEF75% correlation in males (Figure 4C; r= -0.14; p=0.37) and females (Figure 4D; r= -0.16, p=0.23).
Discussion
Obesity is a worldwide public health problem and a recognized cause of poor lung function. It causes a reduction in both dynamic and static lung volumes [11,12]. However, insignificant results were also reported [13-15]. The negative impact of increased BMI on the respiratory system can be explained by the direct mechanical effect of fat deposition in the chest wall and abdomen that causes movement restriction of the respiratory muscles [16,17]. Another explanation is the increased production of inflammatory cytokines from the adipose tissue and the associated increase in immune cells that induce structural and inflammatory changes within the small lung airways [16,17].
In this study, we found insignificant effects of obesity on most of the lung ventilatory functions of late adolescents, except for FEV1/FVC values in females. Our findings are similar to a regional study that reported an insignificant difference in lung function indicators between obese and non-obese adults [18]. In that study, the author recommended searching for an alternative explanation, other than obesity, to justify low spirometric values [18]. In another regional study, the reduction in lung function becomes significant only when the effects of obesity are combined with smoking [19]. Moreover, prolonged duration of obesity is required to develop marked obesity-related lung function effects [20]. The short duration of obesity of our participants, being late adolescents with an average age of 19 years old, could explain the absence of significant effects. The early development of obesity during childhood was found to be associated with higher, rather than lower, FEV1 and FVC [21]. Similarly, in the current study, we observed an increased FVC in both overweight and obese individuals with insignificant variations in the FEV1 values between the two groups in either gender. Another important factor that is associated with reduced lung function is the way of fat distribution. Mafort and colleagues claimed that the negative of obesiimpactty on lung function could be associated with the pattern of body fat distribution, whether central or peripheral [17]. They found that the reduced lung function is more likely to be related to central fat distribution in the thorax and abdomen than to peripheral fat distribution in the hips and thighs. The patterns of fat distribution were not examined in the current study.
Obese individuals may develop bronchial hyper-responsiveness and asthma that is characterized by low FEV1/FVC and low Forced Expiratory Flow rates (FEF) as a sign of small airway inflammation [22]. In this study, the correlation between BMI and FEV1/FVC in both males and females showed that the ratio tends to decrease with high BMI. Although the FEV1/FVC ratio of the obese females is significantly lower than that of the other participants, it remains above the value of 0.7 (in most of the cases), which possibly excludes the element of airway obstruction. A gender disparity in lung function impairment with females being affected more than males is a recognized finding [23]. A negative correlation was also found between the BMI and FEV1 and the forced expiratory flow parameters. Although the relationship is statistically insignificant, except for the FEF50, it is expected that morbid obesity with higher BMI values would give significant results. Al-Alwan and colleagues have confirmed the association between obesity and peripheral airway disease, especially among asthmatics [24]. On the other hand, the correlation between BMI and the FVC shows that the FVC seems to increase with obesity. Variable findings were reported in similar age groups [21]. It is worth noting that the hormonal changes during late adolescence and young adulthood are associated with increased growth and changes in body muscle and fat deposition; this could explain the contradictory findings of different studies.
Another interesting aspect that needs to be discussed in this context is the obesity paradox. Multiple epidemiological studies have demonstrated the positive relationship between obesity and mortality, particularly cardiovascular mortality [25,26]. Nonetheless, other studies have found an inverse correlation between Body Mass Index (BMI) and mortality, which is termed the obesity paradox [27,28]. This implies that it could be healthier to be overweight than to be normal or low weight. This concept needs to be discussed in the context of current study results. As depicted in the results, most of the respiratory function parameters in obese/overweight participants were comparable to normal late adolescents. However, further studies are necessary to categorically prove this observation.
A few limitations in this study need to be taken into consideration while extrapolating the results. Since the BMI was used as a measure for obesity evaluation it did not distinguish fat mass and muscle mass of the body, and it cannot determine the pattern of regional fat distribution in the participants. The relatively small sample size and the expected variation in physical activity between the participants are other limitations that should be considered while interpreting the results. In conclusion, our results confirm the previous finding that adolescents’ lung ventilatory function indicators are not significantly affected by overweight and obesity. Another causative factor like smoking or pattern of body fat distribution should be investigated whenever poor lung function is diagnosed in an obese adolescent.
Conclusion
An increased BMI did not significantly influence most of the lung function parameters of adolescents, except for FEV1/FVC values in females. However, in either gender, a trend to have decreased FEV1/FVC values was observed as the BMI increases. Moreover, compromised forced expiratory flow rates were evident as the BMI increases in adolescents, especially in males. Obesity will have a significant influence on respiratory parameters, particularly on female adolescents as they face medical, psychological, and reproductive health challenges during this phase. Therefore, early intervention is very much required to prevent short-term and long-term morbidity.
Declarations
Conflicts of Interest
The authors declared no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
- Nuttall, Frank Q. "Body mass index: Obesity, BMI, and health: A critical review." Nutrition Today, Vol. 50, No. 3, 2015, pp. 117-28.
- Pasco, Julie A., et al. "Body mass index and measures of body fat for defining obesity and underweight: A cross-sectional, population-based study." BMC Obesity, Vol. 1, No. 1, 2014, pp. 1-7.
- Sulaiman, Nabil, et al. "Prevalence of overweight and obesity in United Arab Emirates Expatriates: The UAE national diabetes and lifestyle study." Diabetology & Metabolic Syndrome, Vol. 9, No. 1, 2017, pp. 1-9.
- Prentice, Andrew M. "The emerging epidemic of obesity in developing countries." International Journal of Epidemiology, Vol. 35, No. 1, 2006, pp. 93-99.
- Parameswaran, Krishnan, David C. Todd, and Mark Soth. "Altered respiratory physiology in obesity." Canadian Respiratory Journal, Vol. 13, No. 4, 2006, pp. 203-10.
- Shoukri, Amr. "Effects of obesity on respiratory mechanics at rest and during exercise." Egyptian Journal of Bronchology, Vol. 9, No. 3, 2015, pp. 224-26.
- Ruppel, Gregg L., and Paul L. Enright. "Pulmonary function testing." Respiratory Care, Vol. 57, No. 1, 2012, pp. 165-75.
- Fortis, Spyridon, et al. "The difference between slow and forced vital capacity increases with increasing body mass index: A paradoxical difference in low and normal body mass indices." Respiratory Care, Vol. 60, No. 1, 2015, pp. 113-18.
- Robinson, Paul D. "Obesity and its impact on the respiratory system." Paediatric Respiratory Reviews, Vol. 15, No. 3, 2014, pp. 219-26.
- Miller, M R et al. “Standardisation of spirometry.” The European Respiratory Journal, Vol. 26, No. 2, 2005, pp. 319-38.
- Peralta, Gabriela P., et al. "Body mass index and weight change are associated with adult lung function trajectories: The prospective ECRHS study." Thorax, Vol. 75, No. 4, 2020, pp. 313-20.
- Littleton, Stephen W., and Aiman Tulaimat. "The effects of obesity on lung volumes and oxygenation." Respiratory Medicine, Vol. 124, 2017, pp. 15-20.
- Ceylan, Emel, et al. "The effects of body fat distribution on pulmonary function tests in the overweight and obese." Southern Medical Journal, Vol. 102, No. 1, 2009, pp. 30-35.
- Gabrielsen, Anne-Marie, et al. "The relationship between anthropometric measures, blood gases, and lung function in morbidly obese white subjects." Obesity Surgery, Vol. 21, No. 4, 2011, pp. 485-91.
- Pekkarinen, E., et al. "Relation between body composition, abdominal obesity, and lung function." Clinical Physiology and Functional Imaging, Vol. 32, No. 2, 2012, pp. 83-88.
- Dixon, Anne E., and Ubong Peters. "The effect of obesity on lung function." Expert Review of Respiratory Medicine, Vol. 12, No. 9, 2018, pp. 755-67.
- Mafort, Thiago Thomaz, et al. "Obesity: systemic and pulmonary complications, biochemical abnormalities, and impairment of lung function." Multidisciplinary Respiratory Medicine, Vol. 11, No. 1, 2016, pp. 1-11.
- Al Ghobain, Mohammed. "The effect of obesity on spirometry tests among healthy non-smoking adults." BMC Pulmonary Medicine, Vol. 12, No. 1, 2012, pp. 1-5.
- Al-sayed, B. A., et al. "Early development of pulmonary function impairment in healthy young adults: Impact of obesity and tobacco smoking." Jokull, Vol. 65, No. 6, 2015, pp. 205-14.
- Santamaria, Francesca, et al. "Obesity duration is associated to pulmonary function impairment in obese subjects." Obesity, Vol. 19, No. 8, 2011, pp. 1623-28.
- Forno, Erick, et al. "Overweight, obesity, and lung function in children and adults-A meta-analysis." The Journal of Allergy and Clinical Immunology: In Practice, Vol. 6, No. 2, 2018, pp. 570-81.
- Oppenheimer, Beno W., et al. "Small airway function in obese individuals with self-reported asthma." ERJ Open Research, Vol. 6, No. 2, 2020, pp. 1-10.
- Banerjee, Joyashree, et al. "Association of Body Mass Index (BMI) with lung function parameters in non-asthmatics identified by spirometric protocols." Journal of Clinical and Diagnostic Research: JCDR, Vol. 8, No. 2, 2014, pp. 12-14.
- Al-Alwan, Ali, et al. "The nonallergic asthma of obesity. A matter of distal lung compliance." American Journal of Respiratory and Critical Care Medicine, Vol. 189, No. 12, 2014, pp. 1494-502.
- Peeters, Anna, et al. "Obesity in adulthood and its consequences for life expectancy: A life-table analysis." Annals of Internal Medicine, Vol. 138, No. 1, 2003, pp. 24-32.
- Calle, Eugenia E., et al. "Body-mass index and mortality in a prospective cohort of US adults." New England Journal of Medicine, Vol. 341, No. 15, 1999, pp. 1097-105.
- Oreopoulos, Antigone, et al. "Body mass index and mortality in heart failure: A meta-analysis." American Heart Journal, Vol. 156, No. 1, 2008, pp. 13-22.
- Romero-Corral, Abel, et al. "Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies." The Lancet, Vol. 368, No. 9536, 2006, pp. 666-78.